Case Description
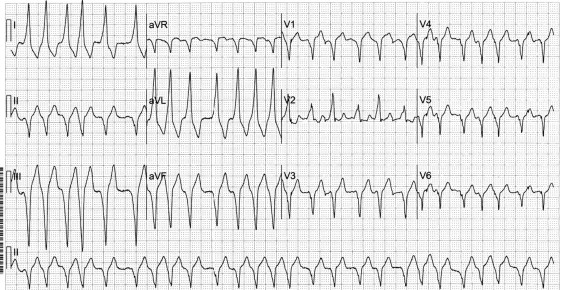
A 50-year-old asymptomatic woman is found to have a Wolff-Parkinson-White pattern of ventricular preexcitation on an electrocardiogram (ECG) which also shows sinus rhythm with frequent premature atrial complexes (PACs), including couplets ( Figure 1 ). The P-wave morphology of the PACs is different from the sinus P-wave morphology. The PACs show more ventricular preexcitation than the sinus-originating complexes. In fact, when a PAC occurs, the atrioventricular nodal conduction slows down, whereas the accessory pathway keeps a constant conduction velocity; consequently, a larger amount of ventricular myocardium gets excited through the accessory pathway. The more premature the complex, the more preexcited the QRS becomes. Also, a PAC that originates ipsilateral and in proximity to the accessory pathway shows more preexcitation than a contralateral PAC. Yet, at one point, with a further increase in prematurity, the refractory period of the accessory pathway is reached, and conduction is achieved through the slower but often less-refractory atrioventricular node (i.e., a very premature complex may not show any preexcitation).
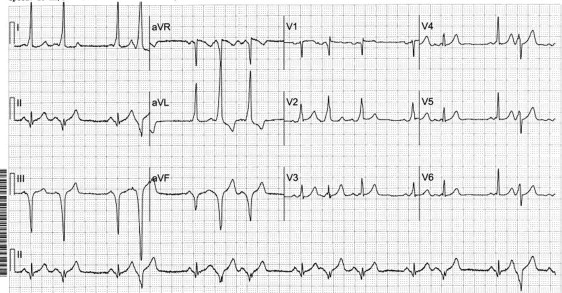
Several hours later, the patient develops atrial fibrillation producing an irregular wide-QRS tachycardia ( Figure 2 ). The shortest preexcited RR interval is ∼280 ms. An interval of ≤250 ms implies an increased risk of cardiac arrest and usually warrants accessory pathway ablation.