There is a paucity of data on long-term outcomes after percutaneous coronary intervention (PCI) for chronic total occlusions (CTOs) in the high-risk group of patients with diabetes mellitus (DM). The aim of this study was to evaluate long-term clinical outcomes after PCI of CTOs in patients with and without DM. A total of 1,742 patients with known DM status underwent PCI of CTOs at 3 tertiary care centers in the United States, South Korea, and Italy from 1998 to 2007. Five-year clinical outcomes were evaluated in patients with successful versus failed CTO PCI and the use of drug-eluting stents (DES) versus bare-metal stents (BMS) stratified according to DM status. A total of 395 patients (23%) had DM (42% of whom had insulin-dependent DM). Procedural success was similar in patients with versus without DM (69.6% vs 67.9%, p = 0.53). After successful CTO PCI, stents were implanted in 96.4% of patients with DM (BMS in 23.8%, DES in 76.2%) and in 94.0% of patients without DM (BMS in 38.6%, DES in 61.4%). Median follow-up was 3.0 years. In patients with DM, successful CTO PCI was associated with reduced long-term mortality (10.4% vs 13.0%, p <0.05) and a reduced need for coronary artery bypass grafting (2.4% vs 15.7%, p <0.01). The use of DES was associated with a reduction in target vessel revascularization in patients with DM (14.8% vs 54.1%, p <0.01) and in those without DM (17.6% vs 26.5%, p <0.01). Multivariate analysis identified insulin-dependent DM as an independent predictor of mortality in the DM cohort. In conclusion, successful CTO PCI in patients with DM was associated with a reduction in mortality and the need for coronary artery bypass grafting. Compared to non-insulin-dependent DM, patients with insulin-dependent DM had an increased risk for long-term mortality. The use of DES rather than BMS was associated with a reduction in target vessel revascularization in patients with and without DM.
The prevalence of diabetes mellitus (DM) is increasing in industrialized countries, and it is expected that 1/3 of Americans born in 2000 will develop DM during their lifetimes. Patients with DM have a greater extent of coronary artery disease and are prone to impaired clinical outcomes compared to patients without DM. Chronic total occlusions (CTOs) located in coronary arteries are observed in 15% to 30% of diagnostic coronary angiograms. The prevalence of CTOs is likely to be increased in patients with DM, as suggested by a recent study showing an increased prevalence of CTOs in non-infarct-related arteries in patients with ST-segment elevation myocardial infarction in patients with DM. Successful percutaneous coronary intervention (PCI) of a CTO has been associated with increased survival and a reduction in the need to perform coronary artery bypass grafting. Moreover, drug-eluting stents (DES), compared to bare-metal stents (BMS), are associated with a reduced need for repeat revascularization after CTO PCI, with possibly a slightly increased stent thrombosis risk. Currently, there is a paucity on data regarding clinical outcome of CTO PCI in patients with DM. Therefore, we investigated clinical outcomes after successful and failed CTO PCI in patients with and without DM. Moreover, we analyzed clinical outcomes after successful PCI with BMS versus DES in patients with and without DM.
Methods
The study design of the Multinational CTO Registry has been previously reported. In brief, all patients who underwent PCI for ≥1 CTO at 3 tertiary care hospitals from 1998 to 2007 were included in this study. A CTO was defined as a coronary artery obstruction with a Thrombolysis In Myocardial Infarction (TIMI) flow grade of 0. All patients included had native vessel occlusions estimated to be of ≥3-month duration on the basis of either a history of sudden chest pain, a previous myocardial infarction in the same target vessel territory, or the time between diagnosis made on coronary angiography and PCI. All patients had symptomatic angina and/or positive results on functional ischemia studies.
PCI and stent implantation were performed in a standard manner. Heparin was administered to maintain an activated clotting time >250 seconds. The use of BMS or DES as well as the use of glycoprotein IIb/IIIa inhibitors was left to the discretion of the treating physician. PCI of the CTO was performed using contemporary techniques such as bilateral injection, specialized hydrophilic, tapered tip, and stiff wires, parallel wires, microcatheters, and retrograde approach when they became available.
Demographic, angiographic, and procedural data regarding all patients who underwent PCI at the 3 participating centers were prospectively entered into a dedicated database. Patients were followed prospectively by telephone interview or outpatient visit after 30 days and yearly thereafter. Demographic, angiographic, procedural, and follow-up data were subsequently merged in the Multinational CTO Registry, containing all data contributed by the 3 participating centers. The following end points were evaluated to compare patients with failed versus successful procedures: all-cause mortality, myocardial infarction, and coronary artery bypass grafting. To compare patients treated with DES versus BMS, the following end points were evaluated: the composite clinical end point of major adverse cardiac events (all-cause mortality, myocardial infarction, or target vessel revascularization [TVR]), all-cause mortality, myocardial infarction, TVR, and definite or probable stent thrombosis according to the Academic Research Consortium definitions. The following definitions were used: multivessel disease was defined as the presence of ≥1 stenosis ≥70% by visual assessment in a major epicardial vessel or its side branches other than that where the CTO was located. Procedural success was defined as successful recanalization and dilation of ≥1 CTO per patient with or without stent implantation, residual stenosis of <50%, and TIMI flow grade ≥2.
Data are presented as mean ± SD or as percentages. Event rates were estimated using the Kaplan-Meier method. Follow-up was censored at the date of last follow-up or at 5 years, whichever came first. Survival curves were constructed for time-to-event variables using Kaplan-Meier methods and compared using log-rank tests. Data on patients who were lost to follow-up were censored at the time of the last contact. Cox proportional-hazards methods were used to identify the predictors of all-cause mortality at 5 years in patients with successful versus unsuccessful PCI and TVR at 5 years in patients who underwent successful PCI with BMS versus DES. Separate models were constructed for patients with DM and patients without DM. The multivariate models were built by stepwise variable selection, with entry and exit criteria set at the p = 0.10 level, but procedural success was forced into the model for all-cause mortality, and the use of DES was forced into the model for TVR. The following patient-level candidate predictors were evaluated: age (per year increment), gender, hypercholesterolemia, hypertension, insulin-dependent DM (only in the DM group), smoking, chronic kidney disease, preprocedural left ventricular ejection fraction (per 10%), previous myocardial infarction, multivessel disease, CTO located in the left anterior descending coronary artery, total CTO length (millimeters) and total stent length (millimeters). Statistical analyses were performed using SPSS version 17.0 (SPSS, Inc., Chicago, Illinois).
Results
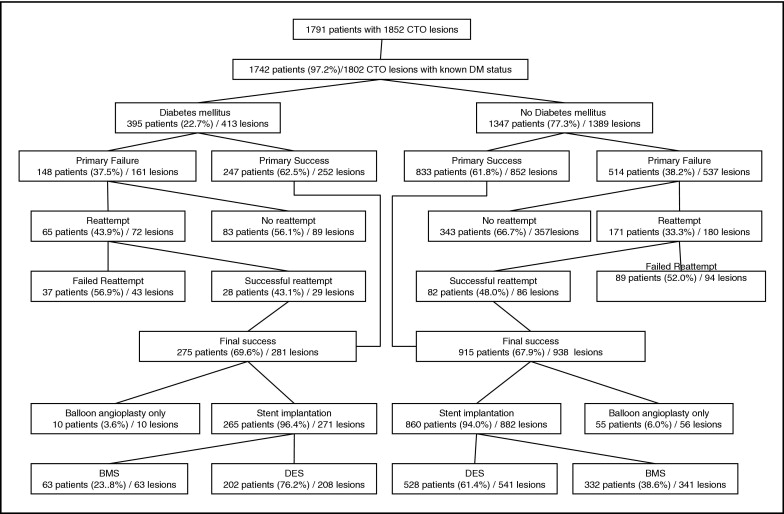
Figure 1 shows the patient flow for the present analysis. A total of 1,802 CTO lesions were attempted in 1,742 patients with known DM status, of whom 395 patients (22.7%) had diagnoses of DM at the time of the index procedure. A total of 164 patients had insulin-dependent DM (41.5%). Table 1 shows baseline demographic, angiographic, and procedural characteristics for patients with versus without DM. Patients with DM were more often male; had higher rates of hypertension, smoking, hypercholesterolemia, and chronic kidney disease; more often had histories of coronary artery bypass grafting; and had lower left ventricular ejection fractions. Procedural success rates were similar in the DM group and the no-DM group.
| Diabetes Mellitus | Patients With Diabetes Mellitus | Patients Without Diabetes Mellitus | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Yes (n = 395, 22.7%) | No (n = 1,347, 77.3%) | p Value | Successful PCI (n = 275, 69.6%) | Failed PCI (n = 120, 30.4%) | p Value | Successful PCI (n = 915, 67.9%) | Failed PCI (n = 432, 32.1%) | p Value |
| Baseline characteristics | |||||||||
| Age (years) | 61.9 ± 9.5 | 61.3 ± 10.9 | 0.3 | 61.9 ± 9.5 | 62.1 ± 9.4 | 0.63 | 60.9 ± 11.0 | 62.1 ± 10.7 | 0.75 |
| Male gender | 87.2% | 82.5% | 0.03 | 81.1% | 85.8% | 0.25 | 85.9% | 89.8% | <0.05 |
| Hypertension | 70.6% | 56.5% | <0.01 | 69.1% | 74.2% | 0.31 | 57.2% | 55.1% | 0.46 |
| Smoking | 33.0% | 24.5% | <0.01 | 35.4% | 27.5% | 0.11 | 25.8% | 21.8% | 0.11 |
| Hypercholesterolemia | 75.0% | 61.2% | <0.01 | 76.9% | 71.7% | 0.29 | 63.2% | 57.6% | 0.06 |
| Prior myocardial infarction | 47.1% | 50.5% | 0.24 | 43.3% | 55.8% | 0.03 | 47.8% | 56.6% | <0.01 |
| Prior coronary artery bypass surgery | 19.2% | 14.6% | 0.03 | 15.6% | 27.5% | <0.01 | 12.7% | 18.8% | <0.01 |
| Ejection fraction | 51.5 ± 10.4% | 53.9 ± 10.2% | <0.01 | 51.8 ± 10.0% | 50.9 ± 11.5% | 0.07 | 54.3 ± 10.1% | 53.0 ± 10.5% | 0.21 |
| Chronic kidney disease | 7.1% | 2.3% | <0.01 | 7.7% | 6.9% | 0.78 | 2.0% | 3.0% | 0.22 |
| Insulin-dependent diabetes mellitus | 41.5% | n/a | n/a | 40.4% | 44.2% | 0.48 | n/a | n/a | n/a |
| Angiographic and procedural characteristics | |||||||||
| Number of CTOs attempted per patient | 1.05 ± 0.22 | 1.03 ± 0.17 | <0.05 | 1.05 ± 0.22 | 1.05 ± 0.21 | 0.82 | 1.04 ± 0.2 | 1.0 ± 0.08 | <0.01 |
| CTO located in | 0.34 | 0.41 | 0.08 | ||||||
| Left anterior descending artery | 32.7% | 35.3% | 32.4% | 33.1% | 37.7% | 30.4% | |||
| Circumflex | 26.2% | 22.0% | 27.4% | 23.3% | 21.9% | 22.2% | |||
| Right coronary artery | 40.9% | 42.0% | 40.2% | 42.9% | 39.9% | 46.9% | |||
| Left main | 0.5% | 0.2% | 0% | 0.8% | 0.5% | 0.4% | |||
| Multivessel disease | 71.8% | 67.6% | 0.14 | 67.4% | 81.7% | <0.01 | 64.6% | 74.0% | <0.01 |
| CTO length (mm, per lesion) | 23.0 ± 15.8 | 23.8 ± 15.3 | 0.54 | 21.7 ± 16.3 | 25.5 ± 14.7 | 0.75 | 22.8 ± 15.5 | 26.2 ± 14.6 | 0.65 |
| Double coronary injection | 25.9% | 26.2% | 0.92 | 23.6% | 31.1% | 0.12 | 28.7% | 20.9% | <0.01 |
| Residual dissection | 6.5% | 5.8% | 0.57 | 4.0% | 13.0% | <0.01 | 4.6% | 8.4% | 0.1 |
| Coronary perforation during procedure | 4.2% | 3.1% | 0.32 | 1.5% | 11.0% | <0.01 | 1.9% | 6.1% | <0.01 |
| Total amount of contrast used (ml) | 466 ± 225 | 480 ± 224 | 0.51 | 484 ± 227 | 457 ± 207 | 0.61 | 485 ± 210 | 384 ± 271 | 0.09 |
| Reattempts after prior failed PCI | 16.5% | 12.7% | 0.06 | n/a | n/a | n/a | n/a | n/a | n/a |
| Procedural success | 69.6% | 67.9% | 0.53 | n/a | n/a | n/a | n/a | n/a | n/a |
| Number of patients treated with stents | n/a | n/a | n/a | 265 (96%) | n/a | 860 (94%) | n/a | ||
| Number of stents per lesion ⁎ | n/a | n/a | n/a | 1.7 ± 1.0 | n/a | 1.6 ± 1.0 | n/a | ||
| Stent length (mm, per stented lesion) ⁎ | n/a | n/a | n/a | 45.5 ± 26.2 | n/a | 39.5 ± 24.6 | n/a | ||
| Stent type ⁎ | n/a | n/a | n/a | ||||||
| Bare metal stent | n/a | n/a | n/a | 23.8% | n/a | 38.9% | n/a | ||
| Sirolimus-eluting stent | n/a | n/a | n/a | 52.5% | n/a | 44.9% | n/a | ||
| Paclitaxel-eluting stent | n/a | n/a | n/a | 23.4% | n/a | 16.0% | n/a | ||
| Other drug-eluting stent type | n/a | n/a | n/a | 0.4% | n/a | 0.2% | n/a | ||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


