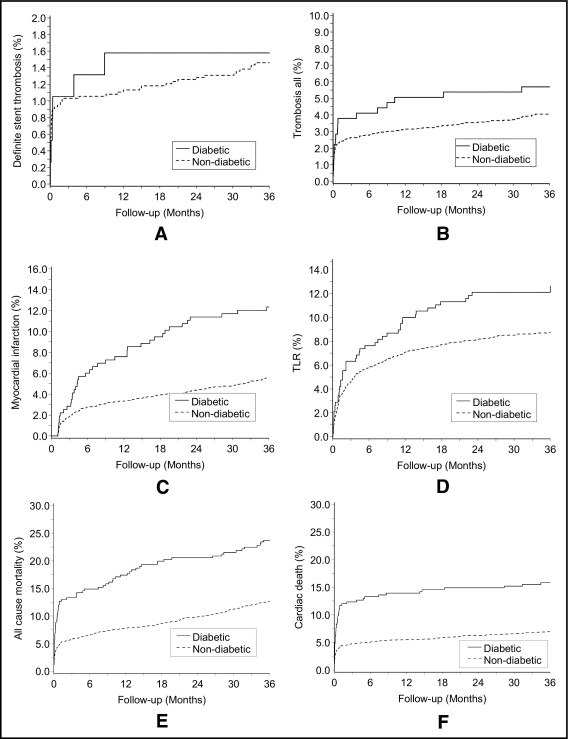
Patients with diabetes mellitus (DM) have a worse outcome after percutaneous coronary intervention (PCI) than nondiabetic patients. The purpose of this study was to compare rates of stent thrombosis, myocardial infarction (MI), target lesion revascularization (TLR), and death in diabetic and nondiabetic patients treated with primary PCI for ST-segment elevation MI (STEMI) in Western Denmark. From January 2002 through June 2005, 3,655 consecutive patients with STEMI treated with primary PCI and stent implantation (316 patients with DM, 8.6%; 3,339 patients without DM, 91.4%) were recorded in the Western Denmark Heart Registry. All patients were followed for 3 years. Cox regression analysis was used to compute hazard ratios (HRs), controlling for potential confounding. Three-year rates of definite stent thrombosis were 1.6% in the DM group and 1.5% in the non-DM group (adjusted HR 1.15, 95% confidence interval [CI] 0.50 to 2.67). The rate of MI was 12.3% in the DM group versus 5.6% in the non-DM group (adjusted HR 2.56, 95% CI 1.81 to 3.61). Rates of TLR were 12.1% in the DM group and 8.7% in the non-DM group (adjusted HR 1.55, 95% CI 1.14 to 2.11). All-cause mortality was 23.7% in patients with DM versus 12.7% in patients without DM (adjusted HR 2.03, 95% CI 1.59 to 2.59). In conclusion, stent thrombosis rate was similar in patients with and without DM and STEMI treated with primary PCI, whereas the presence of DM increased the risk of MI, TLR, and death.
Diabetes mellitus (DM) affects >180 million patients worldwide. It is present in up to 25% to 30% of all patients undergoing percutaneous coronary intervention (PCI). DM is associated with increased cardiovascular risk and mortality, and patients with DM often have a higher rate of thrombotic events and more frequently require reintervention procedures than patients without DM. Patients with type 2 DM without previous myocardial infarction (MI) have been found to have a similar mortality rate from coronary artery disease as patients without DM and previous MI in a 7-year follow-up study. In patients with ST-segment elevation MI (STEMI), primary PCI is a well-established treatment. However, the long-term prognosis remains unsatisfactory in patients with DM. Meta-analyses, randomized trials, and cohort studies have shown that, in patients with STEMI undergoing primary PCI, DM is associated with impaired perfusion, distal embolization, and higher mortality. Drug-eluting stents have shown promise in decreasing the restenosis rate in patients with and without DM. Randomized trials have shown that sirolimus-eluting stents are superior to bare-metal stents in decreasing rates of restenosis and target lesion revascularization (TLR) in patients with STEMI. The beneficial effects of paclitaxel-eluting stents in treating patients with STEMI are less well documented, with only 1 randomized trial showing a better outcome with this stent type. We used data from the Western Denmark Heart Registry to examine rates of stent thrombosis, MI, TLR, and death in a cohort study of patients with STEMI with and without DM after primary PCI with stent implantation.
Methods
The study was conducted using western Denmark’s health care databases, which cover the region’s entire population of approximately 3.0 million inhabitants (55% of Danish population). All patients were followed for 36 months. A detailed description of the databases has been reported previously.
Primary PCI for STEMI has been the recommended treatment in Denmark since the publication of results from the Danish Trial in Acute Myocardial Infarction-2 (DANAMI 2) study in 2003. To be eligible for primary PCI in Denmark at the current time, patients must meet the following criteria: (1) symptoms present <12 hours from onset of pain to time of catheterization and (2) STE (≥1 mm in ≥2 standard leads or ≥2 mm in ≥2 contiguous precordial leads) or a new left bundle-branch block. We used the Western Denmark Heart Registry to identify all primary PCIs performed from January 1, 2002 through June 30, 2005. For inclusion in the present study patients had to receive a drug-eluting stent or a bare-metal stent. Those treated with balloon angioplasty without stent implantation or with a combination of bare-metal and drug-eluting stents were excluded (n = 91, 2.4%). During the first year of the study only bare-metal stents were available. From 2003 on the preference of the PCI operator determined the selection of a drug-eluting stent or a bare-metal stent. PCI was performed according to standard practices of participating centers. A glycoprotein IIb/IIIa receptor blocker was administered at the operator’s discretion. The postintervention antiplatelet regimen included lifelong acetylsalicylic acid (75 to 150 mg 1 time/day) and clopidogrel with a loading dose of 300 mg followed by maintenance with 75 mg/day. The recommended duration of clopidogrel treatment was 3 to 12 months until November 2002 and 12 months thereafter. Patients were considered to have DM if their Western Denmark Heart Registry records indicated receipt of dietary treatment, oral antidiabetic medication, or insulin.
We computed rates of stent thrombosis (definite, probable, and possible), MI, all-cause mortality, TLR, and cardiac death. All end points were assessed within 36 months of the PCI date and ascertained from the Western Denmark Heart Registry, the Danish National Registry of Patients covering all Danish hospitals, and the Danish Registry of Causes of Death. All patients were followed for 36 months.
We defined stent thrombosis using the Academic Research Consortium definition, with a modification for probable stent thrombosis, as follows: probable stent thrombosis was defined as any unexplained death within the first 30 days after intracoronary stenting.
We defined new MIs as hospitalization for MI occurring >28 days after the index PCI. We ascertained admissions and readmissions for MI ( International Classification of Diseases, Tenth Revision codes I21 to I21.9) from the Danish National Registry of Patients and deaths from the Civil Registration System. Original death certificates were obtained from the National Registry of Causes of Death, and deaths were classified according to their underlying cause. Cardiac death was defined as any death from an evident cardiac cause, any death related to PCI, an unwitnessed death, or any death from unknown causes. From the Western Denmark Heart Registry we ascertained the occurrence of TLR, defined as a repeat PCI of the index lesion or coronary artery bypass grafting, occurring within 3 years after the index stent implantation.
We assessed all clinical end points occurring within 2 years of the index PCI. An expert committee reviewed relevant records and adjudicated end points for stent thrombosis and cause of death. For all cases of stent thrombosis we reviewed relevant medical records and catheterization films. Data on all key patient and procedure characteristics were >95% complete, and ascertainment of end points (stent thrombosis, death, MI, and TLR) was 100% complete.
From the Western Denmark Heart Registry we retrieved data on potential confounding factors for subsequent cardiovascular events including patient, procedure, and lesion characteristics. For each patient we also obtained data on all discharge diagnoses from the Danish National Registry of Patients. We then computed co-morbidity scores using the Charlson Co-morbidity Index, which covers 19 major disease categories including heart failure, cerebrovascular diseases, and cancer. The index value is a weighted summary of diagnoses, with each weight calculated based on 1-year mortality associated with each disease in the original Charlson dataset.
Distributions of continuous variables in the 2 groups were compared using 2-sample t test or Mann–Whitney test depending on whether the data followed a normal distribution. Continuous variables were summarized as median and interquartile range (twenty-fifth to seventy-fifth percentiles) or mean ± 1 SD depending on whether the data followed a normal distribution.
We counted end-point events that occurred during the follow-up period and compared their rates for the cohort of patients with DM to the cohort without this condition. Follow-up began on the date of the index PCI procedure. In analyses with stent thrombosis as the outcome, follow-up continued until the date of definite stent thrombosis, death, or until 36 months after implantation, whichever came first. In analyses with death as the outcome, follow-up continued until the date of death or until 36 months after implantation. In analyses with MI as the outcome, follow-up continued until the date of MI, death, or until 36 months after implantation.
We constructed Kaplan–Meier curves for patients with and without DM and used the life-table method to compute the 3-year rate for each end point (proportion of population at risk for outcome of interest). Cox proportional-hazards regression was used to compute hazard ratios (HRs) as estimates of the relative risk for each end point. Because the hazards were not proportional throughout the follow-up period, we computed HR estimates within separate time windows. The HR in these analyses reflected the risk in patients alive and at risk of the specific end point at the start of each period (e.g., after 30 days or 1 year of follow-up). We controlled for age, gender, stent type (bare-metal stent or drug-eluting stent), and procedure time in all regression analyses. Also, we controlled for the co-morbidity index (100% complete data for all cases), whereas further variables listed in Table 1 were not used in the adjusted analysis because of a substantial number of missing data. To improve the precision of risk estimates, we used the change-in-estimate method, which entailed retaining variables that changed relative risk estimates for an outcome by >10%. The number of variables included in the final regression models varied from 0 to 3. Thus, in lesion-specific analyses (stent thrombosis and TLR) we also adjusted for glycoprotein IIb/IIIa receptor blockers, stent length, and reference vessel size. All statistical analyses were performed using SAS 9.2 (SAS Institute, Cary, North Carolina).
| Variable | Diabetes Mellitus | p Value | |||
|---|---|---|---|---|---|
| Yes | Valid Cases | No | Valid Cases | ||
| (n = 316) | (n = 3,339) | ||||
| Men | 217 (68.7%) | 316 | 2,451 (73.4%) | 3,339 | 0.07 |
| Age (years) ⁎ | 64 (56–72) | 316 | 63 (54–73) | 3,339 | 0.61 |
| Smoker | 107 (46.1%) | 232 | 1,484 (57.0%) | 2,604 | 0.0014 |
| Body mass index (kg/m 2 ) ⁎ | 28.0 (24.8–32.0) | 102 | 26.0 (23.9–28.7) | 1,233 | <0.0001 |
| Hypertension | 125 (50.2%) | 249 | 668 (24.9%) | 2,688 | <0.001 |
| Previous coronary artery bypass grafting | 6 (2.3%) | 256 | 42 (1.5%) | 2,800 | 0.30 |
| Previous percutaneous coronary intervention | 18 (7.4%) | 243 | 102 (3.9%) | 2,597 | 0.0099 |
| Previous myocardial infarction | 48 (19.9%) | 241 | 329 (12.6%) | 2,603 | 0.0014 |
| Lipid-lowering therapy | 70 (28.2%) | 248 | 326 (12.2%) | 2,683 | <0.001 |
| Glycoprotein IIb/IIIa receptor blocker | 198 (74.7%) | 265 | 1,967 (72.6%) | 2,710 | 0.46 |
| Co-morbidity index score | 316 | 3,339 | <0.001 | ||
| 0 | 181 (57.3%) | 2,424 (72.6%) | |||
| 1–2 | 116 (36.7%) | 769 (23.0%) | |||
| ≥3 | 19 (6.0%) | 146 (4.4%) | |||
Results
In total 3,655 patients with STEMI (with 4,356 lesions) treated with primary PCI and stenting were followed for 36 months. Of these, 316 patients (8.6%) with 380 lesions had DM, whereas 3,339 patients (91.4%) with 3,976 lesions did not have DM. Patients’ median age was 63 years (interquartile range 54 to 73) and 30.9% of patients were >75 years old. DM was associated with a higher prevalence of hypertension, hypercholesterolemia, previous MI, previous PCI, and a higher co-morbidity index score ( Table 1 ). The number of patients treated with a drug-eluting stent was 748; of these 82 patients (10.9%) had DM and 666 patients (89.0%) did not have DM. Preprocedural Thrombolysis In Myocardial Infarction flow did not differ significantly between patients with and those without DM, but fewer patients with DM achieved a final postprocedure Thrombolysis In Myocardial Infarction grade 3 flow ( Table 2 ).
| Variable | Diabetes Mellitus | p Value | |||
|---|---|---|---|---|---|
| Yes | Valid Cases | No | Valid Cases | ||
| Number of lesions | 380 | 380 | 3,976 | 3,976 | |
| Infarct-related coronary artery | 380 | 3,975 | 0.83 | ||
| Left anterior descending | 160 (42.1%) | 1,721 (43.6%) | |||
| Left circumflex | 58 (15.3%) | 545 (13.7%) | |||
| Right | 156 (41.1%) | 1,643 (41.3%) | |||
| Left main | 6 (1.6%) | 55 (1.4%) | |||
| Preintervention Thrombolysis In Myocardial Infarction flow grade | 377 | 3,927 | 0.76 | ||
| 0 | 196 (51.5%) | 2,174 (54.7%) | |||
| 1 | 28 (7.4%) | 235 (5.9%) | |||
| 2 | 59 (15.6%) | 529 (13.3%) | |||
| 3 | 97 (25.6%) | 1,038 (26.1%) | |||
| Lesion length (mm) | 13.0 (10.0–20.0) | 372 | 14.0 (10.0–18.0) | 3,863 | 0.77 |
| Reference segment (mm) | 3.2 (3.0–3.6) | 361 | 3.5 (3.0–3.8) | 3,783 | <0.0001 |
| Minimum lumen diameter (mm) | 0 (0–0.20) | 360 | 0 (0–0.20) | 3,738 | 0.96 |
| Diameter stenosis (%) | 100 (95–100) | 377 | 100 (95–100) | 3,927 | 0.99 |
| Saphenous vein graft | 0 (0.0%) | 380 | 20 (0.5%) | 3,976 | 0.13 |
| Stent length (mm) | 16.0 (13.0–23.0) | 370 | 18.0 (13.0–23.0) | 3,883 | 0.26 |
| Stent number | 378 | 3,963 | 0.20 | ||
| 1 | 313 (82.8%) | 3,280 (82.8%) | |||
| 2 | 55 (14.8%) | 561 (14.2%) | |||
| ≥3 | 10 (2.6%) | 122 (3.1%) | |||
| Drug-eluting stent | 100 (26.3%) | 380 | 845 (21.3%) | 3,976 | 0.02 |
| Maximum balloon pressure (atm) | 15.0 (13.0–18.0) | 374 | 15.0 (12.0–18.0) | 3,956 | 0.53 |
| Maximum balloon diameter (mm) | 3.4 (3.0–3.8) | 371 | 3.5 (3.2–3.9) | 3,918 | 0.0005 |
| Final Thrombolysis In Myocardial Infarction flow grade | 377 | 3,927 | <0.001 | ||
| 0 | 11 (2.9%) | 31 (0.8%) | |||
| 1 | 4 (1.1%) | 35 (0.9%) | |||
| 2 | 43 (11.4%) | 265 (6.7%) | |||
| 3 | 322 (84.7%) | 3,645 (91.7%) | |||
| Procedure time (minutes) | 22.0 (15.0–33.0) | 301 | 23.0 (15.0–33.0) | 3,252 | 0.68 |
| Fluoroscopic time (minutes) | 6.8 (4.3–11.3) | 308 | 6.5 (4.0–10.6) | 3,291 | 0.50 |
| Contrast (ml) | 100.0 (80.0–175.0) | 306 | 110.0 (80.0–180.0) | 3,288 | 0.26 |
Three-year rates of definite stent thrombosis were 1.6% in patients with DM (n = 6, 2 drug-eluting stents, 4 bare-metal stents) and 1.5% in patients without DM (n = 58, 22 drug-eluting stents, 36 bare-metal stents). Adjusted HR was 1.15 (95% confidence interval [CI] 0.50 to 2.67). Definite stent thrombosis occurred within 1 week in 34 patients (0.9%). Of these 2 had DM (0.5%) and 32 did not have DM (0.8%). Definite stent thrombosis occurred within 30 days in 41 patients (64%). Of these 4 had DM (1.1%) and 37 did not have DM (0.9%). Median time to occurrence of definite stent thrombosis was 6.4 days (interquartile range 1.8 to 275.8). Rates of acute, subacute, and late definite stent thrombosis were also similar in the 2 groups ( Figure 1 ) . Very late definite stent thrombosis was not seen in patients with DM but occurred in 14 patients without DM (0.4%; Table 3 , Figure 1 ). Cumulative rate of stent thrombosis over time showed an initial steep increase followed by a slight almost linear increase up to 36 months in nondiabetic patients.