INDICATIONS/CONTRAINDICATIONS
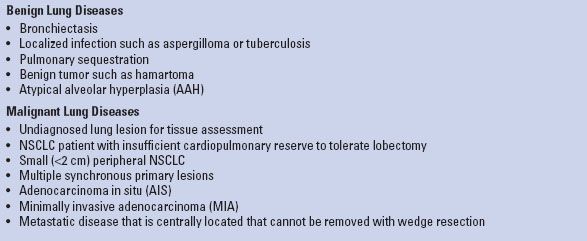
Parenchyma-sparing lung resections were first described in the 1930s by Churchill for patients diagnosed with benign lung disorders such as bronchiectasis and tuberculosis. This pioneering surgeon described segmental resection of the lung, also known as segmentectomy, using anatomic planes to resect pulmonary tissue based on the bronchovasacular anatomy. It is important that a clear distinction be made between segmentectomy and wedge resection as the latter is a sublobar resection of the lung tissue without using intersegmental planes. Segmentectomy is generally thought to be superior to wedge resection for lung cancer resections because it allows isolation of the bronchovascular structures and improved resectability of regional lymph nodes. To be successful in performing a segmental resection, a surgeon requires a thorough understanding of the three-dimensional anatomic segmental anatomy of the lung. Segmentectomy is currently performed for a wide variety of benign and malignant lung disorders (Table 27.1) and may be completed using minimally invasive or open techniques. In nonsmall cell lung cancer (NSCLC) segmentectomy has traditionally been performed for patients with limited pulmonary function for whom lobectomy is not feasible, where a lesser resection offers a more suitable alternative. More recently, publications suggest that segmentectomy may be an acceptable alternative to lobectomy in the management of patients with small (<2 cm) peripheral NSCLC tumors with local recurrence rates and 5-year survival similar to lobectomy in carefully selected patients. Although, the benefits and role of segmentectomy in patients with imaging suggesting solitary or multiple foci of atypical alveolar hyperplasia (AAH), adenocarcinoma in situ (AIS—formerly bronchoalveolar carcinoma), or minimally invasive adenocarcinoma (MIA—<5-mm invasive adenocarcinoma) remains unclear it is an often utilized approach.
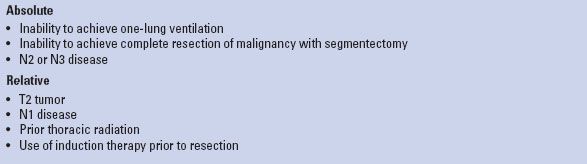
Contraindications to anatomic segmentectomy are listed in Table 27.2. Although some factors such as previous thoracic surgery, incomplete or absent lung fissures or bulky mediastinal adenopathy may make performing a segmentectomy technically more challenging, they are not considered contraindications to the procedure. Segmentectomy should not be performed in patients with a preoperative diagnosis of N2 disease. It is our opinion that patients with a preoperative diagnosis of N1 disease should preferentially undergo lobectomy. Some surgeons do, however, consider segmentectomy with complete nodal resection in select patients with known N1 disease who are not candidates for lobectomy due to limited cardiopulmonary reserve and who do not have evidence of bulky adenopathy.
TABLE 27.1 Indications for Anatomic Segmentectomy
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
As with any patient being considered for lung resection, a careful preoperative assessment should be performed to ensure suitability for surgery. After a thorough history and physical examination, an evaluation of the cardiac and pulmonary fitness should be performed using one or a combination of pulmonary function testing, low technology exercise testing with shuttle walk test (SWT) or a stair climb test (SCT). Quantitative ventilation–perfusion scans and cardiopulmonary exercise testing (CPET) is reserved for patients with significant cardiopulmonary impairment. Cardiac testing such as echocardiogram and exercise stress testing are reserved for symptomatic patients with a history of cardiac disease. For patients with suspected or confirmed lung cancer, computed tomography (CT) of the chest and upper abdomen, and positron emission tomography (PET) scanning is routinely used to assess the primary tumor as well as to rule out metastatic disease. Testing using magnetic resonance imaging or CT of the head is reserved for symptomatic patients to rule out neurologic metastases. Suspected mediastinal nodal disease identified on imaging studies is further assessed using endobronchial ultrasound and/or mediastinoscopy.
There is no universally accepted definition of what comprises a patient with poor cardiopulmonary function. At our institution, patients with predicted postoperative (PPO) forced expiratory volume in 1 second (FEV1) and/or PPO diffusion capacity (DLCO) less than 40% predicted, PCO2 >45 mm Hg, PO2 <50% on room air, ejection fraction <45%, and moderate-to-severe pulmonary hypertension are considered high risk for surgery. These marginal patients undergo CPET with measurement of maximal oxygen consumption (VO2max). If VO2max is <10 mL/kg/min (or 35% predicted) patients should be counseled about nonoperative treatment options for lung cancer and the increased risk of perioperative death and cardiopulmonary complications even with sublobar lung resection. Prior to surgery, high-risk patients with potentially resectable lung cancer should undergo smoking cessation counseling, be enrolled in a pulmonary rehabilitation program, and be evaluated by a multidisciplinary team, which includes radiation therapists, medical oncologists, pulmonologists, radiologists, and thoracic surgeons. Despite these diagnostic measures, however, it is often difficult to define a patient as medically inoperable for lung resection.
TABLE 27.2 Contraindications for Anatomic Segmentectomy
 SURGERY
SURGERY
In preparation for surgery, the patient is kept fasting for 8 hours prior to general anesthesia. The patient receives prophylactic antibiotics intravenously as well as a subcutaneous heparin injection (5,000 units) for deep vein thrombosis (DVT) prophylaxis within 60 minutes of skin incision. When the patient enters the operating room and prior to the induction of anesthesia, a detailed safety “time-out” is routinely performed involving the entire operating room team. Importantly, the correct side of the surgery is confirmed with the patient and surgeon, as well as by the anesthesia team and nursing staff. Preoperative CT or PET imaging is reviewed with the operative team prior to induction of anesthesia to check the size and segment location of the target lesion and for the presence of adenopathy.
For the open technique an epidural catheter or paravertebral catheter is often placed to optimize postoperative pain management. A left-sided double-lumen tube or bronchial blocker is used for lung isolation. Position of the double-lumen tube is confirmed using a pediatric bronchoscope.
Position
For open procedures patients are placed in the lateral decubitus position and secured in place using a bean bag or rolls. The bed is flexed at the level of the hip to extend the rib cage in the operative field. Careful padding of the extremities is undertaken to minimize the risk to the patient of developing pressure necrosis or neuromuscular injury. The top arm is carefully hung using a padded arm sling. Position of the double-lumen tube is always reconfirmed once final positioning of the patient is complete. The proposed chest incision (posterolateral thoracotomy) is then marked followed by a second safety check list review. This methodical review is done before prepping, draping, and making the incision to ensure the correct administration of medications (antibiotics and prophylactic heparin) and confirm the side of surgery and availability of blood products. At this point, the left lung is deflated and the patient prepped and draped.
Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


