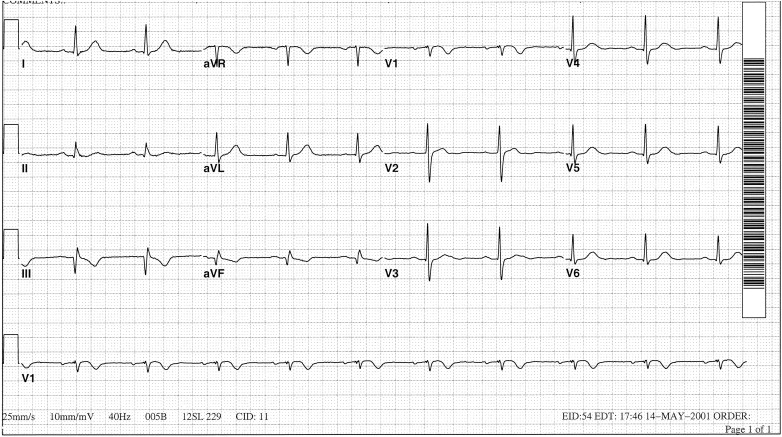
The electrocardiogram (ECG) in Figure 1 is that of an 80-year-old woman and is unchanged from an ECG recorded 16 months earlier. The rhythm is sinus at a rate of 76 beats/minute. Left axis deviation with a frontal plane QRS axis of −42° and left bundle branch block are present. Do Q waves in leads III and aVF represent old inferior myocardial infarction?
In patients with acute chest pain and left bundle branch block, repolarization changes often are helpful in confirming acute myocardial infarction. Diagnosing old myocardial infarction in the presence of left bundle branch block is a tougher assignment. In this regard, the presence of Q waves in leads usually devoid of them in patients with left bundle branch block has received considerable attention. For example, in the presence of left bundle branch block, pathologic Q waves in the left lateral leads (I, aVL, V 5 , and V 6 ) or a Q in lead V 6 with a prominent R wave in lead V 1 are insensitive but specific markers of an infarct, not in the lateral portion of the left ventricle but in its anteroseptal region.
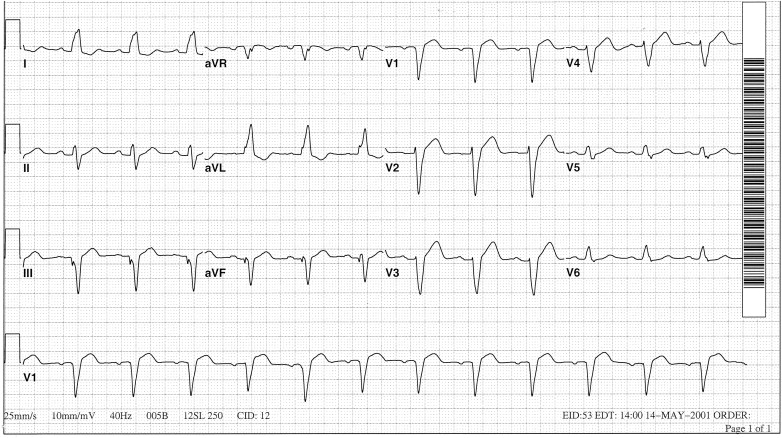
Horan et al reported that diagnostic inferior Q waves in patients with left bundle branch block were highly specific but insensitive indicators of an inferior myocardial infarct. They did so both before and after Timmis et al challenged the thesis on the basis of 5 patients in whom QS waves disappeared when the ventricular conduction pattern spontaneously changed from left bundle branch block to normal. When our patient’s left bundle branch block spontaneously disappeared later the same day, probably as a result of the sinus rate’s slowing from 76 to 60 beats/minute, pathologic Q waves persisted in leads III and aVF and were accompanied by inverted T waves ( Figure 2 ). Thus, in her, the Q waves in both ECGs shown here and the one 16 months earlier represented an inferior myocardial infarct.