Junctional Arrhythmias and AV Blocks
Overview
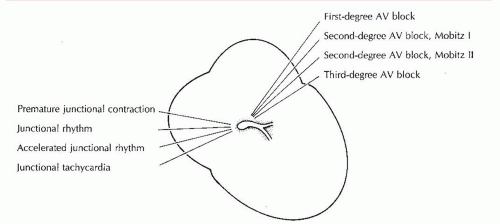
The atrioventricular (AV) node is located in the lower portion of the right atrium. The bundle of His connects the AV node to the two bundle branches. Together, the AV node and the bundle of His are called the AV junction. The AV node doesn’t contain pacemaker cells. The main function of the AV node is to slow conduction of the electrical impulse through the AV node to allow the atria to contract and complete filling of the ventricles prior to ventricular contraction. Pacemaker cells nearest the bundle of His in the AV junction are responsible for secondary pacing function. Arrhythmias originating in the AV junction are called junctional rhythms (Figure 8-1).
The inherent firing rate of the junctional pacemaker cells is 40 to 60 beats per minute. A rhythm occurring at this rate is called a junctional rhythm. Other rhythms originating in the AV junctional area include premature junctional contraction, accelerated junctional rhythm, and junctional tachycardia.
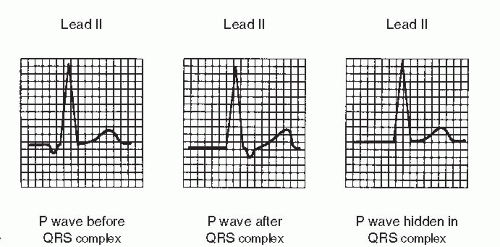
When the AV junction is functioning as the pacemaker of the heart, the electrical impulse produces a wave of depolarization that spreads backward (retrograde) into the atria as well as forward (antegrade) into the ventricles. The location of the P wave relative to the QRS complex depends on the speed of antegrade and retrograde conduction:
▪ If the electrical impulse from the AV junction depolarizes the atria first and then depolarizes the ventricles, the P wave will be in front of the QRS complex.
▪ If the electrical impulse from the AV junction depolarizes the ventricles first and then depolarizes the atria, the P wave will be after the QRS complex.
▪ If the electrical impulse from the AV junction depolarizes both the atria and the ventricles simultaneously, the P wave will be hidden in the QRS complex.
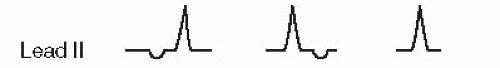
Retrograde stimulation of the atria is just opposite the direction of atrial depolarization when normal sinus rhythm is present and produces negative P waves (instead of upright) in lead II (a positive lead). The PR interval is short (0.10 second or less). The ventricles are depolarized normally, resulting in a normal duration QRS complex. Identifying features of junctional rhythms are summarized in Figure 8-2.
Premature junctional contraction
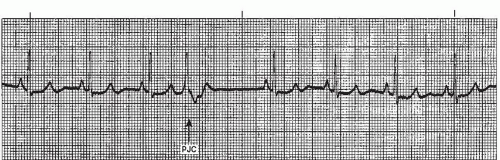
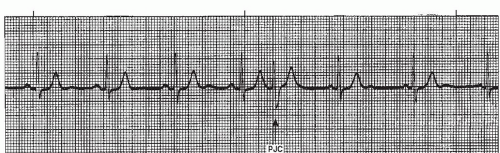
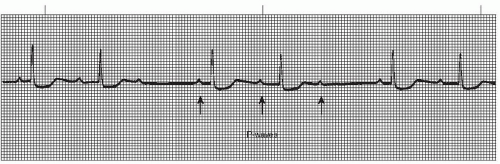
A premature junctional contraction (PJC) (Figures 8-3, 8-4, 8-5, 8-6, 8-7 and 8-8 and Box 8-1) is an early beat that originates in an ectopic pacemaker site in the AV junction. Like the premature atrial contraction (PAC), the premature junctional beat is characterized by a premature, abnormal P wave and a premature QRS complex that’s identical or similar to the QRS complex of the normally conducted beats, and is followed by a pause that is usually noncompensatory. Some differences exist, however, between the two premature beats. Because atrial depolarization occurs in a retrograde fashion with the PJC, the P wave associated with the premature beat will be negative in lead II (a positive lead). The inverted P waves will occur immediately before or after the QRS, or will be hidden within the QRS complex. The PR interval will be short (0.10 second or less). Figure 8-4 shows a PJC with the P wave before the QRS complex; Figure 8-5 shows a PJC with the P wave after the QRS complex; and in Figure 8-6 the P wave is hidden within the QRS. PJCs are less common than PACs or premature ventricular contractions (PVCs) (discussed in Chapter 9).
Box 8-1. Premature junctional contraction (PJC): Identifying ECG features
Rhythm: Underlying rhythm usually regular; irregular with PJC
Rate: That of the underlying rhythm
P waves: P waves associated with the PJC will be premature, inverted in lead II, and will occur immediately before the QRS complex, immediately after the QRS, or be hidden within the QRS
PR interval: Short (0.10 second or less)
QRS complex: Premature; normal duration (0.10 second or less)
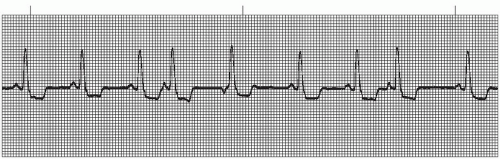
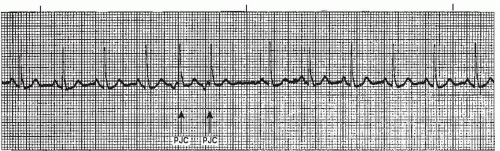
Inverted P waves in lead II may also occur with PACs arising from the lower atria, but the associated PR interval is usually normal. If difficulty is encountered in differentiating PJCs from PACs, keep the following in mind: PACs are much more common than PJCs. As a result, narrow complex premature beats are more likely to be PACs. A comparison of ectopic atrial beats and ectopic junctional beats is shown in Figure 8-7. PJCs occur in addition to the underlying rhythm. They occur in the same patterns as PACs: as a single beat; in bigeminal, trigeminal, or quadrigeminal patterns; or in pairs (Figure 8-8). A series of three or more consecutive junctional beats is considered
a rhythm (junctional rhythm, accelerated junctional rhythm, or junctional tachycardia). Differentiation of the rhythm depends on the heart rate.
a rhythm (junctional rhythm, accelerated junctional rhythm, or junctional tachycardia). Differentiation of the rhythm depends on the heart rate.
Like PACs, the premature junctional impulse may (rarely) be conducted to the ventricles abnormally (aberrantly). This results in a wide QRS complex. A PJC associated with a wide QRS complex is called a PJC with aberrancy, indicating that conduction through the ventricles is aberrant. Because of the wide QRS complex, PJCs with aberrancy must be differentiated from PVCs.
Conditions associated with PJCs include ingestion of substances such as caffeine, alcohol, or tobacco; electrolyte imbalances; hypoxia; congestive heart failure; coronary artery disease; and enhanced automaticity of the AV junction caused by digitalis toxicity (the most common cause). PJCs may also occur without apparent cause.
Frequent PJCs are best treated by correcting the underlying cause: decreasing or eliminating the consumption of caffeine, alcohol, or tobacco; correcting electrolyte imbalances; administering oxygen; treating congestive heart failure; and assessing digitalis levels. Frequent PJCs (more than 6/minute) may precede the development of a more serious junctional arrhythmia such as junctional tachycardia.
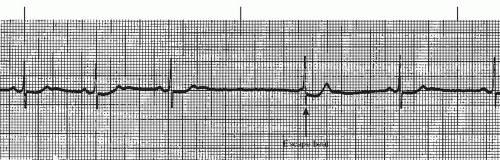
Occasionally, an ectopic junctional beat will occur late instead of early. The late beat usually occurs after a pause in the underlying rhythm in which the dominant pacemaker (usually the sinoatrial [SA] node) fails to initiate an impulse. If the ventricles are not activated by the SA node within a certain amount of time, a focus in the AV junction may “escape” and pace the heart. These are called junctional escape beats (Figure 8-9).
Junctional rhythm
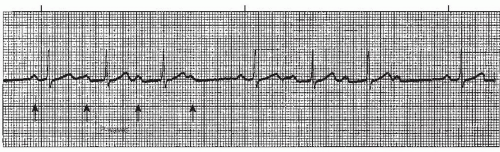
Junctional rhythm (Figures 8-10, 8-11, 8-12 and 8-13 and Box 8-2) is an arrhythmia originating in the AV junction with a rate between 40 and 60 beats per minute. Junctional rhythm is the normal rhythm of the AV junction. Junctional rhythm can occur under either of the following conditions:
▪ The heart rate of the dominant pacemaker (usually the SA node) becomes less than the heart rate of the AV junction.
 Figure 8-10. Junctional rhythm will appear as a continuous rhythm at a rate of 40 to 60 beats/minute in either of the above three patterns. |
Box 8-2. Junctional rhythm: Identifying ECG features
Rhythm: Regular
Rate: 40 to 60 beats/minute
P waves: Inverted in lead II and occurs immediately before the QRS complex, immediately after the QRS complex, or is hidden within the QRS complex
PR interval: Short (0.10 second or less)
QRS complex: Normal (0.10 second or less)
▪ Electrical impulses from the SA node or atria fail to reach the ventricles because of sinus arrest, sinus exit block, or third-degree AV block.
If the ventricles are not activated by the SA node or atria, a focus in the AV junction can “escape” and pace the heart. For this reason, junctional rhythm is commonly referred to as junctional escape rhythm.
Junctional rhythm is regular with a heart rate between 40 and 60 beats per minute. The P waves are inverted in lead II (a positive lead), and will occur immediately before or after the QRS or will be hidden within the QRS complex. The PR interval is short (0.10 second or less). The QRS duration is normal. Junctional rhythm has the same characteristics as accelerated junctional rhythm and junctional tachycardia. This rhythm is differentiated from the other junctional rhythms by the heart rate.
Junctional rhythm may be seen in acute myocardial infarction (MI) (particularly inferior-wall MI), increased parasympathetic tone, disease of the SA node, and hypoxia. It can also occur in patients taking digitalis, calcium channel blockers, or beta blockers.
The slow rate and loss of normal atrial contraction (atrial kick) secondary to retrograde atrial depolarization may cause a decrease in cardiac output. Treatment for symptomatic junctional rhythm includes following the protocols for significant bradycardia (atropine, pacing, dopamine, or epinephrine infusions to increase blood pressure). Treatment should also be directed at identifying and correcting the underlying cause of the rhythm if possible. All medications should be reviewed and discontinued if indicated.
Accelerated junctional rhythm
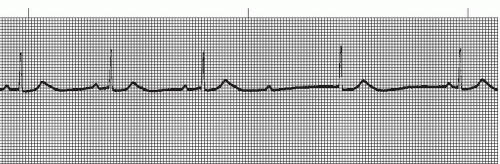
Accelerated junctional rhythm (Figures 8-14, 8-15 and 8-16 and Box 8-3) is an arrhythmia originating in the AV junction with a rate between 60 and 100 beats per minute. The term “accelerated” denotes a rhythm that occurs at a rate that exceeds the junctional escape rate of 40 to 60, but isn’t fast enough to be junctional tachycardia.
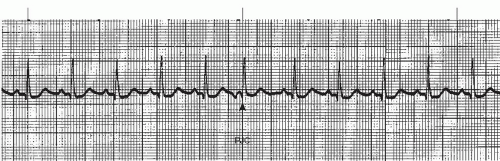
Accelerated junctional rhythm is regular with a heart rate between 60 and 100 beats per minute. The P waves are inverted in lead II (a positive lead), and will occur immediately before or after the QRS or will be hidden within the QRS complex. The PR interval is short (0.10 second or less). The QRS duration is normal. Accelerated junctional rhythm has the same characteristics as junctional rhythm and junctional tachycardia. This rhythm is differentiated from the other junctional rhythms by the heart rate. Accelerated junctional rhythm is not a common arrhythmia.
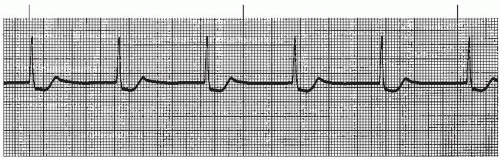
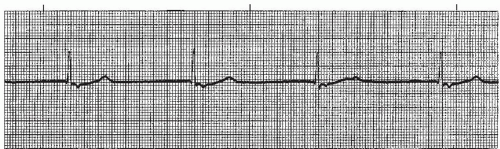 Figure 8-12. Junctional rhythm. Rhythm: Regular Rate: 33 beats/minute P waves: Inverted after QRS complex PR interval: 0.08 to 0.10 second QRS complex: 0.08 to 0.10 second. |
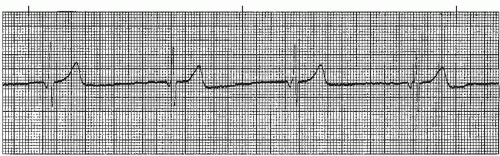 Figure 8-13. Junctional rhythm. Rhythm: Regular Rate: 35 beats/minute P waves: Inverted before the QRS PR interval: 0.06 to 0.08 second QRS complex: 0.06 to 0.08 second. |
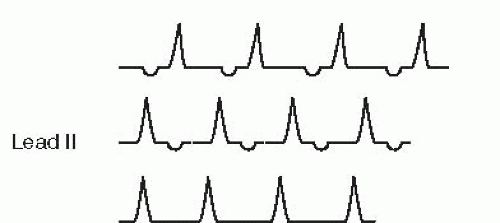 Figure 8-14. Accelerated junctional rhythm will appear as a continuous rhythm at a rate of 60 to 100 beats/minute in any of the above three patterns. |
Box 8-3. Accelerated junctional rhythm: Identifying ECG features
Rhythm: Regular
Rate: 60 to 100 beats/minute
P waves: Inverted in lead II and occurs immediately before the QRS complex, immediately after the QRS complex, or is hidden within the QRS complex
PR interval: Short (0.10 second or less)
QRS complex: Normal (0.10 second or less)
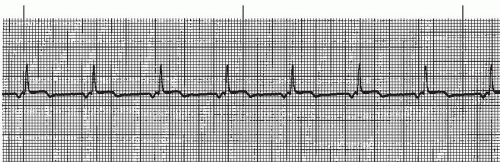
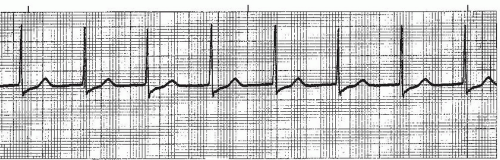 Figure 8-16. Accelerated junctional rhythm. Rhythm: Regular Rate: 68 beats/minute P waves: Hidden in QRS complex PR interval: Not measurable QRS complex: 0.06 to 0.08 second. |
Accelerated junctional rhythm may result from enhanced automaticity of the AV junction caused by digitalis toxicity (the most common cause). Other causes include damage to the AV junction from MI (usually inferior-wall MI), heart failure, and electrolyte imbalances.
Usually the heart rate associated with accelerated junctional rhythm isn’t a problem because it corresponds to that of the sinus node (60 to 100 beats per minute). Problems are more likely to occur from the loss of the atrial kick secondary to retrograde depolarization of the atria, resulting in a reduction in cardiac output. Treatment is directed at reversing the consequences of reduced cardiac output, if present, as well as identifying and correcting the underlying cause of the rhythm. All medications should be reviewed and discontinued if indicated.
Paroxysmal junctional tachycardia
Paroxysmal junctional tachycardia (PJT) (Figures 8-17 and 8-18 and Box 8-4) is an arrhythmia originating in the AV junction with a heart rate exceeding 100 beats per minute. Junctional tachycardia commonly starts and stops abruptly (like paroxysmal atrial tachycardia) and is often precipitated by a premature junctional complex. Three or more PJCs in a row at a rate exceeding 100 per minute constitute a run of junctional tachycardia.
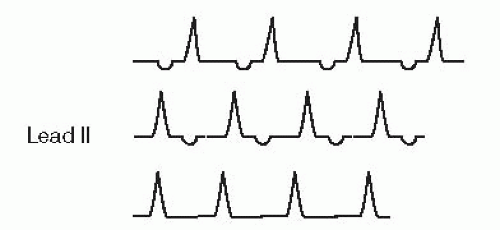 Figure 8-17. Paroxysmal junctional tachycardia will appear as a continuous rhythm at a rate exceeding 100 beats/minute in any of the above three patterns. |
Junctional tachycardia is regular with a heart rate exceeding 100 beats per minute. The P waves are inverted in lead II (a positive lead), and will occur immediately before or after the QRS or will be hidden within the QRS complex. The PR interval will be short (0.10 second or less). The QRS duration is normal. Junctional tachycardia has the same characteristics as junctional rhythm and accelerated junctional rhythm. This rhythm is differentiated from the other junctional rhythms by the heart rate. Junctional tachycardia is not a common arrhythmia.
Box 8-4. Paroxysmal junctional tachycardia: Identifying ECG features
Rhythm: Regular
Rate: Greater than 100 beats/minute
P waves: Inverted in lead II and occurs immediately before the QRS complex, immediately after the QRS complex, or is hidden within the QRS complex
PR interval: Short (0.10 second or less)
QRS complex: Normal (0.10 second or less)
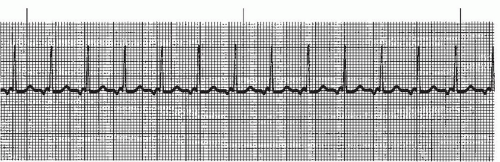 Figure 8-18. Paroxysmal junctional tachycardia. Rhythm: Regular Rate: 115 beats/minute P waves: Inverted before each QRS complex PR interval: 0.08 second QRS complex: 0.06 to 0.08 second. |
Junctional tachycardia may result from enhanced automaticity of the AV junction caused by digitalis toxicity (the most common cause). Other causes include damage to the AV junction from MI (usually inferior-wall MI) and heart failure.
Junctional tachycardia may lead to a decrease in cardiac output related to the faster heart rate as well as the loss of the atrial kick secondary to retrograde depolarization of the atria. Treatment is directed at reversing the consequences of reduced cardiac output, as well as identifying and correcting the underlying cause of the rhythm. Symptomatic junctional tachycardia may respond to diltiazem, beta blockers (use caution in patients with pulmonary disease or heart failure), or amiodarone.
AV heart blocks
The term heart block is used to describe arrhythmias in which there is delayed conduction or failed conduction of impulses through the AV node into the ventricles. Normally the AV node acts as a bridge between the atria and the ventricles. The PR interval is primarily a measure of conduction between the initial stimulation of the atria and the initial stimulation of the ventricles. This measurement is normally 0.12 to 0.20 second.
The site of pathology of the AV blocks may be at the level of the AV node, the bundle of His, or the bundle branches. When located at the level of the AV node or bundle of His, the QRS complexes will be normal duration. The QRS complex will be wide if the site of pathology is located in the bundle branches.
AV blocks are classified into first-degree, second-degree (type I and II), and third-degree. This classification system is based on the degree (type) of block and the location of the block. It is important to remember that the PR interval is the key to identifying the type of block present. The width of the QRS complex and the ventricular rate are keys to differentiating the location of the block (the lower the location of the block in the conduction system, the wider the QRS complex and the slower the ventricular rate).
In first-degree AV block (the mildest form), the electrical impulses are delayed in the AV node longer than normal, but all impulses are conducted to the ventricles. In second-degree AV block (type I and II), some impulses are conducted to the ventricles and some are blocked. The most extreme form of heart block is third-degree AV block, in which no impulses are conducted from the atria to the ventricles. The clinical significance of an AV block depends on the degree of block, the ventricular rate, and patient response.
The ability to accurately diagnose AV blocks depends on a systematic approach. The following steps are suggested:
▪ Look for the P wave. Is there one P wave before each QRS or more than one?
▪ Measure the regularity of the atrial rhythm (the P-P interval) and the ventricular rhythm (the R-R interval).
▪ Measure the PR interval. Is the PR interval consistent or does it vary? Remember, the PR interval is the key to identifying the type of AV block present.
▪ Look at the QRS complex. Is it narrow or wide?
First-degree AV block
In first-degree AV block (Figure 8-19 and Box 8-5), the sinus impulse is normally conducted to the AV node, where it’s delayed longer than usual before being conducted to the ventricles. This delay in the AV node results in a prolonged PR interval (> 0.20 second). This rhythm is reflected on the ECG by a regular rhythm (both atrial
and ventricular), one P wave preceding each QRS complex, a consistent but prolonged PR interval, and a narrow QRS complex. This conduction disorder is located at the level of the AV node (thus the narrow QRS complex) and isn’t a serious form of heart block.
and ventricular), one P wave preceding each QRS complex, a consistent but prolonged PR interval, and a narrow QRS complex. This conduction disorder is located at the level of the AV node (thus the narrow QRS complex) and isn’t a serious form of heart block.
The underlying sinus rhythm is usually identified along with the AV block when interpreting the rhythm (for example, normal sinus rhythm with first-degree AV block).
First-degree AV block may occur from ischemia or injury to the AV node or junction secondary to acute MI (usually inferior-wall MI), increased parasympathetic (vagal) tone, drug effects (beta blockers, calcium channel blockers, digitalis, amiodarone), hyperkalemia, degeneration of the conduction pathways associated with aging, and unknown causes.
First-degree AV block produces no symptoms and requires no treatment. Because first-degree heart block can progress to a higher degree of AV block under certain conditions, the rhythm should continue to be monitored until the block resolves or stabilizes. Drugs causing AV block should be reviewed and discontinued if indicated.
Box 8-5. First-degree AV block: Identifying ECG features
Rhythm: Regular
Rate: That of the underlying sinus rhythm; both atrial and ventricular rates will be the same
P waves: Sinus; one P wave to each QRS complex
PR interval: Prolonged (> 0.20 second); remains consistent
QRS complex: Normal (0.10 second or less)
Second-degree AV block, type I (Mobitz I or Wenckebach)
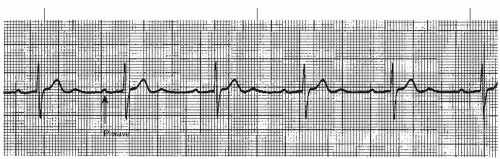
Second-degree AV block, type I is commonly known as Mobitz I or Wenckebach (for the early 20th century physician who discovered it). This rhythm (Figures 8-20, 8-21, 8-22 and 8-23 and Box 8-6) is characterized by a failure of some of the sinus impulses to be conducted to the ventricles. In Mobitz I, the sinus impulse is normally conducted to the AV node, but each successive impulse has increasing difficulty passing through the AV node, until finally an impulse does not pass through (isn’t conducted). This rhythm is reflected on the ECG by P waves that occur at regular intervals across the rhythm strip and PR intervals that progressively lengthen from beat to beat until a P wave appears that is not followed by a QRS complex, but instead by a pause. The missing QRS complex (dropped beat) causes the ventricular rhythm to be irregular. After each dropped beat the cycle repeats itself. The overall appearance of the rhythm demonstrates group beating (groups of beats separated by pauses) and is a distinguishing characteristic of Mobitz I. Escape beats (atrial, junctional, or ventricular) may occasionally occur during the pause in the ventricular rhythm, and may obscure the diagnosis because they interrupt the group beating pattern (Figure 8-22). The location of the conduction disturbance is at the level of the AV node and therefore the QRS complex will be narrow.
Box 8-6. Second-degree AV block (Mobitz I): Identifying ECG features
Rhythm: Regular atrial rhythm; irregular ventricular rhythm
Rate: Atrial: That of the underlying sinus rhythm Ventricular: Varies depending on number of impulses conducted through AV node (will be less than the atrial rate)
P waves: Sinus
PR interval: Varies; progressively lengthens until a P wave isn’t conducted (P wave occurs without the QRS complex); a pause follows the dropped QRS complex
QRS complex: Normal (0.10 second or less)
Mobitz I can be confused with the nonconducted PAC (Figure 8-23). Both rhythms have episodes where P waves are not followed by a QRS complex, but instead by a pause. To differentiate between the two rhythms, one must examine the configuration of the P waves and measure the P-P regularity. The nonconducted PAC will have an abnormal P wave and will occur prematurely. In Mobitz I, the P wave is normal and occurs on schedule, not prematurely.
Mobitz I is common following acute inferior-wall MI due to AV node ischemia. Other causes include increased parasympathetic (vagal) tone, effects of medications (digitalis, beta blockers, calcium channel blockers), and hyperkalemia. Mobitz I may also occur as a normal variant in athletes because of physiologic increase in vagal tone. Mobitz I, under certain conditions, may progress to a higher degree of AV block, but generally this is not the case. This type of AV block is usually temporary and resolves spontaneously.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree