1.
Continuous infusion of propofol and remifentanil is recommended for maintenance of anesthesia
2.
Pulmonary artery catheter is a useful monitoring system while the heart is in a vertical position
3.
Transesophageal echocardiography is essential in all patients unless there are contraindications
4.
The use of a warming system to maintain normothermia is important
5.
Fast-track anesthesia technique including postoperative pain management is favorable
6.
Prevention of severe atrioventricular valve regurgitation and ventricular outflow tract stenosis using conventional stabilizer and positioner is needed
7.
Trendelenburg position during Cx or RCA anastomosis is effective
6.1.4 Intraoperative Monitoring
As with most cardiac surgical procedures, monitoring of electrocardiography using leads II and V5, pulse oximeter, capnometer, and direct arterial and central venous pressure is needed. Electroencephalography such as bispectral analysis is used to monitor anesthetic depth. Core body temperature is usually monitored using pharyngeal or bladder temperature. Tympanic temperature is occasionally used for this purpose. Peripheral temperature is monitored through the surface temperature of the palm or forearm.
It has been reported that there were no significant differences in mortality and morbidity based on whether a pulmonary artery catheter monitoring is used in CABG surgery involving a cardiopulmonary bypass. In OPCAB surgery, however, a pulmonary artery catheter is often useful for monitoring abrupt increases in pulmonary arterial pressure and decreases in central venous oxygen saturation (SvO2). A pulmonary artery catheter is also needed for postoperative management in some cases [11]. Transesophageal echocardiography (TEE) is needed to evaluate mitral and tricuspid regurgitation and ventricular wall motion, as well as to diagnose narrowing of the pulmonary artery and left ventricular outflow tract. TEE is also useful for evaluating diastolic ventricular function.
In the OPCAB procedure, anastomoses are generally performed in the following order: left anterior descending coronary artery (LAD), circumflex artery (Cx), and right coronary artery (RCA).
During LAD anastomosis, SvO2 and cardiac output sometimes decrease. If pulmonary arterial pressure increases significantly, left ventricular compression and pulmonary venous obstruction should be suspected. On the other hand, low pulmonary arterial pressure indicates the possibility of right ventricular outflow tract stenosis and right heart compression. To diagnose these conditions, TEE is used to evaluate the shape and motion of the left and right ventricles.
The electrocardiographic output voltage decreases when the heart is in a vertical position during Cx or RCA anastomosis, and thus ST changes cannot be identified. Additionally, SvO2 is almost always markedly decreased when the heart is in a vertical position, reflecting a decrease in cardiac output. Decreased pulmonary arterial pressure indicates that there is a high likelihood of right ventricular outflow tract obstruction, right heart failure, or exacerbation of tricuspid regurgitation. In contrast, elevated pulmonary arterial pressure suggests left heart failure or exacerbation of mitral regurgitation. To diagnose these conditions, TEE is useful to evaluate the degree of mitral and tricuspid regurgitation.
Moreover, TEE is important for intraoperative evaluation of left ventricular diastolic function. Diastolic dysfunction and pseudonormalization are diagnosed by the evaluation of left ventricular inflow waveforms (Fig. 6.1). By combining them with measurements of tissue Doppler and pulmonary venous inflow waveforms, a more accurate diagnosis becomes possible. If the ratio of the E-wave velocity from the left ventricular inflow waveform to the tissue Doppler-derived velocity (E/e′) is ≤8, then left ventricular diastolic function is considered normal. If E/e′ is ≥15, then diastolic dysfunction is present (Fig. 6.2). Since diastolic dysfunction significantly affects cardiovascular management in OPCAB surgery, identifying diastolic dysfunction is important.
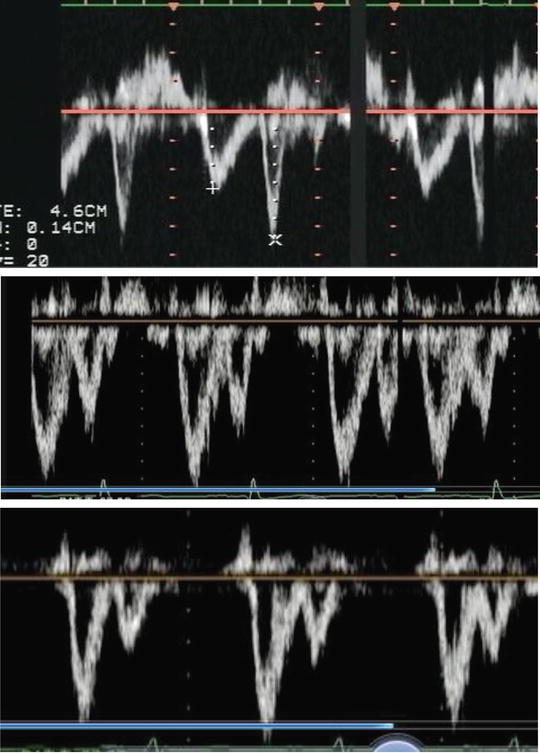
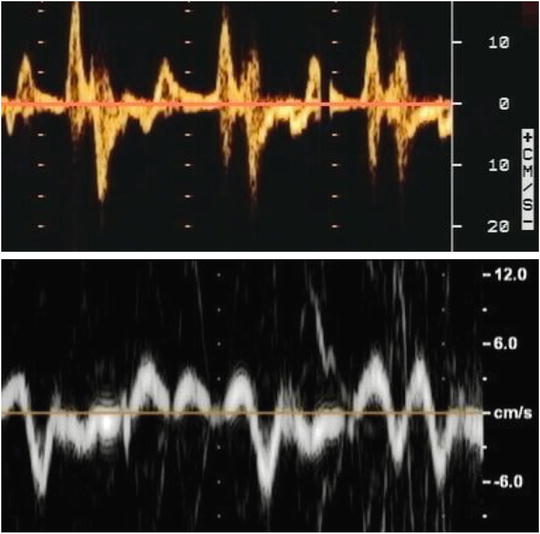
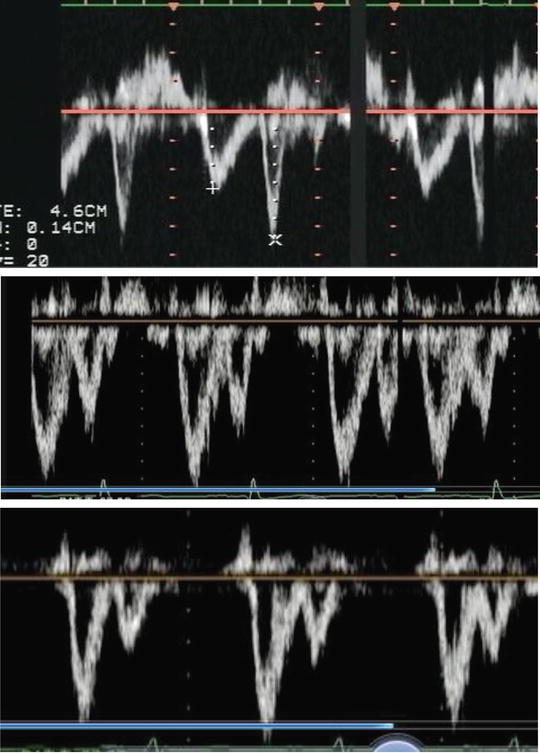
Fig. 6.1
Intraoperative left ventricular diastolic function is evaluated by transesophageal echocardiography. Mitral inflow pattern is measured using a pulse wave Doppler. (a) Abnormal relaxation pattern showed that peak E-wave is decreased and deceleration time is expanded, and peak A-wave is increased. (E/A wave ratio <1). (b) Pseudonormalization pattern showed increasing of peak E-wave and decreasing of peak A-wave. Deceleration time of E-wave is gradually reduced (E/A wave ratio >1). (c) Restrictive pattern showed high-peak E-wave. E/A wave ratio increased >2. Early diastolic pressure of left ventricle is rapidly increased
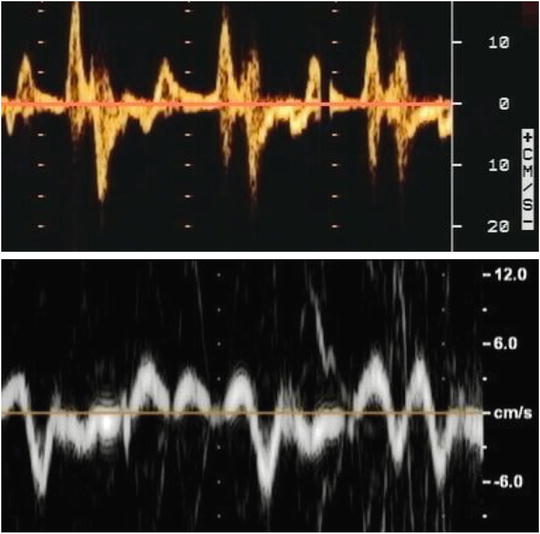
Fig. 6.2
Tissue Doppler pattern is measured at lateral mitral annulus using 4-chamber view. (a) Abnormal relaxation pattern of tissue Doppler showed increasing of a′-wave and decreasing of e′-wave. However, e′-wave remained over 8 mm/s. (b) Restrictive pattern of tissue Doppler showed decreasing of e′-wave under 8 mm/s
During OPCAB surgery, evaluation of right ventricular function is also of importance. Central venous pressure and waveforms are useful for the evaluation of the right heart. Pulmonary arterial pressure waveforms, determined using a pulmonary artery catheter, are also useful for monitoring right ventricular function. Although the evaluation of right ventricular EF with TEE is difficult because the right ventricle is not round like the left ventricle, TEE provides important information. TEE is also needed for the evaluation of right ventricular diastolic function. The myocardial performance index, which is a ratio related to the right ventricular systolic time interval, is useful for evaluating right ventricular function. For monitoring right ventricular systolic function, measurement of tricuspid annular plane systolic excursion (TAPSE) is also useful.
To monitor brain function in patients with carotid stenosis or cerebrovascular occlusion, near-infrared spectroscopy is performed.
6.1.5 Postoperative Anesthesia
After surgery, patients are generally managed in the ICU. Continuous infusion of both propofol (2–3 mg/kg/h) and dexmedetomidine (0.2–0.4 μg/kg/h) is applied for sedation. Appropriate fluid administration is needed to maintain diuresis. Once the peripheral temperature has sufficiently recovered, early extubation is attempted. Spontaneous breathing returns soon after patients are transferred to the ICU, and extubation is commonly performed within 3–6 h after surgery. In most cases, patients are discharged from the ICU the next day. Fentanyl is continuously infused to relieve postoperative pain.
6.2 Intraoperative Management
6.2.1 Intraoperative Cardiovascular Control
Following anesthetic induction, the dose of remifentanil is reduced to 0.05–0.1 μg/kg/min until the start of surgery. For patients with a decrease in systemic blood pressure, phenylephrine (0.1–0.2 mg) is administered intravenously to maintain the blood pressure. If peripheral vascular resistance declines with anesthetic induction, crystalloid solution should generally be given.
During internal thoracic artery or radial artery harvesting, fluid replacement should be sufficient to compensate for blood loss. The size of the heart, EF, and diastolic function are monitored using TEE. Mitral and tricuspid regurgitation are also evaluated. During internal thoracic artery harvesting, thoracic motion due to breathing may, in some cases, interfere with surgical manipulation. Increasing the respiratory rate to 30–50/min while decreasing tidal volume to 100–200 ml may reduce such respiratory motion.
Before the anastomosis procedure, low-dose heparin (100–150 u/kg) is infused and activated clotting time (ACT) is maintained over 250 s. During LAD anastomosis, a sling is inserted under the inferior part of the pericardium or a piece of gauze is inserted under the inferior part of the heart, and the left ventricle is lifted slightly. Compression of the LAD with a stabilizer may cause mitral regurgitation and diastolic dysfunction of both ventricles. After a small incision is made in the LAD, an intraluminal coronary shunt is inserted into the LAD coronary artery to maintain blood flow to the LAD; therefore, blood flow to the distal side of the anastomosis is maintained [8]. During end-to-side anastomosis, reducing volume overload and maintaining coronary blood flow by raising blood pressure with vasoconstrictors such as phenylephrine are recommended. The same procedure is also applied during diagonal branch anastomosis.
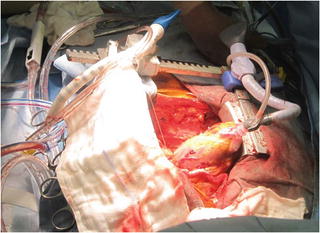
During Cx anastomosis, the patient is placed in the Trendelenburg position to increase venous return flow. The apex is pulled with a positioner so that the heart is in a vertical position (Fig. 6.3). For Cx anastomosis, torsion of the heart may exacerbate mitral and tricuspid regurgitation. Mitral and tricuspid valve regurgitation is markedly increased when the heart is in a vertical position, which reduces cardiac output remarkably [9]. When regurgitation is severe, changing the direction of the positioner and reducing the torsion may reduce regurgitation. Although compression with a stabilizer does not have a significant effect, there are negative effects on circulation when the heart is extensively twisted or vertically positioned (Fig. 6.4). Since cardiac output decreases when the heart is positioned vertically, transfusion is needed to maintain preload. Continuous infusion of vasopressors such as dopamine or noradrenaline is necessary in many cases.