39 Infective Endocarditis
Clinical Presentation
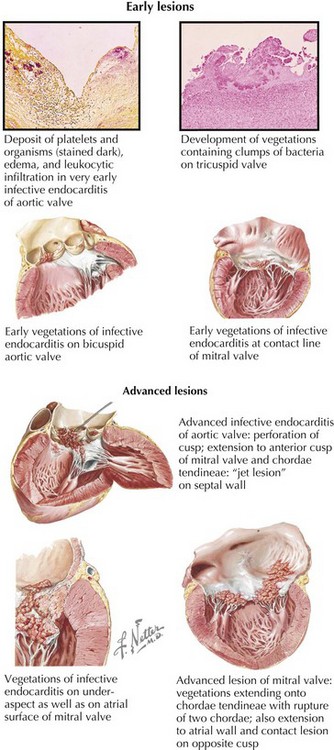
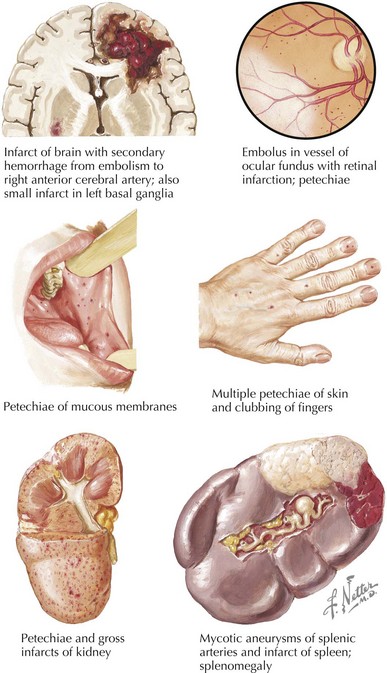
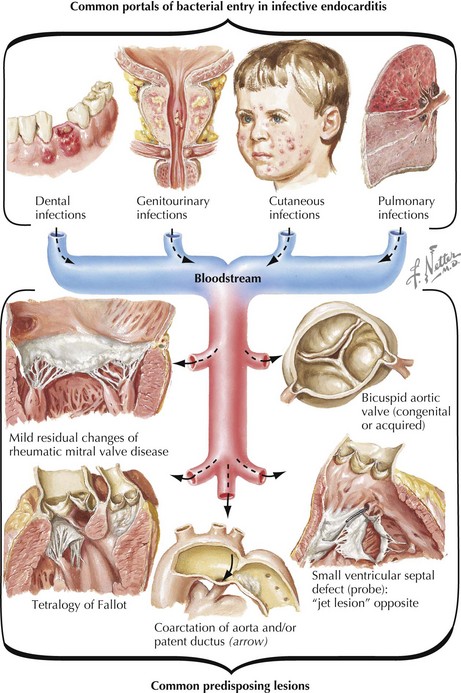
Any organ system can be involved in patients with IE, and thus the clinical presentation is highly variable. Four processes contribute to IE’s clinical manifestations: (1) the infectious process on the valve causing local intracardiac complications (e.g., perivalvular abscess, incompetent valve, conduction disturbances, congestive heart failure [CHF]) (Fig. 39-1); (2) vascular phenomena (e.g., septic pulmonary or arterial emboli, mycotic aneurysm, intracranial hemorrhage); (3) bacteremic seeding of remote sites (e.g., osteomyelitis, psoas or perirenal abscess) (Fig. 39-2); and (4) immunologic phenomena (e.g., glomerulonephritis, Osler’s nodes, Roth’s spots, positive rheumatoid factor, and antinuclear antibodies).
Frequently the diagnosis can be made clinically if a careful physical examination is performed. Attention should be given to the conjunctiva (hemorrhages), dilated fundoscopic exam (Roth’s spots), complete cardiovascular examination (new or changing murmur, especially aortic, mitral or tricuspid regurgitation, and signs of CHF), splenomegaly, and extremities (splinter hemorrhages, septic emboli, Janeway’s or Osler’s nodes) (Fig. 39-3). The comprehensive physical examination can be complemented by several nonspecific, yet suggestive laboratory studies. Findings in IE include (but are not limited to) anemia, thrombocytopenia, leukocytosis, active urinary sediment, elevated sedimentation rate, hypergammaglobulinemia, positive rheumatoid factor, antinuclear antibodies, hypocomplementemia, and false-positive Venereal Disease Research Laboratory and Lyme disease serology.