INDICATIONS
Sleeve lobectomy (lobectomy associated with resections and reconstruction of the bronchus, the pulmonary artery [PA], or both) is a suitable choice for the treatment of centrally located tumors, particularly lung cancer. The main indication is bronchogenic carcinoma infiltrating the lobar bronchus (Fig. 37.1A,B) and/or the origin of the lobar branches of the PA but not to the extent that a pneumonectomy is required. Sleeve lobectomy may also be indicated for N1 (hilar) lymph node infiltration of the bronchus and/or PA. This reconstructive procedure may also be indicated after induction therapy, when unremovable fibrotic tissue or residual tumor is embedded with the origin of the lobar bronchus; after induction there might also be residual tumor around the bronchus requiring a sleeve resection. In rare cases, also local recurrence at the level of a previous lobectomy bronchial stump may be an indication. Typical and atypical carcinoid tumors with the same pattern of presentation may pose the indication for a bronchial sleeve lobectomy; however, in these situations reconstruction of the PA is rarely required. Also inflammatory disorders like posttuberculosis strictures or benign tumors may seldom be an indication.
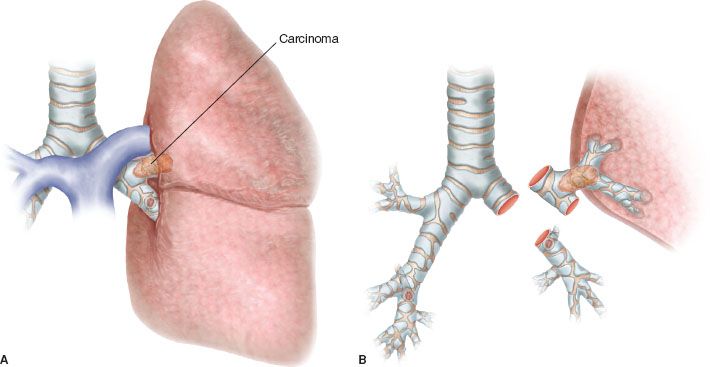
Figure 37.1 The most frequent indication to bronchial sleeve lobectomy is lung cancer infiltrating the orifice of the lobar bronchus. Here the tumor invades the origin of the left upper bronchus (A) that is removed along with a “sleeve” of main bronchus (B).
 CONTRAINDICATIONS
CONTRAINDICATIONS
In addition to the functional contraindications to a standard lobectomy (low pulmonary function, major cardiac problems, other major comorbidities), sleeve resections are clearly contraindicated when the local extension of the tumor requires pneumonectomy. Particularly, invasion of the interlobar fissure poses the indication to a more extended resection (bilobectomy on the right side or pneumonectomy).
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
The indication to a bronchial sleeve resection is usually made preoperatively, on the basis of the computed tomography (CT) and fiberoptic bronchoscopy findings. Standard workup for major pulmonary resections is recommended. Particularly, fiberoptic bronchoscopy is extremely important to assess the relationship between the upper lobe and the B6 orifices. The extension of the tumor should be carefully ascertained. Histology should be confirmed with biopsy. If extrinsic compression due to lymph node enlargement is visible at the level of the interlobar carina a transbronchial needle biopsy may be useful to plan the operation. It is extremely important that in these cases the endoscopic examination is performed or reviewed by one of the operating surgeons. This shows advantages at the time of the operation, when the bronchi are incised and divided.
When the main bronchus is partially or completely obstructed by the tumor, preoperative laser recanalization may be helpful. It contributes to improve morphologic and functional evaluation of the distal airway and lung parenchyma, helps to prevent infectious complications during induction chemotherapy, does not affect the adjacent mucosa and does not increase postoperative complications.
 SURGERY
SURGERY
Anatomical background of left upper sleeve lobectomy: The left main bronchus is 4 to 6 cm in length and it passes under the aortic arch to lie anteroinferiorly to the left PA (Figs. 37.2 and 37.3) and posteriorly to the right upper vein. The main bronchus bifurcates to give rise to the upper and lower bronchi. The greater length of the main bronchus offers more possibilities to perform left upper lobe sleeve resections; however, the adjacent aortic arch often interferes with maneuvers required to achieve optimal exposure for the anastomosis. The left upper lobe bronchus is less than 1 cm long; the lower lobe bronchus usually gives off the superior segmental bronchus (B6) posteriorly about 0.5 cm from the left upper lobe orifice. The absence of the intermediate bronchus on this side might make bronchial reconstruction more difficult when compared to the right side; the location of B6 often dictates the distal bronchial section after left upper lobe sleeve resection; this should be carefully evaluated at preoperative bronchoscopy. Also the difference in diameter between the main and the lower bronchus may cause some technical difficulties. The left recurrent laryngeal nerve is vulnerable when the dissection and anastomosis involves the proximal main bronchus; injury might be caused also by dissection of the aortopulmonary region if a combined bronchial and PA reconstruction is to be performed or during dissection of station 5 lymph nodes. The strict relationship between the bronchial tree and the PA that lies posteriorly adjacent to the bronchus offers the anatomical background for combined bronchial and PA reconstructions if cancer invades both of them.
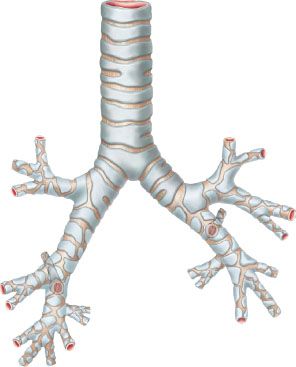
Figure 37.2 Anatomical details of the airway on the right and left side.
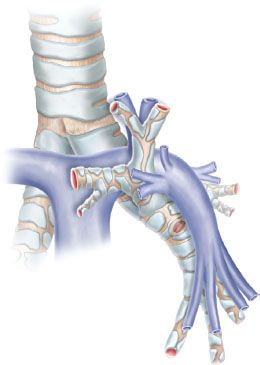
Figure 37.3 Anatomical relationship between the airway and the pulmonary artery on the left side.
Positioning and surgical incision: The patient is placed in the lateral decubitus position. Many surgeons are still convinced that wide surgical incisions should be preferred to perform technically demanding surgical procedures, particularly bronchovascular reconstructions. On the other hand, some authors have recently described Video assisted thoracic surgery (VATS) sleeve lobectomy. We believe that the standard posterolateral thoracotomy can be easily replaced by a muscle-sparing minithoracotomy or a small lateral or anterolateral thoracotomy.
Operative technique:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


