Left Ventricular Function Cardiomyopathy
Systolic Function
There is considerable literature devoted to load-independent measures of contractility, but the venerable ejection fraction, for all its load dependence and the well-known and well-described vagaries of measuring it, remains a useful tool for the assessment of ventricular function. Where edges are well defined (with the use of contrast as necessary to visualize endocardium), echocardiography can provide a reasonable estimate of left ventricular ejection fraction.
An advantage of transesophageal echocardiography (TEE) over transthoracic echocardiography (TTE) in the assessment of systolic left ventricular function is its excellent resolution of the endocardium. However, the foreshortening of the four- and two-chamber views of the left ventricle (LV) limits TEE in its capacity to calculate LVEF accurately and so, in practice, TTE is the usual approach to left ventricular ejection fraction (LVEF) calculation. On the other hand, regional wall motion can be effectively assessed, assigning a wall motion score (normal = 1; hypokinetic = 2; akinetic = 3; dyskinetic = 4; aneurysmal = 5) to each of the 17 segments as recommended by the American Society of Echocardiography. The normal myocardium thickens by approximately 30% to 50% and this can be used as a quantitative approach to scoring. In practice, scores for each segment are most often assigned on the basis of visual inspection. The segments correspond, in general, to the distribution of the different coronary arteries, but of course, individual anatomy varies. For instance, the inferior wall would be served by different arteries depending on whether the posterior descending artery arises from the right coronary artery or the left circumflex artery. The segmental scores can be added and divided by the number of segments scored to give an index of global function. An average score of 1.0 with all segments visualized would indicate a completely normal ventricle. A substantial advantage of TEE is the ability to routinely visualize the endocardium well.
Because the left ventricle contracts not only in an inward or radial fashion, but also longitudinally, attempts have been made to assess longitudinal shortening, using Doppler tissue imaging (DTI). A pulsed Doppler sample volume is placed on the mitral annulus on either the septal or the lateral aspect and the flow velocity measured. A peak velocity of 9 cm/sec is consistent with normal longitudinal left ventricular function; decreased velocities indicate diminished function.
Diastolic Function
Unlike TTE, not much work has been done on the assessment of LV diastolic function by TEE, using either Doppler mitral inflow velocities or DTI. In contrast to mitral inflow velocities, the movement of the mitral annulus in diastole has relatively limited load dependence. As a result, the peak early diastolic annular velocity measured by DTI has attained popularity for the assessment of diastolic function. An Em <8 cm/sec, when measured on the septal side, or <13 cm/sec, when measured on the lateral aspect, suggests diastolic dysfunction. Some authors have also used the Em/Am ratio (abnormal <1) but restriction of diastolic filling of the LV or loss of atrial function limits the usefulness of this ratio. Although either the septal or lateral aspect of the mitral annulus can be used, it has been suggested that the septal aspect is less error prone. On the other hand, the septal velocities may be affected by right ventricular function.
A reduced mitral inflow velocity ratio (E/A) is a classical measure of diastolic dysfunction (diagnosed when E/A <1) but is limited by pseudonormalization of the ratio as diastolic function worsens. A Valsalva maneuver can be used to unmask abnormal function, although it is difficult to get some patients to perform a proper Valsalva. Another parameter found useful in assessing LV diastolic function is a ratio of the peak early diastolic velocities obtained from the mitral inflow (E) by
regular Doppler imaging and from the mitral annulus by DTI. When the ratio is >15 the left atrial filling pressure is usually elevated and when it is <10 it is usually normal. Values between these are not of diagnostic significance. Percent change in the shortening or relaxation (strain) or the rate of change of deformation (strain rate) between two adjacent points of myocardial tissue has been utilized to assess systolic and diastolic LV longitudinal function. This methodology has been developed to reduce errors introduced by twisting and rotation of the heart during the cardiac cycle when assessing velocities using the standard DTI approach. However, this newer methodology is fraught with significant intra- and interobserver variabilities, which reduce its clinical utility.
regular Doppler imaging and from the mitral annulus by DTI. When the ratio is >15 the left atrial filling pressure is usually elevated and when it is <10 it is usually normal. Values between these are not of diagnostic significance. Percent change in the shortening or relaxation (strain) or the rate of change of deformation (strain rate) between two adjacent points of myocardial tissue has been utilized to assess systolic and diastolic LV longitudinal function. This methodology has been developed to reduce errors introduced by twisting and rotation of the heart during the cardiac cycle when assessing velocities using the standard DTI approach. However, this newer methodology is fraught with significant intra- and interobserver variabilities, which reduce its clinical utility.
It must be added that there is considerable controversy surrounding the diagnosis of heart failure with preserved systolic function and even about the presence of diastolic dysfunction-based heart failure as assessed by the above parameters. Indeed, some authors have advocated the use of a dilated left atrium as a very sensitive measure of elevated filling pressures, which, in the absence of systolic dysfunction, is consistent with a diagnosis of heart failure with preserved systolic function.
DTI is also useful in assessing LV dyssynchrony in patients with cardiomyopathy with markedly reduced LV systolic function (LV ejection fraction <35%) and left bundle branch block. Marked delay in peak annular systolic velocity observed in the LV lateral wall as compared to the septum is an indication of biventricular pacing (resynchronization therapy) in these patients. This shortens the delay, reducing or abolishing dyssynchrony with consequent improvement in LV function.
Echocardiography, in general, is a critically useful tool in the workup for heart failure and dyspnea (and also hypotension). Indeed, one of the most common clinical issues for which echocardiography is ordered is the assessment of the physiology underlying a presentation in heart failure or deciding whether shortness of breath is caused by the heart. The clinical syndrome of heart failure can result from systolic or diastolic dysfunction, valvular disease (including endocarditis), constrictive pericarditis, and even pericardial effusion. All of these are also part of the differential diagnosis of dyspnea. The assessment of diastolic dysfunction has gained increased currency with the recognition that 30% to 50% of patients with heart failure have preserved systolic function.
Generally, TTE is sufficient to make the diagnoses mentioned in the preceding text and to guide therapy. However, TEE offers an effective alternative when TTE is inadequate.
Dilated cardiomyopathy (DCM) is recognized by dilatation of the cardiac chambers and poor ventricular function. The sluggish flow that occurs in these patients may result in thrombus formation that is visible with echocardiography. Ventricular assist devices have been used to support the left and right ventricles. Some examples of imaging of the conduits that are placed in these patients are shown in this chapter.
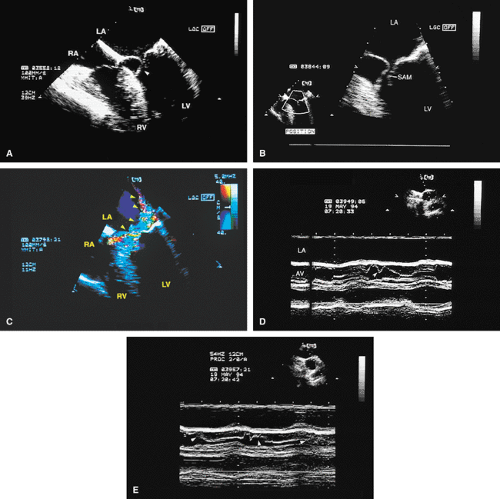
Hypertrophic cardiomyopathy is characterized by inappropriate hypertrophy of the left ventricle. Although asymmetric septal hypertrophy is the classical presentation, any wall or even the entire ventricle may be involved. Systolic anterior motion of the mitral valve occurs, leading to outflow obstruction. The result is mitral regurgitation and a subvalvular gradient across the left ventricular outflow tract (LVOT). The obstruction of the LVOT results in turbulence that can be recognized on a color flow Doppler. The velocity waveform obtained from conventional Doppler examination of the outflow tract shows a high peak velocity, reflecting the increased pressure gradient. The location of obstruction within the ventricle can be determined. Additionally, there is a slow upslope of the velocity waveform and a more rapid downslope. This differentiates it from fixed LVOT obstruction in which the velocity waveform is symmetric. Midsystolic notching of the aortic valve is another common finding. There is often evidence of reduced diastolic function.
The surgical treatment of this lesion is myomyectomy of the ventricular septum. The resection appears as a “scooped-out” area with echocardiography.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree