Lobectomy: Thoracoscopic
Tyler Grenda
Jules Lin
DEFINITION
Video-assisted thoracic surgery (VATS) lobectomy is defined as an anatomic lobectomy in which bronchial and vascular ligation is performed with lymph node sampling or dissection through several small incisions while avoiding spreading of the ribs. VATS is an appealing alternative to thoracotomy but must follow the same principles with vascular ligation, resection with negative margins, and appropriate lymph node dissection.
PATIENT HISTORY AND PHYSICAL FINDINGS
A detailed history and physical must be performed prior to any treatment including past medical and surgical history, allergies, medications, social, and family history.
The patient’s previous history of tobacco use as well as any chemical or asbestos exposures should be determined. Cessation of tobacco use preoperatively should be strongly encouraged for 4 weeks prior to any surgical intervention.
The history should include the patient’s current functional status and exercise tolerance.
A complete physical examination should be performed with particular attention to auscultation of the heart and lungs and any evidence of cervical or supraclavicular lymphadenopathy or peripheral edema.
Routine laboratory studies including a complete blood count and basic chemistry panel should be included as part of the preoperative evaluation.
IMAGING AND OTHER DIAGNOSTIC STUDIES
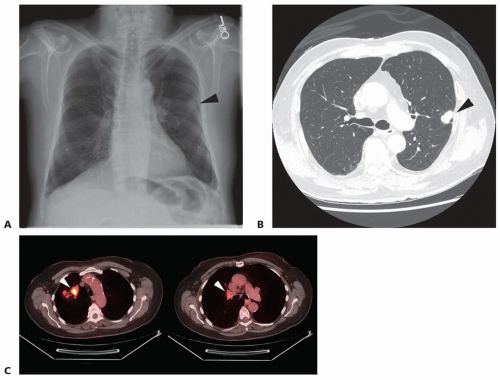
Patients typically present with abnormal chest radiograph (FIG 1A) or chest computed tomography (CT) findings. If available, the findings should be compared to previous imaging to determine any interval changes. Lesions that are stable for more than 2 years are generally considered benign. Indeterminate lesions less than 1 cm in size can be followed on serial imaging according to the recommendations of the Fleischner Society.1
A chest CT (FIG 1B) should be obtained in all patients with a suspicious lung nodule to evaluate the size and characteristics of the nodule; proximity to the chest wall, vessels, airway, and mediastinum; additional pulmonary lesions; and hilar or mediastinal lymphadenopathy. The CT should include the upper abdomen to evaluate the liver and adrenal glands for metastatic disease.
A positron emission tomography (PET) scan (FIG 1C) provides additional information regarding the metabolic activity of the pulmonary nodule and areas of uptake that are suspicious for regional nodal or distant metastatic disease
and should be obtained in all patients suspected of having a non-small cell lung carcinoma.2 In patients with abnormal findings on fluorodeoxyglucose (FDG)-PET imaging, sampling of the abnormal lymph node should be performed prior to lung resection either by endobronchial ultrasound (EBUS) or mediastinoscopy.
For patients with non-small cell lung carcinoma who are surgical candidates, anatomic lobectomy and mediastinal lymph node dissection for complete oncologic resection and staging is recommended.3
Due to the low morbidity and mortality after wedge resection, our preference for nodules that are highly suspicious for lung carcinoma based on PET or serial imaging is to perform a VATS wedge resection for a tissue diagnosis. Needle biopsies are performed less often and are reserved for cases where the diagnosis is less clear or for central lesions that would require a lobectomy for diagnosis alone.
SURGICAL MANAGEMENT
Preoperative Planning
Preoperative risk assessment determines whether a patient will tolerate pulmonary resection based on pulmonary reserve (pulmonary function tests [PFTs]) and other comorbidities.4 Patients with significant cardiovascular risk factors or symptoms should undergo preoperative cardiac evaluation.
Patients with a preoperative forced expiratory volume in 1 second (FEV1) of more than 60% predicted and diffusing capacity of lung for carbon monoxide (Dlco) of more than 50% predicted are candidates for lobectomy. Patients not meeting these criteria should undergo further evaluation with a quantitative ventilation perfusion scan to determine their postoperative predicted pulmonary function with a minimum postoperative value of 40% predicted.
Cardiopulmonary exercise testing is occasionally helpful in patients whose symptoms do not correlate with the severity of their pulmonary function results.
For patients who will not tolerate an anatomic lobectomy, alternatives include a sublobar resection such as a segmentectomy or wedge resection, stereotactic body radiation therapy (SBRT), radiofrequency ablation (RFA), or definitive chemoradiation. These patients are best discussed in a multidisciplinary setting.
Relative contraindications for VATS lobectomy are listed in Table 1.
In the preoperative area, the history and physical should be reviewed and consent should be obtained. The operative side should be appropriately marked.
Once in the operating room, a flexible bronchoscopy should be performed to verify airway anatomy and rule out any endobronchial lesions.
Single-lung ventilation is achieved with a left-sided double lumen endotracheal tube, which is generally preferable to a bronchial blocker.
Table 1: Relative Contraindications to Thoracoscopic Lobectomy | |||||||
|---|---|---|---|---|---|---|---|
|
Positioning
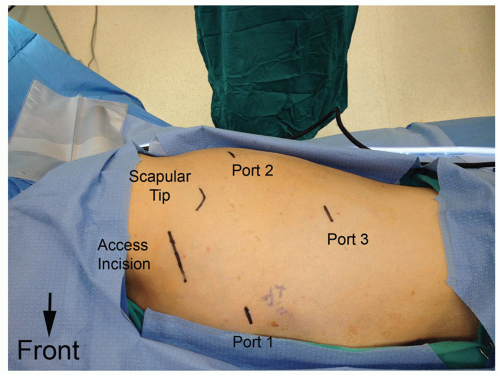
The patient should be placed in the lateral decubitus position, tilted slightly posteriorly. The bed is flexed taking care to drop the hips out of the way of the camera port (FIG 2). The arms should be positioned in an arm holder in neutral position. The patient should then be secured and all pressure points padded.
Following positioning, the endotracheal tube position should be confirmed again by the anesthesiologist.
 FIG 2 • The patient is placed in the lateral decubitus position. It is important to drop the hip out of the way of the camera, which is placed in the most inferior port. |
PLACEMENT OF INCISIONS
Port placement is important to obtain the ideal angles for stapler placement and lung retraction. Our general port placement for a VATS lobectomy is shown (FIG 3).
Port 1 is placed just below the inframammary crease in the 6th intercostal space in the anterior axillary line. A 5-mm, 30-degree angled scope is preferable to decrease compression of the intercostal nerve. The remaining ports can be placed under direct visualization.
Port 2 is placed posteriorly in the auscultatory triangle in the 6th intercostal space. Placing this incision one interspace lower is helpful for an upper lobectomy in passing the stapler when dividing the superior pulmonary vein.
Port 3 is placed in the 8th or 9th intercostal space in the posterior axillary line, taking care to avoid injuring the diaphragm.
An access incision (<10 cm) is placed in the 4th intercostal space in the midaxillary line (directly above the superior
pulmonary vein for an upper lobectomy or one space lower for a middle or lower lobectomy) for dissection and retrieval of the specimen. A Weitlaner retractor is used to hold the incision open to prevent suction from reexpanding the lung. In the event of bleeding, a sponge stick can be quickly inserted through the access incision to hold pressure.
The surgeon operates through port 1 and the access incision while the assistant positions the lung using Foerster clamps in port 2. The camera is placed in the most inferior port 3.
Thoracoscopic exploration should be performed looking for any effusion, pleural lesions, or unexpected nodules in the remainder of the lung.
If the lung is not adequately collapsed, suction should be applied to the appropriate lumen of the endotracheal tube.
LOCALIZATION OF THE LUNG NODULE
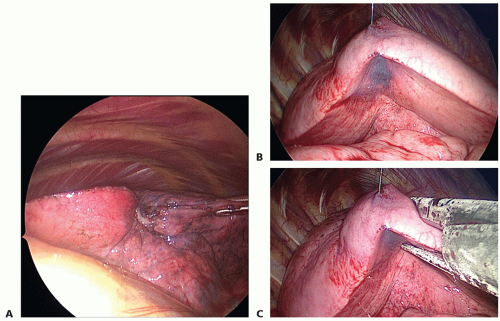
The nodule is localized by correlating the chest CT with the visualized anatomy. The nodule is then palpated with either the surgeon’s finger or an instrument (FIG 4A). Care should be taken not to crush the nodule, which could make it hard to identify. In addition, rupturing the mass risks pleural spread of disease.
As screening chest CTs identify smaller nodules, preoperative localization with methylene blue or coil/wire placement by CT guidance or super dimensional bronchoscopy may be helpful in identifying ground glass nodules (<1 cm), small nodules (<5 mm), or nodules deep to the pleural surface intraoperatively (FIG 4B).
A Foerster clamp can be used to compress the lung below the nodule to help with passage of the stapler if needed.
A stapler (Ethicon, Inc, San Antonio, TX or Covidien, Inc, Mansfield, MA; purple load Endo GIA 3.0- to 4.0-mm stapler height) is used to perform the wedge resection (FIG 4C).
The specimen is placed in a bag to prevent port site recurrence.
If the specimen is benign, cultures are sent and the procedure is terminated.
If cancer is confirmed, the access incision is made in the 4th intercostal space and a thoracoscopic lobectomy is performed.
RIGHT UPPER LOBECTOMY
The major and minor fissures should be inspected, and the location of the tumor in the right upper lobe should be confirmed. The lung is retracted posteriorly to expose the hilum.
The dissection is performed from anterior to posterior as opposed to the traditional fissure dissection used in an open lobectomy.
The anterior mediastinal pleura is opened sharply to avoid injuring the phrenic nerve using thoracoscopic Metzenbaum scissors and pickups (FIG 5A).
The superior pulmonary vein is dissected bluntly with a long coronary tip suction. The division between the upper lobe and middle lobe venous branches must be identified (FIG 5B). The minor fissure can be followed anteriorly to ensure that the middle lobe vein is preserved. Attention must also be taken to avoid injury to the underlying right pulmonary artery.
The upper lobe venous branches are isolated and divided using a vascular beige load stapler (2.0- to 3.0-mm stapler height) through the posterior incision (FIG 5B). If needed, the vessels can be encircled with a silk tie for traction or a curved-tip stapler can be used to assist in passage of the stapler.
Following division of the pulmonary vein, the pulmonary artery is then exposed. The truncus anterior branch of the pulmonary artery is then carefully isolated and divided using a beige load stapler through the posterior incision (FIG 5C).
Once the truncus anterior has been divided, the right upper lobe bronchus is exposed. The lung is then retracted anteriorly, and the pleura is opened posteriorly. The branch point between the upper lobe bronchus and the bronchus intermedius is identified (FIG 5D). Stations 10R and 11R lymph nodes are often taken at this time, which helps with the dissection.
The lung is then retracted posteriorly. The upper lobe bronchus is isolated and clamped flush with the bronchus intermedius. The lung is gently reinflated with a hand breath to ensure that the bronchus intermedius is patent before dividing the upper lobe bronchus using a purple load (size of staple) stapler through the anterior incision (FIG 5E).
The posterior ascending arterial branch to the right upper lobe (FIG 5F) is then dissected free and divided using a beige load stapler through the posterior incision.
A purple load stapler through the anterior incision is then used to divide the minor fissure to complete the resection of the right upper lobe (FIG 5G). Care should be taken to preserve the middle lobe vein and underlying pulmonary artery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree