5 Intracardiac Echocardiography for Common Interventions on Structural Heart Disease
Introduction
• Intracardiac echocardiography (ICE) may be performed as a collaborative effort between the echocardiographer and interventionalist, or performed solo by a skilled interventionalist or electrophysiologist during a procedure.
• It is used as an alternative to transesophageal echocardiography (TEE) in guiding complex percutaneous noncoronary interventions (Box 5-1).
• Advantages of ICE include:
• Many structures may be better visualized with ICE than on TEE, including the interatrial septum and its surrounding structures.
• ICE may reveal abnormalities not appreciated on preprocedure transthoracic echocardiography (TTE), TEE, or other radiologic studies. For example, multiple fenestrations of an atrial septal defect (ASD), deficient rim, or anomalous pulmonary veins may all be better visualized with ICE than TEE.
• Certainly, real-time three-dimensional (3D) TEE images may be better in specific circumstances, such as percutaneous mitral valve (MV) repair with the MitraClip system, but most common interventional procedures do not need this degree of imaging precision.
• 3D ICE is currently being actively developed for clinical use (Biosense Webster SoundStar 3D ICE, Diamond Bar, CA).
• This chapter reviews how to obtain images with the Biosense Webster–distributed, Siemens-manufactured popular AcuNav catheter (Siemens Medical, Mountain View, CA), a commonly used phased array transducer, for ICE guidance of interventions on the interatrial septum, including ASD and patent foramen ovale (PFO) closure, transseptal puncture, and for guiding percutaneous balloon mitral valvuloplasty.
• A nearly identical approach can be used with the St. Jude Medical ViewFlex PLUS ICE catheter (St. Jude Medical, St. Paul, MN), with the exception that this catheter only offers two directions of steering (anterior and posterior), whereas the Biosense Webster catheter offers four directions of steering (anterior, posterior, rightward, and leftward). See the later discussion on the use of these steering directions.
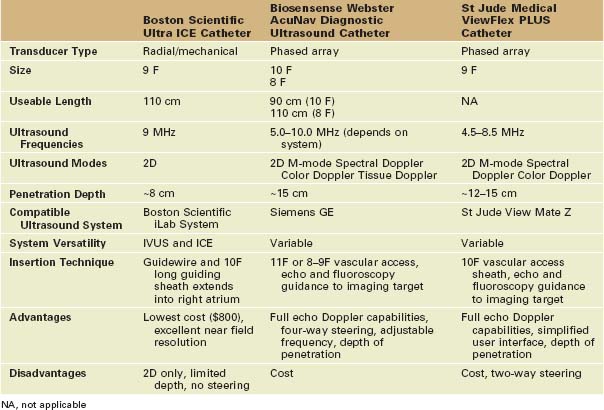
• This chapter will not address the use of radial ICE with the Boston Scientific Ultra ICE catheter (Boston Scientific, Natick, MA). This system more closely resembles an intravascular ultrasound catheter as it provides radial ICE imaging and not phased array imaging. It is not steerable, nor does it offer full Doppler capabilities. Although it is used worldwide to guide procedures, it is exclusively used by interventionalists, electrophysiologists, and surgeons, and therefore not accessible to cardiac imagers per se.
Box 5-1 Procedures Guided by Intracardiac Echocardiography
Standard Views
• The Biosense Webster AcuNav catheter creates a standard, wedge-shaped display of imaging that is identical to that seen with the phased array catheters used for standard TTE and TEE.
• It is a four-way steerable catheter, able to perform linear and Doppler measurements, and has full color Doppler flow imaging capability.
• The catheter is typically introduced into the right or left femoral vein in a neutral position and advanced into the right atrium (RA) using fluoroscopic guidance.
• The catheter may be placed in the aorta or other vascular structures that can accommodate its size.
• The catheter is then rotated clockwise in small 10- to 15-degree increments to image initially more posterior structures and flexed rightward or leftward as needed.
• The catheter also includes anterior and posterior flexion steering, allowing the catheter to move closer or away from structures, as well as “look up” (posterior deflexion, which points the imaging array more cephalad or superiorly) or “look down” (anterior deflexion, which points more caudad or inferiorly) at structures of interest.
Key Views
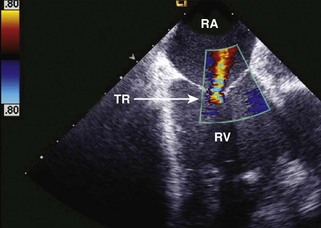
• Axially rotating the catheter to approximately 15 to 30 degrees (“home view”) images the mid-RA, tricuspid valve, right ventricle, and a short axis view of the aortic valve (Fig. 5-1). Large atrial septal aneurysms can sometimes be seen from the home view, as can many PFOs and secundum ASDs.
• The right ventricular outflow tract and pulmonic valve can be brought into view at 30 to 40 degrees of axial rotation (“right ventricular outflow tract [RVOT] view”) (Fig. 5-2).
• At 45 degrees of rotation (“left ventricular outflow tract [LVOT] view”), the left ventricle (LV) is seen in the oblique long axis, as well as a long axis view of the aortic valve. This view is often used for color Doppler evaluation of the aortic valve (Fig. 5-3) or when evaluating for a perimembranous ventricular septal defect.
• Then the catheter may be inserted more superiorly into the RA, and clockwise rotated to 60 to 70 degrees (“left atrial appendage [LAA] view” or “lower interatrial septal view”) (Figs. 5-4 and 5-5). The lower interatrial septum, left atrium (LA), left atrial appendage, MV, and an oblique view of the LV are seen in this view. This view is used for Doppler interrogation of the MV and guidance of balloon mitral valvuloplasty. If the LAA is well seen, then it may be possible to visualize medium to large thrombi.
• Typically, we enter the pulmonary artery to image the LAA when thrombus needs to be excluded definitively.
• Rotating to 90 to 100 degrees (“left pulmonary veins view”) demonstrates the left inferior and left superior pulmonary veins in long axis (Fig. 5-6A). They extend from the LA with the interatrial septum at the top of the image, an ideal view for ICE-guided pulmonary vein isolation.
• The catheter may then be flexed posteriorly and rightward to obtain the “interatrial septal long axis view” (see Fig. 5-6B). This view is ideal for ASD and PFO closure, or transseptal puncture.
• Rotating and further posterior flexing the catheter results in the “septal short axis view” (Fig. 5-7). This view demonstrates the aortic valve in short axis and the upper interatrial septum, dividing the RA and LA. The pulmonic valve is also seen. This view is comparable with the short axis view of the septum and aortic valve seen on TEE.
• With the catheter returned to neutral, it is then further clockwise rotated to produce the “right pulmonary veins view” (Fig. 5-8). Here the short axis of the right inferior and superior pulmonary veins are visualized.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree