L
Laryngeal cancer
The most common form of laryngeal cancer is squamous cell cancer (95%); rare forms include adenocarcinoma, sarcoma, and others. Such cancer may be intrinsic or extrinsic. An intrinsic tumor is on the true vocal cord and doesn’t tend to spread because underlying connective tissues lack lymph nodes. An extrinsic tumor is on some other part of the larynx and tends to spread early.
CAUSES AND INCIDENCE
In laryngeal cancer, major predisposing factors include smoking and alcoholism; minor factors include chronic inhalation of noxious fumes and familial tendency. Cancer of the larynx rarely occurs in nonsmokers.
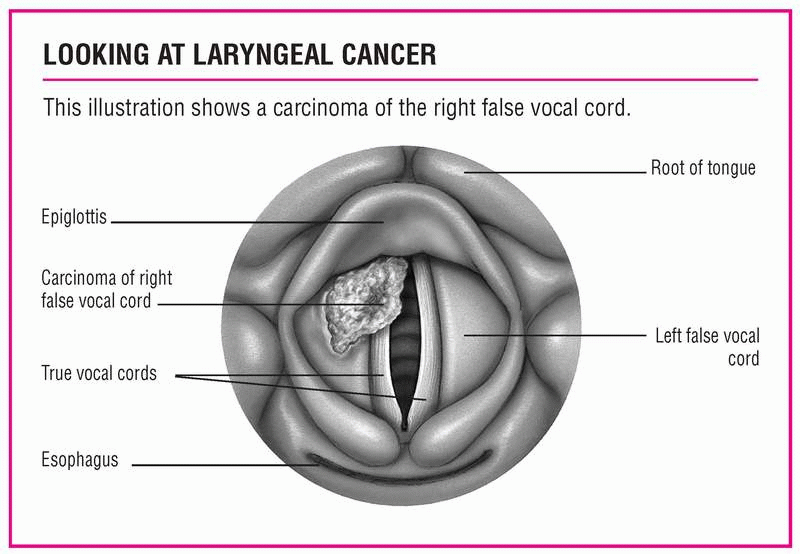
Laryngeal cancer is classified according to its location. It can occur in the supraglottis (false vocal cords), glottis (true vocal cords), or subglottis (downward extension from vocal cords [rare]). The ratio of male to female incidence is 10:1, and most victims are between ages 50 and 65. The five-year survival rate is 65%. (See Looking at laryngeal cancer.)
SIGNS AND SYMPTOMS
Signs and symptoms of laryngeal cancer include:
• hoarseness that persists longer than 3 weeks
• lump in the throat or pain or burning in the throat when drinking citrus juice or hot liquid
• dysphagia
• dyspnea
• cough
• enlarged cervical lymph nodes
• pain radiating to the ear.
COMPLICATIONS
• Airway obstruction
• Metastasis
• Pain
• Difficulty swallowing
DIAGNOSIS
• Laryngoscopy shows the presence of the tumor.
• Xeroradiography, biopsy, laryngeal tomography, computed tomography scans, or laryngography de-fine the borders of the lesion.
• Chest X-rays detect metastases. (See Staging laryngeal cancer, pages 102-103.)
TREATMENT
Early lesions are treated with surgery or radiation; advanced lesions, with surgery, radiation, and chemotherapy. In early stages, laser surgery can excise precancerous lesions; in advanced stages it can help relieve obstruction caused by tumor
growth. Surgical procedures vary with tumor size and can include cordectomy, partial or total laryngectomy, supraglottic laryngectomy, or total laryngectomy with laryngoplasty. The goal is to eliminate the cancer and preserve speech. If speech preservation isn’t possible, speech rehabilitation may include esophageal speech or prosthetic devices; surgical techniques to construct a new voice box are still experimental.
growth. Surgical procedures vary with tumor size and can include cordectomy, partial or total laryngectomy, supraglottic laryngectomy, or total laryngectomy with laryngoplasty. The goal is to eliminate the cancer and preserve speech. If speech preservation isn’t possible, speech rehabilitation may include esophageal speech or prosthetic devices; surgical techniques to construct a new voice box are still experimental.
Drugs
• Chemotherapeutic drugs, such as cisplatin; the combination of irinotecan, 5-Fluorouracil, and leucovorin (IFL); methotrexate; mitomycin; or the combination of paclitaxel, ifosfamide, and cisplatin (TIP), to slow tumor growth
• Analgesics to reduce pain
SPECIAL CONSIDERATIONS
Provide psychological support and good preoperative and postoperative care to minimize complications and speed recovery.
Before a partial or total laryngectomy, take these steps:
• Instruct the patient to maintain good oral hygiene. If appropriate, instruct a male patient to shave off his beard.
• Encourage the patient to express his concerns before surgery. Help him choose a temporary nonspeaking communication method, such as writing.
• If appropriate, arrange for a laryngectomee to visit the patient. Explain postoperative procedures (suctioning, nasogastric [NG] feeding, laryngectomy tube care) and their results (breathing through the neck, speech alteration). Also, prepare the
patient for other functional losses: He won’t be able to smell, blow his nose, whistle, gargle, sip, or suck on a straw.
patient for other functional losses: He won’t be able to smell, blow his nose, whistle, gargle, sip, or suck on a straw.
STAGING LARYNGEAL CANCER
The TNM (tumor, node, metastasis) classification system developed by the American Joint Committee on Cancer describes laryngeal cancer stages and guides treatment. The T stages cover supraglottic, glottic, and subglottic tumors.
Primary tumor
TX — primary tumor unassessible
T0 — no evidence of primary tumor
Tis — carcinoma in situ
Supraglottic tumor stages
T1 — tumor confined to one subsite in supraglottis; vocal cords retain motion
T2 — tumor extends to other sites in supraglottis or to glottis; vocal cords retain motion
T3 — tumor confined to larynx, but vocal cords lose motion; or tumor extends to the postcricoid area, the pyriform sinus, or the pre-epiglottic space, and vocal cords lose motion; or both
T4 — tumor extends through thyroid cartilage or extends to tissues beyond the larynx (such as the oropharynx or soft tissues of the neck) or both
T4a — tumor invades through the thyroid cartilage or invades tissues beyond the larynx (trachea, soft tissues of neck including deep extrinsic muscle of the tongue, strap muscles, thyroid, or esophagus)
T4b — tumor invades prevertebral space, encases carotid artery, or invades mediastinal structures
Glottic tumor stages
T1 — tumor confined to vocal cords, which retain normal motion; may involve anterior or posterior commissures
T2 — tumor extends to supraglottis or subglottis or both; vocal cords may lose motion
T3 — tumor confined to larynx, but vocal cords lose motion
T4 — tumor extends through thyroid cartilage or extends to tissues beyond the larynx (such as the oropharynx or soft tissues of the neck) or both
T4a — tumor invades through the thyroid cartilage or invades tissues beyond the larynx (trachea, soft tissues of neck including deep extrinsic muscle of the tongue, strap muscles, thyroid, or esophagus) or both
T4b — tumor invades prevertebral space, encases carotid artery, or invades mediastinal structures.
Subglottic tumor stages
T1 — tumor confined to subglottis
T2 — tumor extends to vocal cords; vocal cords may lose motion
T3 — tumor confined to larynx with vocal cord fixation
T4 — tumor extends through cricoid or thyroid cartilage or extends to tissues beyond the larynx, or both
T4a — tumor invades through the thyroid cartilage or invades tissues beyond the larynx (trachea, soft tissues of neck including deep extrinsic muscle of the tongue, strap muscles, thyroid, or esophagus) or both
T4b — tumor invades prevertebral space, encases carotid artery, or invades mediastinal structures
Regional lymph nodes
NX — regional lymph nodes can’t be assessed
N0 — no evidence of regional lymph node metastasis
N1 — metastasis in a single ipsilateral lymph node, 3 cm or less in greatest dimension
N2 — metastasis in one or more ipsilateral lymph nodes, or in bilateral or contralateral nodes, larger than 3 cm but less than 6 cm in greatest dimension
N3 — metastasis in a node larger than 6 cm in greatest dimension
Distant metastasis
MX — distant metastasis unassessible
M0 — no evidence of distant metastasis
M1 — distant metastasis
Staging categories
Laryngeal cancer progresses from mild to severe as follows:
Stage 0 — Tis, N0, M0
Stage I — T1, N0, M0
Stage II — T2, N0, M0
Stage III — T3, N0, M0; T1, N1, M0; T2, N1, M0; T3, N1, M0
Stage IVA— T4, N0, M0; T4, N1, M0; Any T, N2, M0
Stage IVB — any T, N3, M0
Stage IVC — any T, any M, MI
After a partial laryngectomy, take these steps:
• Give I.V. fluids and, usually, tube feedings in the initial postoperative
period; then resume oral fluids. Keep the tracheostomy tube (inserted during surgery) in place until edema subsides.
period; then resume oral fluids. Keep the tracheostomy tube (inserted during surgery) in place until edema subsides.
• Keep the patient from using his voice until he has medical permission (usually 2 to 3 days postoperatively). Then caution him to whisper until healing is complete.
After a total laryngectomy, follow these steps:
• As soon as the patient returns to his bed, place him on his side and elevate his head 30 to 45 degrees. When you move him, remember to support his neck.
• The patient will probably have a laryngectomy tube in place until his stoma heals (about 7 to 10 days). This tube is shorter and thicker than a tracheostomy tube but requires the same care. Watch for crusting and secretions around the stoma, which can cause skin breakdown. To prevent crust formation, provide adequate room humidification. Remove crusting with petroleum jelly, antimicrobial ointment, and moist gauze.
• Teach stoma care.
• Watch for and report complications, including fistula formation (redness, swelling, secretions on the suture line), carotid artery rupture (bleeding), and tracheostomy stenosis (constant shortness of breath). A fistula may form between the reconstructed hypopharynx and the skin. This eventually heals spontaneously, but healing may take weeks or months. Carotid artery rupture usually occurs in patients who have had preoperative radiation, particularly those with a fistula that constantly bathes the carotid artery with oral secretions.
If carotid rupture occurs, apply pressure to the site; call for help immediately and take the patient to the operating room for carotid ligation.
• Tracheostomy stenosis occurs weeks to months after laryngectomy; treatment includes fitting the patient with successively larger tracheostomy tubes until he can tolerate insertion of a large one. If the patient has a fistula, feed him through an NG tube; otherwise, food will leak through the fistula and delay healing. Monitor vital signs (be especially alert for fever, which indicates infection). Record fluid intake and output, and watch for dehydration.
• Give frequent mouth care.
• Suction gently; unless ordered otherwise. Don’t attempt deep suctioning, which could penetrate the suture line. Suction through both the tube and the patient’s nose because the patient can no longer blow air through his nose; suction his mouth gently.
• After insertion of a drainage catheter (usually connected to a wound-drainage system or a GI drainage system), don’t stop suction without the practitioner’s consent. After catheter removal, check dressings for drainage.
• Give analgesics as ordered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree