12 Left Heart Anomalies
Background
• Left heart anomalies include lesions of the mitral valve (MV), left ventricular outflow tract (LVOT), aortic valve (AV), coronary arteries, and aorta (Ao). Within each of these structures there is a wide spectrum of both congenital and acquired diseases.
TABLE 12-1 SYNDROMES AND DISEASES ASSOCIATED WITH LEFT HEART LESIONS
| Left Heart Disease | Association |
|---|---|
| Coarctation of the aorta | Turner syndrome |
| Bicuspid AV | |
| Unicuspid AV | |
| Supravalvular aortic stenosis | Williams syndrome |
| Dilated aorta | Bicuspid AV |
| Marfan syndrome | |
| Loeys-Dietz syndrome | |
| Ehlers-Danlos syndrome | |
| Shprintzen-Goldberg syndrome | |
| Turner Syndrome | |
| Simultaneous left heart obstructions: mitral stenosis, aortic stenosis, coarctation | Shone syndrome |
| Hypoplastic left heart syndrome |
This list is intended to summarize more commonly associated syndromes and is not all-inclusive.
Overview of Echocardiographic Approach
• Any abnormality that is detected by echocardiography (echo) should trigger the detailed evaluation of structures both upstream and downstream of the lesion. For example, if coarctation of the aorta is diagnosed, both the AV and MV should be carefully evaluated to rule out associated functional or structural abnormalities (Box 12-1).
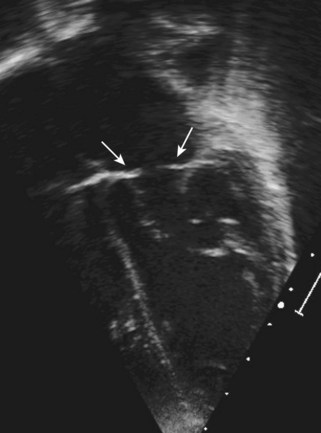
• Evaluation of lesions by two-dimensional (2D) echo should be performed via all available acoustic windows because subtle diagnostic or anatomic clues can be gleaned. A single en face view of the MV, for example, would not be able to determine whether there are problems with the submitral apparatus or whether there are signs of supramitral obstruction.
• Fine-tune 2D images to maximize resolution. Use the highest frequency transducer that windows will permit. Eliminate unnecessarily wide views by narrowing the 2D sector angle or by zooming into a region of interest. Consider changing line density if higher frame rates take priority over spatial resolution.
• Doppler imaging is critical to evaluate the hemodynamic impact of the anomaly. The regions immediately adjacent to an identified anomaly should be carefully performed to determine whether problems exist in series. Color Doppler complements spectral Doppler and can help visualize the location and degree of stenosis or regurgitation and the presence or absence of turbulence.
• Nyquist limits are inversely related to transducer frequency; if color Doppler maps or pulsed wave (PW) Doppler scales are limited, consider switching to a lower frequency setting or switch to a lower frequency transducer.
• A good-quality color Doppler map is best predicted by the quality of the 2D image and the acoustic windows. If the acoustic window or the 2D image is poor, the color Doppler maps are unlikely to be useful.
• A surprisingly good spectral Doppler tracing, however, can frequently be obtained even if 2D images are suboptimal.
Left Atrial Anomalies
Cor Triatriatum
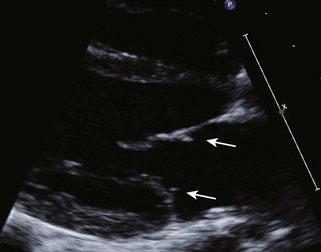
• Typically seen as an “extra” atrial septum that partially divides the left atrium (LA) into a pulmonary venous chamber and the true left atrial chamber.
Aortic Valve Anomalies
Congenital Anomalies
Anatomic Imaging
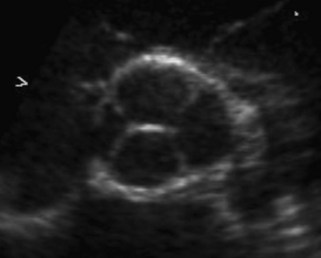
• Leaflet thickness, position, and mobility are best evaluated in the parasternal long axis and short axis. M-mode cursors can evaluate motion with good temporal resolution. With modern-day ultrasound carts, however, temporal resolution of the 2D images is almost as fine.
• In adults, estimations of AV area can determined by using the continuity equation or, less frequently, by 2D planimetry.
• Valve areas are less frequently measured in pediatric patients due to the relative lack of precision in smaller patients as well as the low frequency of low-output AS for which the AV area would be diagnostically useful.
Physiologic Data
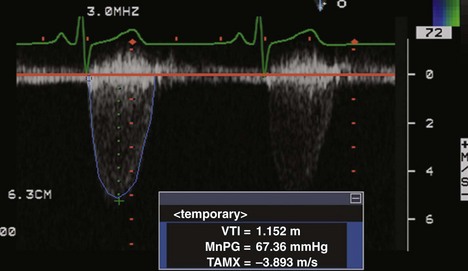
• PW Doppler and continuous wave (CW) Doppler of the subaortic and supravalvular regions should be obtained to determine whether any additional obstruction exists (Fig. 12-3).
• Peak velocity and mean gradients can be obtained from the apical windows. The mean gradient from this view best correlates with peak-to-peak estimations by catheterization.
• Overestimation of pressure gradients can occur when velocities are obtained in the suprasternal notch (SSN) or high parasternal views. Pressure recovery phenomena may account for these discrepancies.
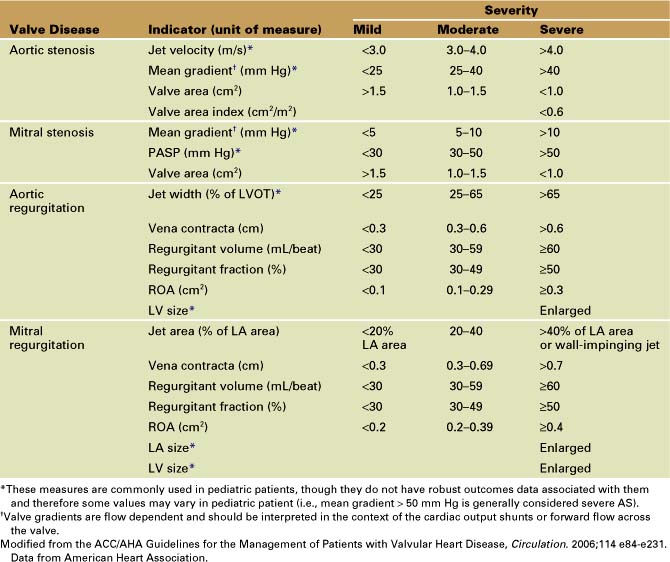
• The degree of aortic regurgitation (AR) can be determined using both color Doppler and spectral Doppler.
• PW Doppler of the ascending and descending aorta should be obtained to evaluate the volume of regurgitation.
Key Points
• Congenital AV disease is usually due to abnormalities in the number of valve leaflets and may result in AS and/or regurgitation.
• Assessment of valvular AS requires the integration of both 2D and Doppler data; when the valve appears to open well despite high transvalvular velocities, subaortic or supravalvular stenosis should be suspected.
Mitral Valve Anomalies
Congenital Anomalies
• Cleft MV.
• Is also present in other congenital diseases such as complete atrioventricular canal defects (see Chapter 6, Atrioventricular Septal Defect: Echocardiographic Assessment).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree