Fig. 18.1
Tip of the new convex probe endobronchial ultrasound (CP-EBUS, BF-UC160F-OL8, Olympus, Tokyo, Japan). The outer diameter of the insertion tube of the flexible bronchoscope is 6.2 mm. CP-EBUS has a linear curved array ultrasonic transducer of 7.5 MHz (a). The balloon attached to the tip of the bronchoscope is inflated with normal saline, and a dedicated TBNA needle is inserted through the working channel (b)
Ultrasound Processor
The ultrasound image is processed by connecting the CP-EBUS to either the dedicated ultrasound scanner (EU-C60, Olympus, Tokyo, Japan), the universal endoscopic ultrasound scanner with capabilities of radial probe EBUS imaging (EU-ME1, Olympus, Tokyo, Japan), or the Aloka Prosound Alpha5 (Aloka) for excellent image quality (Fig. 18.2). The EU-ME1 is equipped with the power Doppler mode as well as the color Doppler mode (Fig. 18.3). The ultrasound images can be captured, and the size of lesions can be measured in two dimensions by the placement of cursors. The area and the circumference enclosed by caliper tracking can be measured as well.
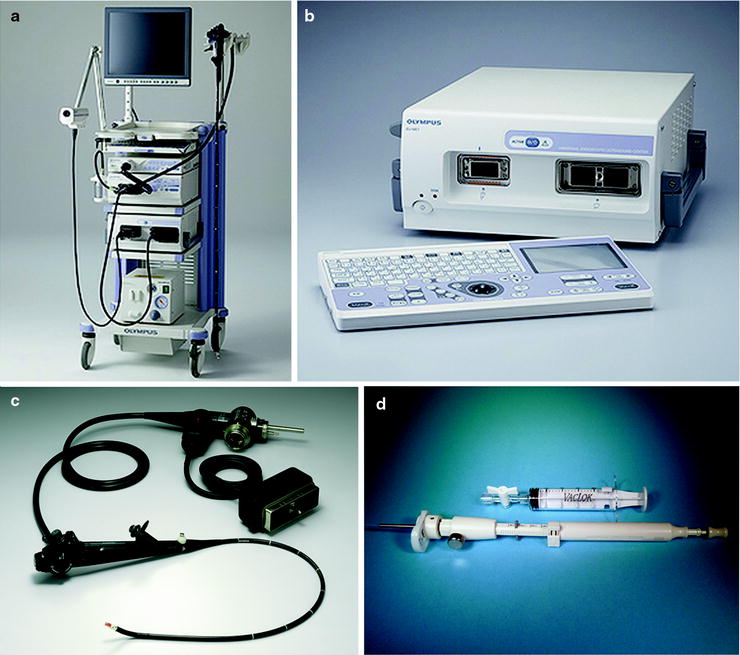
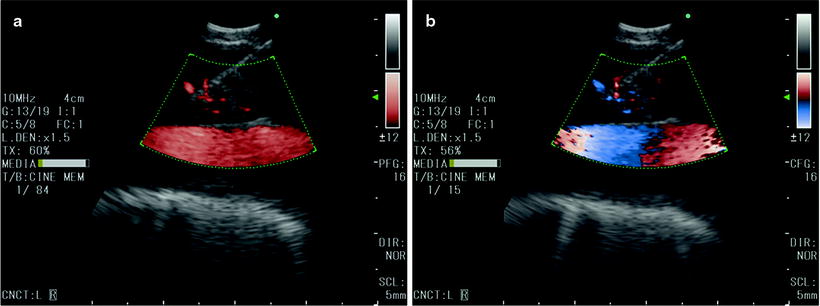
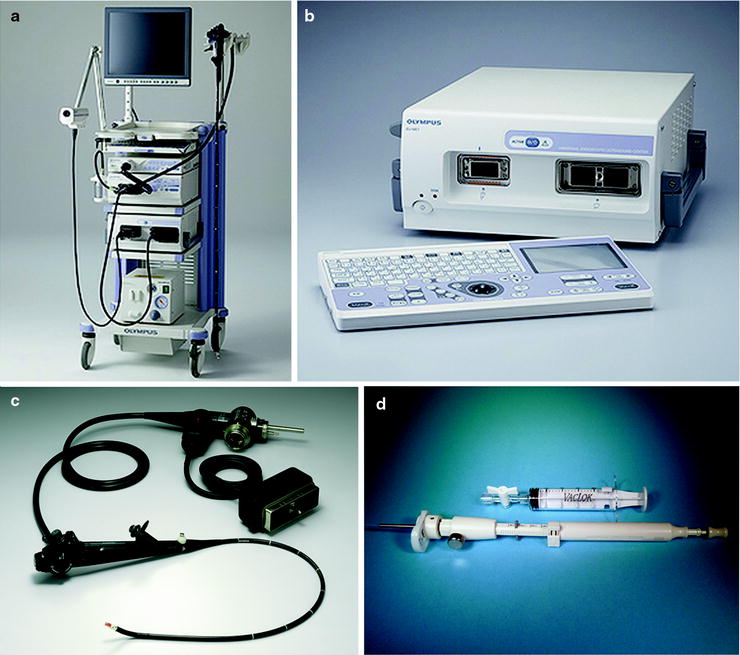
Fig. 18.2
The endobronchial ultrasound system. The tower includes the universal endoscopic ultrasound scanner with capabilities of radial probe EBUS imaging as well as the convex probe endobronchial ultrasound (EU-ME1, Olympus, Tokyo, Japan) (a, b). The convex probe endobronchial ultrasound (CP-EBUS, BF-UC180F-OL8, Olympus, Tokyo, Japan) (c) is used with the dedicated 22- or 21-gauge needle (NA-201SX-4022/NA-201SX-4021, Olympus, Tokyo, Japan) and the Vaclok syringe used to create negative pressure (d)
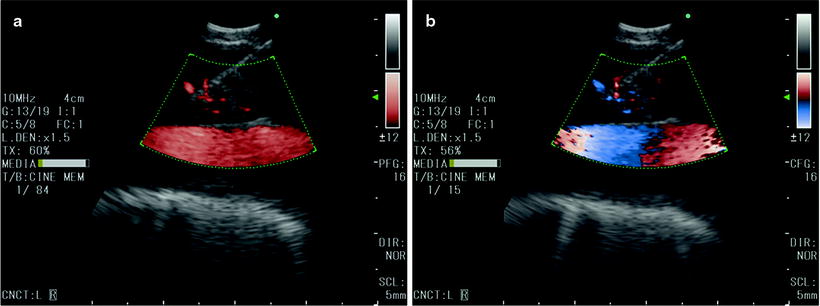
Fig. 18.3
The ultrasound processor is also equipped with the power Doppler mode (a) as well as color Doppler mode (b)
Dedicated TBNA Needle
Two types of dedicated needles are available for EBUS-TBNA. The 21-gauge (NA-201SX-4021) or the 22-gauge needle (NA-201SX-4022) passed through the 2.2-mm instrument channel allows real-time EBUS-TBNA (Fig. 18.2d). This needle has various adjuster knobs which work as a safety device to prevent damage of the channel. The maximum extruding stroke is 40 mm, and to prevent excessive protrusion, a safety mechanism stops the needle at the stroke of 20 mm. The needle is also equipped with an internal sheath which is withdrawn after passing the bronchial wall, avoiding contamination during TBNA. This internal sheath is also used to clear out the tip of the needle after passing the bronchial wall. The exit of the needle is at 20° with respect to the outer covering of the insertion tube. The needle can be visualized through the optics and on the ultrasound image.
Procedural Technique
Anesthesia
EBUS-TBNA can be performed on an outpatient basis under conscious sedation. The bronchoscope is usually inserted orally, since the ultrasound probe on the tip will limit nasal insertion. Some investigators prefer the use of the endotracheal tube or rigid bronchoscopy under general anesthesia. An endotracheal tube larger or equal to size 8 is required due to the size of the EBUS-TBNA scope. Cough reflex is minimal under general anesthesia which may be an advantage during the procedure. However, operators should be careful not to put excessive pressure with the probe on to the airway. The disadvantage of the endotracheal tube is that it causes the bronchoscope to lie in the central position within the airway which creates difficulty to bring its tip in close proximity to the trachea or bronchus. The use of the laryngeal mask airway has been shown to be useful during EBUS-TBNA.
Insertion to Visualization of Lymph Nodes
Two separate monitors should be used during EBUS-TBNA: one for the endoscopic image and one for the ultrasound image (Fig. 18.4). Since the linear curved array transducer is on the tip of the flexible bronchoscope, the optic located proximal to the ultrasound probe is set at a 35-degree forward oblique angle. Therefore, in order to obtain a straight view, the tip of the bronchoscope needs to be slightly flexed down. The bronchoscopist also needs to be aware that the 7.5-MHz ultrasound probe attached on the tip of the bronchoscope is not visible without the inflation of the balloon. Careful attention should be made to advance the scope atraumatically.


Fig. 18.4
Bronchoscopists performing endobronchial ultrasound-guided transbronchial needle aspiration under local anesthesia. A two-screen display is preferable for endobronchial images as well as ultrasound images during the procedure
After achieving local anesthesia and conscious sedation, the CP-EBUS is inserted orally and passed through the vocal cords by visualizing the anterior angle of the glottis (Fig. 18.5a). Once the bronchoscope is introduced into the airway until the desired position is reached for EBUS imaging (Fig. 18.5b), the balloon is inflated with normal saline to achieve a maximum contact with the tissue of interest. The tip of the CP-EBUS is flexed and gently pressed onto the airway. Ultrasonically visible vascular landmarks are used to identify the specific lymph node stations according to the International Lymph Node Map by the International Association for the Study of Lung Cancer. The Doppler mode is used to confirm and identify surrounding vessels as well as the blood flow within lymph nodes. There is a standard EBUS classification system of sonographic features of lymph nodes on EBUS. One can predict malignant versus benign during lymph node staging with EBUS-TBNA. Lymph nodes larger than 1 cm in short axis, round shaped, distinct margins, heterogeneous echogenicity, with the presence of coagulation necrosis sign and without the presence of central hilar structures are suspicious for malignancy and need to be biopsied (Fig. 18.6).
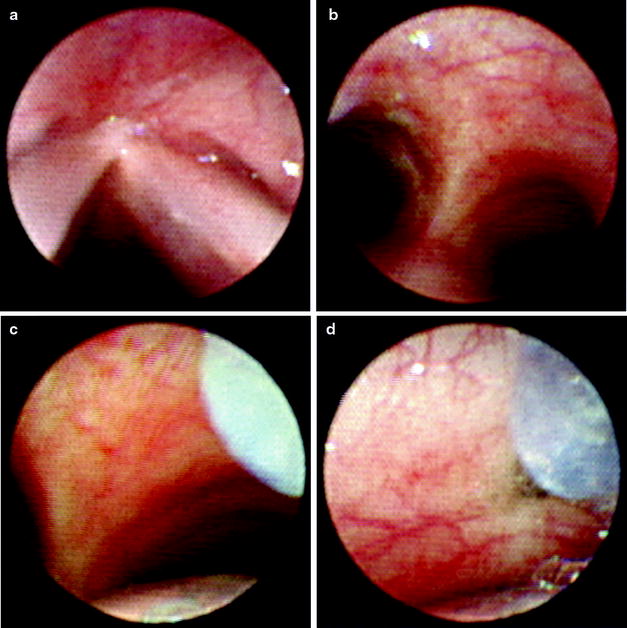
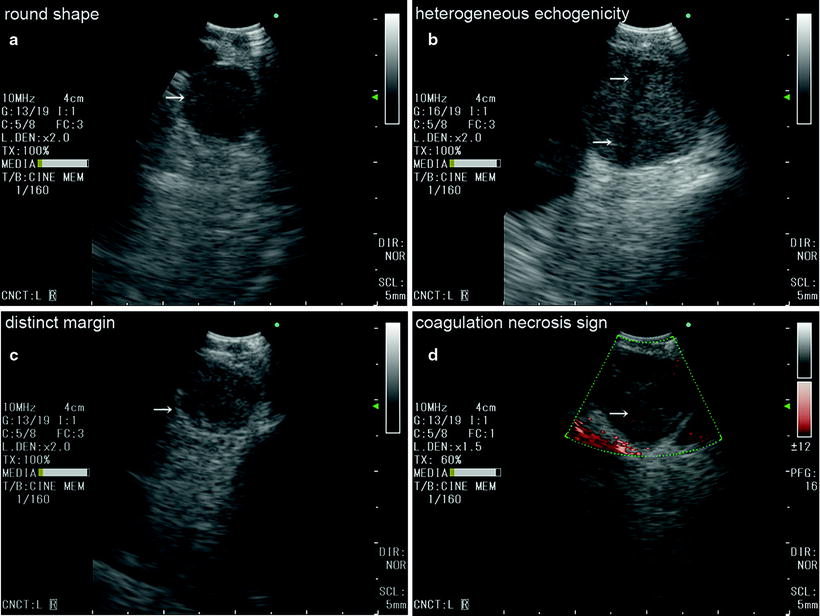
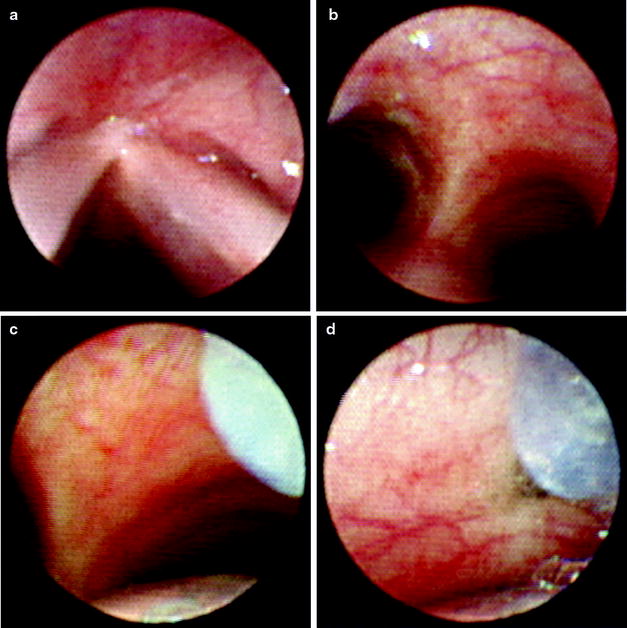
Fig. 18.5
Endobronchial images of the EBUS-TBNA procedure. The bronchoscope is passed through the vocal cords by visualizing the anterior angle of the glottis (a). In order to obtain a straight view, the bronchoscope needs to be slightly flexed down (b). The balloon is inflated with normal saline for maximum contact, and the tip is gently pressed onto the airway (c). The needle is passed through the intercartilage space (d)
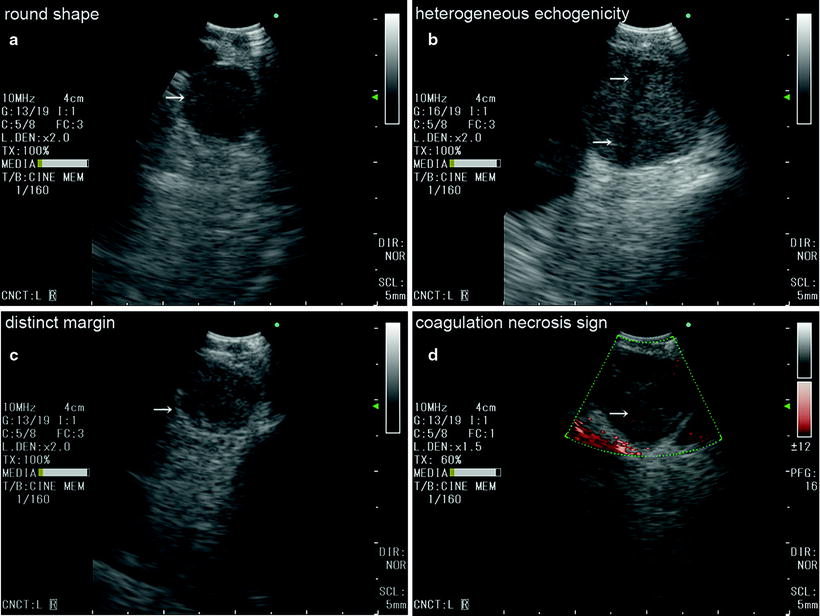
Fig. 18.6
Sonographic features of lymph nodes during endobronchial ultrasound. Lymph nodes with the following characters: round shape (a), heterogeneous echogenicity (b), distinct margin (c), and presence of coagulation necrosis sign (d) are independent predictive factors for lymph node metastasis and should be biopsied. White arrows represent each sonographic characteristics
Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration (EBUS-TBNA)
After identifying the lesion of interest, the bronchoscopic image of the airway is simultaneously visualized to localize the insertion point of the needle. Once the point of entry is decided using small landmarks on the airway, the dedicated TBNA needle is fastened on to the working channel of the bronchoscope. The manipulation of the needle is a very important element of performing EBUS-TBNA and is shown in Fig. 18.7. The sheath adjuster knob is loosened, and the length of the sheath is adjusted so that the sheath can be visualized on endoscopic image (Fig. 18.5c). The tip of the bronchoscope is flexed up for contact, and the lymph node is visualized again on ultrasound image. After the needle adjuster knob is loosened, the needle can be passed through the airway into the lymph node. The cartilaginous ring should be avoided during penetration (Fig. 18.5d). Once the needle is confirmed inside of the lymph node, the internal stylet is used to clear out the internal lumen, which may become clogged with bronchial membrane. The internal sheath is then removed, and negative pressure is applied with the Vaclok syringe. In case of a hyper vascular lymph node, negative pressure may cause bloody samples; thus, EBUS-TBNA can be done without suction. The needle is moved back and forth inside the lymph node to obtain samples. Finally, the needle is retrieved inside of the outer sheath, and entire needle is removed from the bronchoscope.
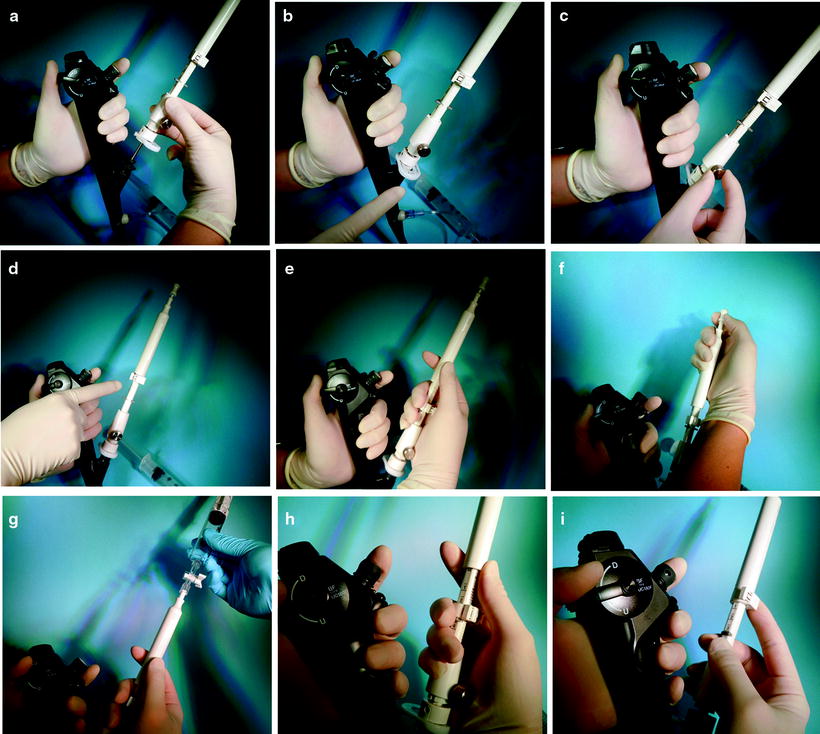
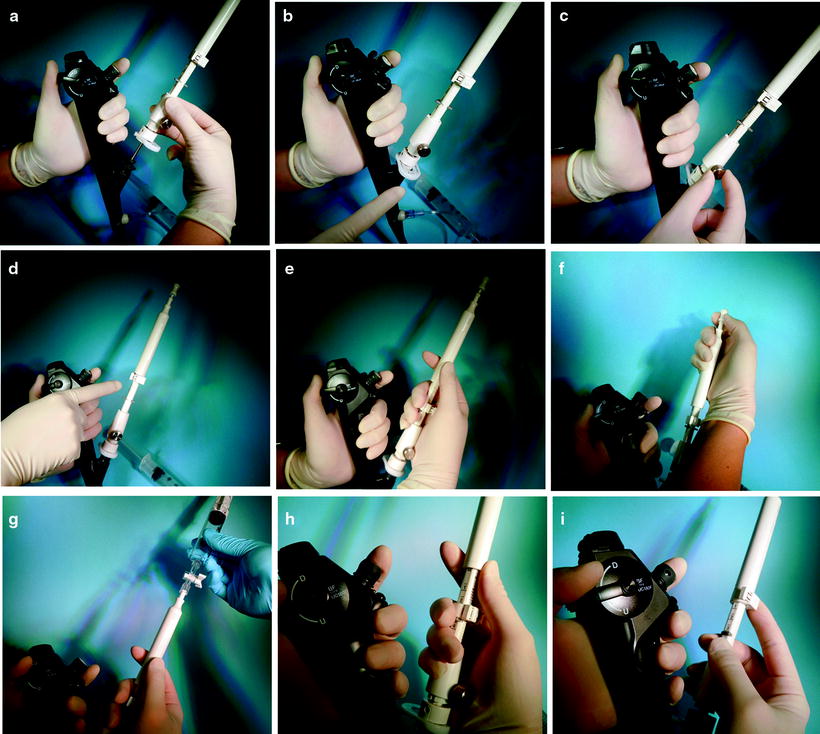
Fig. 18.7
Manipulation of the dedicated needle. The assistant should assist the operator so that the needle does not kink during this process (a). The needle is fastened on to the working channel (b). The sheath adjuster is loosened and the length adjusted (c). The needle adjuster is unlocked (d). EBUS-TBNA is performed (e). After the initial puncture, the internal stylet is used to clear out the internal lumen (f). Negative pressure is applied with the Vaclok syringe (g). Pull the needle back into the outer sheath until you hear the click on the needle (h). Lock the needle and pull the outer sheath back into the channel of the bronchoscope (i)
It is extremely important to process the specimen obtained by EBUS-TBNA in a proper way to achieve maximum results. Although the EBUS-TBNA procedure can be performed successfully by following the steps explained in this chapter, handling of the specimen may differ between centers, and this would depend on the preference of the cytopathologist and thus should follow your institutional standards. The internal stylet is usually used to push out samples. With the presence of a cytopathologist, the first few drops are placed on the slide glass, and smears are made for rapid on-site cytological evaluation using Diff-Quik staining (Fig. 18.8). The rest of the specimen is placed in a 50-ml conical filled with normal saline for cellblock preparation. The remaining specimen within the needle is also washed in this conical.
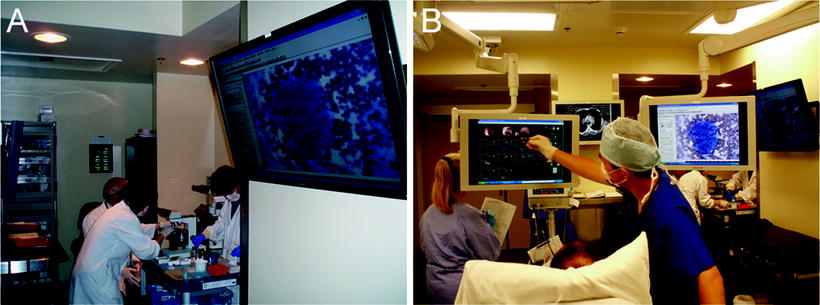
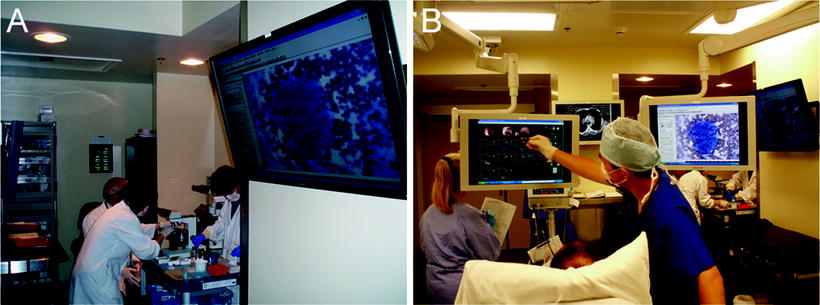
Fig. 18.8
Rapid on-site cytological evaluation of aspirates. Results of rapid on-site cytological evaluation are projected on to a large display in the Interventional Thoracic Surgery Suite (a). The results of the procedure can be explained to the patient immediately after the completion of the procedure (b)
Systematic Assessment of Mediastinal and Hilar Lymph Nodes
Prior to EBUS-TBNA, all of the mediastinal and hilar lymph nodes should be assessed, characterized, and documented in a systematic way. Lymph nodes should be identified according to the International Lymph Node Map by the International Association for the Study of Lung Cancer (Fig. 18.9). The vascular anatomy is used for identification of the lymph nodes. The authors prefer to start the lymph node assessment from the hilum, working up into the mediastinum and ending in the contralateral hilum. To avoid contamination and upstaging, EBUS-TBNA should be performed from the N3 nodes, followed by N2 nodes and N1 nodes.
Fig. 18.9
Regional lymph node map for lung cancer staging. EBUS-TBNA: endobronchial ultrasound-guided transbronchial needle aspiration. EUS-FNA: endoscopic ultrasound-guided fine needle aspiration
Representative lymph node stations, bronchoscopic landmarks for optimal ultrasound visualization, and ultrasound images of lymph nodes and surrounding vessels are explained in details below.
Station #12R
The bronchoscope is advanced into the right lower lobe bronchus. The tip of the CP-EBUS is flexed up against the lower lobe bronchus just proximal to where the basal bronchus branches. Station #12R can be visualized adjacent to the interlobar pulmonary artery.
Station #11R
Straighten and withdraw the bronchoscope to the intermediate bronchus. Turn to the 2-o’clock position and flex the tip just distal to the entrance of the right upper lobe bronchus. Station #11R can be visualized with the interlobar pulmonary artery running distal to the lymph node.
Station #10R
Withdraw the bronchoscope to the right main bronchus. Turn the tip to the 3-o’clock position and flex the tip to visualize station #10R. Lymph nodes identified distal to the azygos vein is station #10R.
Station #7
Station #7 can be visualized from either the right or the left main bronchus. On the right side, turn to the 12-o’clock position and flex the tip against the right main bronchus to visualize the right main pulmonary artery. After confirmation with the Doppler mode, turn the tip counterclockwise to the 9-o’clock position to visualize station #7.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


