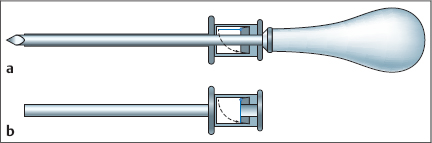
1 Introduction The Role of Medical Thoracoscopy/ Pleuroscopy in Respiratory Medicine Endoscopic procedures play an essential role in the diagnostic evaluation of patients with respiratory diseases. These techniques were mainly developed and refined during the last century. The recent tremendous advances in endoscopic technology with sophisticated instruments and telescopes with extremely high optimal resolution and small diameters, as well as developments in anesthesiology, offer a wide range of diagnostic and therapeutic possibilities. Thoracoscopy, introduced 100 years ago, is—after bronchoscopy—the second most important endoscopic technique in respiratory medicine. In the past, the vast majority of respiratory specialists (pulmonologists/pneumologists/chest physicians) performed only flexible bronchoscopy, thoracentesis, and chest tube placement. A growing number now perform medical thoracoscopy/pleuroscopy as well. Just as the art and science of flexible bronchoscopy has evolved since its introduction in the 1960s, medical thoracoscopy/pleuroscopy (MT/P) will follow as more pulmonologists, already adept and comfortable with flexible endoscopic instruments, venture to explore the pleural space with the semirigid (semiflexible) pleuroscope (“Thoracoscopy: window to the pleural space” [Colt 1999], “Pleuroscopy: a window to the pleura” [Mathur 2004]. MT/P is meanwhile considered to be one of the main areas of interventional pulmonology (Beamis and Mathur 1999; Seijo and Sterman 2001; Beamis et al. 2004; Lee et al. 2010). The definition of interventional pulmonology is the art and science of medicine related to the performance of invasive diagnostic and therapeutic procedures that require additional training and expertise beyond that required within a standard training program in respiratory medicine (Beamis and Mathur 1999). In many European countries medical thoracoscopy has already been part of the training program in respiratory medicine for many years (Dijkman et al. 1994; UEMS 1995; Loddenkemper et al. 2006; Loddenkemper et al. 2008). It has also become more popular in the United States, where according to the national survey in 1994, medical thoracoscopy was applied frequently by 5% of all pulmonary physicians (Tape et al. 1995). Although newer data are not available, the interest in the technique seems to be increasing (Lee et al. 2003; Loddenkemper 2003). However, training is lagging; in an American College of Chest Physicians (ACCP) survey of US pulmonary/critical care fellowship programs in 2002/2003, only 12% of the directors stated that MT/P was offered in their programs (Pastis et al. 2005). In the United Kingdom, where medical thoracoscopy was underutilized compared with the rest of Europe, there is also growing interest (Burrows et al. 2006; Medford et al. 2010). Meanwhile, the technique has been introduced successfully in Australia as well as in many Asian, South American, and some African countries. MT/P is an invasive technique that should be used to obtain a diagnosis only when other, simpler methods are nondiagnostic (mainly in case of pleural exudates). But, in addition to its several diagnostic advantages, it offers certain therapeutic possibilities, in particular talc poudrage, to achieve pleurodesis (in case of recurrent pleural effusion or pneumothorax) (Loddenkemper 1998; Tassi et al. 2006; Rodriguez-Panadero 2008). As with all technical procedures requiring special skills, there is a learning curve before full competence is achieved (Boutin et al. 1981a; Rodriguez-Panadero 1995). Appropriate learning is therefore mandatory (Loddenkemper 1998; Ernst et al. 2003). The technique is actually very similar to chest tube insertion by means of a trocar, the difference being that the thoracoscope/pleuroscope is introduced before the insertion of the chest tube. Thus, the whole pleural cavity can be visualized, and biopsies can be taken from all areas of the pleural cavity, including the chest wall, diaphragm, lung, and even mediastinum (Loddenkemper 1998). In general, medical thoracoscopy/pleuroscopy is easier to learn than flexible bronchoscopy if sufficient expertise in thoracentesis and chest tube placement has already been gained. When indicated, talc poudrage can be performed prior to chest tube insertion, allowing a very homogeneous distribution of talc on the visceral and parietal pleural surface. Today, this is the gold standard for nonsurgical pleurodesis (Rodriguez-Panadero and Antony 1997; Antony et al. 2000). Although medical thoracoscopy/pleuroscopy are invasive techniques, it is necessary to outline important differences in comparison with surgical thoracoscopy or video-assisted thoracic surgery, which are much more invasive and expensive, usually requiring selective double-lumen intubation under general anesthesia, multiple points of entry, disposable instruments, and an operating theater (Kaiser and Daniel 1993). Because the term is now used for both the medical and the surgical procedures, a degree of uncertainty has arisen, which may lead to unnecessary surgical interventions for what are in fact medical indications. Thus, to distinguish it better from the surgical approach, the term “medical thoracoscopy” was introduced (Mathur et al. 1994). This method is actually performed under local anesthesia or conscious sedation, via only one or two points of entry, by the respiratory physician in an endoscopy suite, using nondisposable instruments. To further clarify the difference from the surgical procedure, and to avoid confusion in the future, it has been suggested that the old term “pleuroscopy,” as used in the early French literature (Piguet and Giraud 1923), and as proposed by Weissberg (1991) for the sake of clarity, should be favored over “medical thoracoscopy.” Today, both terms are used in parallel, but often the term “medical thoracoscopy” is preferred for the technique using rigid instruments, and the term “pleuroscopy” for the technique using semirigid (semiflexible) instruments. Another alternative has been proposed in the United Kingdom, with the term “thoracoscopy for physicians” (Buchanan and Neville 2004). The added term “video-assisted” can be confusing, since this is very often associated with video-assisted thoracic surgery (VATS). However, here it actually means only that direct inspection through the thoracoscope is not used, but rather the inspection is performed indirectly by video-assisted observation, which can be employed both with the semirigid (semiflexible) pleuroscope and with the rigid thoracoscope for medical thoracoscopy. The recent development of medical and surgical thoracoscopy coincided with several technical improvements, as well as with a renewed interest in this field of respiratory medicine. This is underlined by the enormous increase in literature. In PubMed, under the terms “thoracoscopy,” “pleuroscopy,” “thoracoscopy and pleuroscopy,” and “VATS,” enormous numbers of publications (more than 8300) are cited today, demonstrating on the one hand the lack of distinction between the medical and surgical approach, and on the other hand the great interest in the technique, which has grown exponentially since the first edition of the Atlas of Diagnostic Thoracoscopy was published in 1985. Until 1982, the total world literature consisted of only approximately 240 publications relating to the clinical applications of thoracoscopy in pleuropulmonary diagnosis (Brandt et al. 1985; Loddenkemper 2004a). In conclusion, medical thoracoscopy/pleuroscopy, in our experience, is easier to learn than flexible bronchoscopy, provided that sufficient skills in thoracentesis and chest tube placement have already been acquired and the appropriate mandatory training has been accomplished. This book aims to lay the basis for learning and teaching the technique with its Manual part, explaining in depth the techniques, indications, results, contraindications, complications, etc., together with the Atlas part, showing in color endoscopic examples of different pathologies. The associated DVD demonstrates the diagnostic and therapeutic techniques of medical thoracoscopy/pleuroscopy, together with some typical case presentations. History and Development of Thoracoscopy/Pleuroscopy Thoracoscopy is based on the development of the artificial pneumothorax, of endoscopes, and of pleural drainage. It was the combination of these three essentials that led to the introduction of the technique in 1910 by Hans-Christian Jacobaeus (Fig. 1.1a, b), who worked as an internist in Stockholm, Sweden (Jacobaeus 1910). Artificial Pneumothorax The first publication describing artificial pneumothorax can be found in the Hippocratic writings. In Chapter 59 of the second book of diseases “Adhesion of the lung to the pleura,” it is stated: “If this disease (pleuritis) is caused by injury or is present in a patient with empyema as a result of a penetrating wound, one should attach an air-filled bladder to a tube and insert it. One should then take a strong instrument of tin and push. With such therapy, one should have the most luck” (Hippocrates, cited in Kapferer and Sticker 1933). Introducing air seems to indicate the establishment of pneumothorax, the little tube suggests drainage, and the tin instrument perforation of the chest wall (although the sequence is not quite clear). The bladder might have been used to catch pus or exudate in a closed system after establishing the pneumothorax. It was only in 1821 that the Scottish physiologist Carson presented the concept of an artificial pneumothorax to the Liverpool Medical Society (Carson, cited in Schmidt 1938). Based on his experiences in rabbits, Carson seems to have been the first to conceive the idea of minimizing lung scarring in tuberculosis by producing a pneumothorax in humans. Later, in 1882, Forlanini in Italy proposed a closed pneumothorax induced by means of fine, sterile needles (Forlanini 1882). He used this method for the first time in a human in 1888 in the presence of a pleural exudate, and in 1894 he produced a pneumothorax in a previously normal pleural space. For the latter, he used nitrogen because of its very slow reabsorption since he wanted to produce a prolonged therapeutic collapse of the affected lung in patients with pulmonary tuberculosis. Saugmann introduced the water manometer for the purpose of producing a controlled pneumothorax in 1902 (Saugmann 1902, cited in Schmidt 1938; Faurschou and Viskum 1997). All of these pneumothorax experiments were performed for therapeutic purposes. Fig. 1.1 Hans-Christian Jacobaeus (1879-1937). a In 1903 (courtesy of Gianpietro Marchetti). b In the 1930s. Pleural Drainage The development of pleural suction drainage for the purpose of reexpanding the lung is closely connected to closed drainage of empyemas and to the therapy for pneumothorax. Some of this was even alluded to in the Hippocratic writings. It was probably Hewitt who, in the modern era, first developed the underwater seal for pleural drainage (Hewitt 1876, cited in Enerson and McIntyre 1966) and who, in 1876, provided instructions at the London Hospital concerning “the value of the pneumatic aspirator.” The management of pleural empyema was the subject of a medical congress in Vienna in 1891, and in the same year Bülau wrote his famous article “On suction drainage in the treatment of empyema” (Bülau 1891). The large number of empyemas during the influenza epidemic in 1918 led to the recommendations of the Empyema Commission in Virginia (Empyema Commission 1918, cited in Enerson and McIntyre 1966). According to Sattler, in 1940 “there were many opinions regarding the most useful and correct measures for the treatment of pneumothorax which were confusing, lacked uniformity or were completely contradictory” (Sattler 1940). Careful thoracoscopic evaluations and studies of pleurodesis, using continuous suction, together with the development of drainage procedures following lung resection, have resulted in the current, highly developed technique of continuous closed pleural suction drainage (Roe 1958; Munnell 1997). Introduction of Thoracoscopy as a Diagnostic Method Hans-Christian Jacobaeus (1879-1937) primarily developed thoracoscopy as a diagnostic method. In 1910, he described the technique at the same time as laparoscopy in a paper entitled “On the possibility to use cystoscopy in the examination of serous cavities” (Jacobaeus 1910). At that time, as a result of the development of suitable optical systems in the nineteenth century, endoscopy was already being applied to all organs and hollow cavities with anatomical connections to the exterior (Moisiuc and Colt 2007). Recently, it has been reported that Francis-Richard Cruise, born in Dublin/Ireland in 1834, was probably the first to perform thoracoscopy as early as 1866. This was brought to light in an article entitled “Thoracoscopy before Jacobaeus” (Hoksch et al. 2002). The authors also point out that the term “thoracoscopy” was well known in several French dictionaries before Jacobaeus defined it, as “exploration of the thoracic cavity” (Larousse 1878, cited by Hoksch et al. 2002). Cruise, who in 1865 had already published on an “Endoscope as an aid to the diagnosis and treatment of disease” (Cruise 1865), performed an “Examination of interior of pleura by endoscope” in an 11-year-old girl with empyema through a pleurocutaneous fistula that had developed after pleural drainage, and he used the technique for monitoring therapy. This was reported by Samuel Gordon, who cared for this patient for about 9 months but, because of a deteriorating course, asked Cruise to help him by using his endoscopic skills (Gordon 1866). Although it was published in the Dublin Quarterly Journal of Medical Science, the technique remained anecdotal. Fig. 1.2 Title page of the 1910 publication of Jacobaeus. Fig. 1.3 Original trocar (a) and automatically closing valve (b) from Jacobaeus (1910). Jacobaeus, in his pioneer paper (published in German in the Münchener Medizinische Wochenschrift, one of the leading journals at that time) (Fig. 1.2), mentioned two cases of tuberculous pleural effusion (pleuritis exsudativa) in which he studied the pleural surfaces after replacing fluid with air according to Holmgren’s technique. Although not initially able to safely characterize the pleural changes, he expressed his confidence that the method would be successful with more training, and that it might even eventually yield prognostic information. Jacobaeus closed his publication by mentioning that he had no experience using the cystoscope in the pericardium, but that he believed that this might also eventually be possible (Jacobaeus 1910). Jacobaeus began his “Preliminary Communication” by referring to endoscopy of organs with natural openings, such as the urinary tract, and referred to the work of Max Nitze, who, in 1877, developed the first cystoscope with a telescopic lens and distal illumination (Nitze 1879). Jacobaeus then commented that closed cavities such as the peritoneum, pleura, and pericardium had not been examined endoscopically. For this kind of “cystoscopy,” Jacobaeus defined three main prerequisites: 1. The possibility to introduce a trocar (or puncture needle) into the relevant cavity without lacerating the inner organs and without causing too much pain. 2. The introduction of a transparent medium into the cavity—Jacobaeus used filtered air for this purpose. 3. A cystoscope of such small dimensions that it could be introduced through the trocar. Figure 1.3a, b shows the trocar Jacobaeus used, which contained an automatically closing valve. It was built with the assistance of Dr. A. Ahlström, chief instrument maker at Stille-Werner in Stockholm. The whole apparatus had a diameter of only 17 Charrière (1 Charrière = 0.33 mm), with the cystoscope having a diameter of 14 Charrière. Jacobaeus delineated the basic procedure as follows: The skin was disinfected and anesthetized with cocaine. Following a small skin incision, the trocar was introduced with or without prior insufflation of air into the cavity. Once the trocar was introduced, filtered air was insufflated by means of a simple Politzer air pump. The cystoscope was then introduced through the trocar, and the inspection was performed. Jacobaeus then described in detail how the peritoneum was examined. He called this “laparoscopy,” and he initially practiced it in over 50 cadavers before successfully performing the procedure in three patients. In the second, much smaller part of his discussion, Jacobaeus described in detail the examination of pleural cavities, which he called “thoracoscopy.” He stated that in this procedure the three above-mentioned main prerequisites are fulfilled more closely than in laparoscopy, especially with regard to point (1) (introduction of the trocar), which he considered to be much less dangerous in the thorax. He referred to a technique developed by Dr. Israel Holmgren, who substituted the fluid with air (“exhalation of the exudate”). He also cited Forlanini’s method, in which air or nitrogen was blown into the pleural space, and which under certain circumstances was used as a therapy for pulmonary tuberculosis. Jacobaeus mentioned that he planned to begin examination of the pleural cavity using Forlanini’s treatment method (closed pneumothorax). This eventually led to the therapeutic application of thoracoscopy, which Jacobaeus himself initiated only a few years later in 1913 (Jacobaeus 1916), to facilitate pneumothorax treatment of tuberculosis by lysis of pleural adhesions by means of thoracocautery (Jacobaeus operation). Jacobaeus therefore has to be regarded as the “father” of endoscopic procedures in serous cavities. Today, these techniques are widely used for diagnostic and therapeutic purposes by internists and surgeons. He was apparently aware neither of the above-mentioned publication in Ireland nor of the report by Georg Kelling, who worked in Dresden, Germany, which was published in 1902, also in the journal Münchener Medizinische Wochenschrift under the title “On Oesophagoscopy, Gastroscopy, and Coelioscopy” (Kelling 1902). Kelling described his experiences with laparoscopy (coelioscopy) in dogs using two ports of entry—one for a trocar through which air was insufflated and one for a trocar through which Nitze’s cystoscope was introduced. Kelling definitely did not perform thoracoscopy, as incorrectly stated by Unverricht in 1923 and later by several other authors. Use of Thoracoscopy for Diagnostic Purposes In the following years, Jacobaeus and several other European pulmonary specialists from Scandinavia, Germany, Italy, and several other European countries performed thoracoscopy for diagnostic purposes in pleural effusions, in spontaneous pneumothorax, in focal pulmonary disease, in diseases of the chest, in mediastinal tumors, as well as in anomalies of the heart and great vessels and in thoracic trauma (Brandt et al. 1985; Loddenkemper 2004b, Moisiuc and Colt 2007). Jacobaeus himself published in 1912 an extensive description of the technique and the results of (laparoscopy and) thoracoscopy, and finally in 1925 a comprehensive summary of his experiences, describing in detail his studies on the etiology and staging of tuberculous pleurisy, malignant effusion, rheumatoid effusion, empyema, parapneumonic effusion, and idiopathic pneumothorax. He divided tuberculous pleurisy into different stages, which are observations still valid to the present day. Additional insight into tuberculous pleurisy was provided by Unverricht (1931), who recognized that in many cases the spread of the disease was hematogenic. In malignant pleural effusion, Jacobaeus was often able to differentiate between primary and secondary tumors of the chest wall, pleura, lung, and mediastinum. He furthermore studied traumatic and nonspecific parapneumonic effusions. He thoracoscopically examined more than 100 cases of empyema, many of which were nontuberculous. He also appreciated that one frequently could not visualize the defect in idiopathic spontaneous pneumothorax. Figure 1.4a, b shows some drawings of endoscopic situations made by Jacobaeus. Publications from different countries appeared sporadically, emphasizing the diagnostic value of thoracoscopy in pleural effusions (15 references in Atlas of Diagnostic Thoracoscopy edited by Brandt et al. 1985), in spontaneous pneumothorax (8 references), in focal pulmonary disease (8 references), in diseases of the chest wall (5 references), in mediastinal tumors (3 references), in anomalies of the heart and great vessels (3 references), and in thoracic trauma (2 references). The highlight in the early history of diagnostic thoracoscopy was presented by Felix Cova from Italy in 1928 with his Atlas thoracoscopicon, in which most of the diseases that could be diagnosed by thoracoscopy were shown in the form of colored illustrations (Fig. 1.5a, b). Thoracoscopy as a Therapeutic Procedure in Tuberculosis (Jacobaeus Operation) Although Jacobaeus developed thoracoscopy primarily as a diagnostic procedure, it was applied during the ensuing 40 years on a worldwide scale, almost exclusively for lysis of pleural adhesions by means of thoracocautery. As briefly mentioned above, in his first publication Jacobaeus anticipated the therapeutic value of thoracoscopy and developed the technique of cauterizing the adhesions between the parietal and visceral pleura, which prevented a complete artificial pneumothorax and was the basis of the collapse therapy for tuberculosis as developed in 1882 and introduced in 1888, both by Forlanini. Jacobaeus stated that during thoracoscopy he found stringlike or membranous adhesions within the artificial pneumothorax induced for pulmonary tuberculosis. This stimulated him to work out a method to remove these pleural adhesions, a process in which “thoracoscopy finds its real practical determination” (Jacobaeus 1916). Already in 1913 he had used the technique with two different points of entry under local anesthesia. He usually introduced the thoraco scope through the patient’s back, either toward the apex or closer to the diaphragm, depending on the location of the adhesions on chest radiography performed after induction of an artificial pneumothorax (Jacobaeus 1922 a). Figure 1.6 shows Jacobaeus performing therapeutic thoracoscopy and Figure 1.7 shows the technique of thoracoscopic cauterization (“burning of membranous adhesions between the chest wall and the compressed lung”), which was the precursor of what we call today “minimally invasive surgery.” Fig. 1.4a,b Original drawings of thoracoscopic situations by Jacobaeus. (Courtesy of Gunnar Hillerdal.)


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


