Infective Endocarditis
Tracy Zivin-Tutela
Bruce Polsky
Infective endocarditis (IE) is a disease that is associated with significant morbidity and mortality. Antimicrobial resistance among common bacterial pathogens has created management issues for physicians.
The three major bacterial causes of IE are streptococci, staphylococci, and enterococci. Staphylococcus aureus has now surpassed Streptococcus viridans as the leading cause of bacterial endocarditis in the United States.1,2 and 3 We are also now faced with multi drug-resistant S. viridans and oxacillin-resistant S. aureus (community acquired as well as health care associated).4,5 and 6 The development of intermediate and high-level resistance to vancomycin has also been documented. Vancomycin and aminoglycoside resistance among enterococci is also a common finding in health-care-associated infections.7
DIAGNOSIS
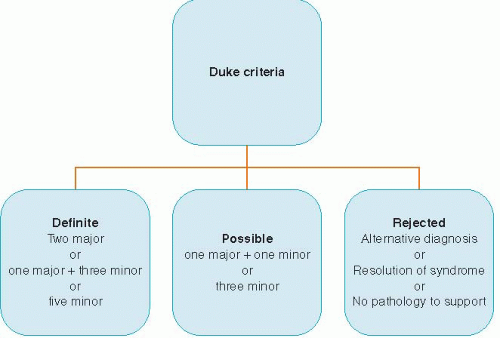
The classic clinical manifestation of IE includes bacteremia or fungemia, acute valvulitis, immunologic phenomena, and peripheral emboli. Immunologic and vascular phenomena are a more common presentation in subacute IE. Right-sided endocarditis may also present with septic pulmonary emboli. The modified Duke criteria were developed to aid in the diagnosis of IE.8 It stratifies patients with suspected endocarditis into “definite,” “possible,” and “rejected.” Definite IE includes microorganisms demonstrated by culture or histopathology of vegetation, vegetation that has embolized or an intracardiac abscess, or two major criteria, or one major and three minor criteria, or five minor criteria. Possible IE includes one major criterion and one minor criterion, or three minor criteria. Rejected diagnosis of endocarditis includes an alternative diagnosis or resolution of IE syndrome with antibiotic therapy for <4 days or no pathological evidence at time of surgery or autopsy.
THE MAJOR AND MINOR CRITERIA OF THE DUKE CRITERIA
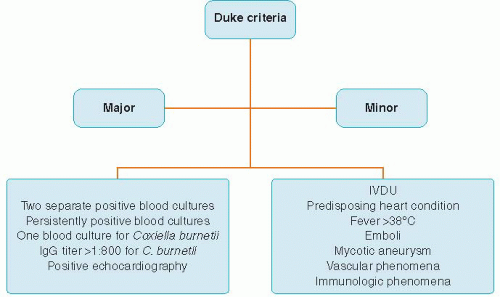
The major criteria include the following (Figure 26.2):
Positive blood culture from two separate blood cultures with typical organisms for IE
Persistently positive blood cultures
Single positive blood culture for Coxiella burnetii or IgG antibody titer >1:800
Echocardiogram positive for oscillating intracardiac mass on valve or supporting structures or on implanted material in the absence of an alternative anatomic explanation or abscess or new partial dehiscence of prosthetic valve or new valvular regurgitation.
The minor criteria include the following:
Predisposing heart condition or intravenous drug use
Fever >38°C
Vascular phenomena, arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhage, or Janeway lesions
Immunologic phenomena such as glomerulonephritis, Osler’s nodes, Roth’s spots, and rheumatoid factor
Microbiologic evidence such as a blood culture that does not meet a major criterion
THE USE OF ECHOCARDIOGRAPHY IN INFECTIVE ENDOCARDITIS
DIAGNOSIS AND MANAGEMENT WITH ECHOCARDIOGRAPHY: TTE VERSUS TEE
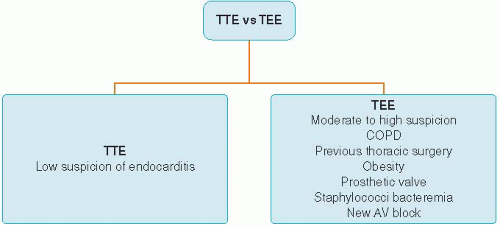
All suspected cases of IE should undergo an echocardiogram. If the clinical suspicion is low then it is reasonable to perform a transthoracic echocardiogram (TTE; Figure 26.3). In a patient with chronic obstructive pulmonary disease, previous thoracic surgery, obesity, or moderate-to-high clinical suspicion for IE, a transesophageal echocardiogram (TEE) should be performed. Moreover, patients with prosthetic valves, staphylococcal bacteremia, or new atrioventricular block should have a TEE performed first, as a TTE will definitely not rule out endocarditis.9,10 and 11 TEE has been shown to be more sensitive than TTE for the detection of vegetations and abscesses.12 TEE has also been shown to be cost-effective as the first examination in those with moderate-to-high clinical suspicion of endocarditis. False negative results of echocardiography may occur if vegetations are small or have already embolized. Perivalvular abscess may be missed as well in the patient’s early illness. Therefore, repeat echocardiography may be essential several days later. An echocardiogram should be done at the completion of therapy for endocarditis to establish a new baseline for valve function as well as ventricular size and function.
TREATMENT OF ENDOCARDITIS
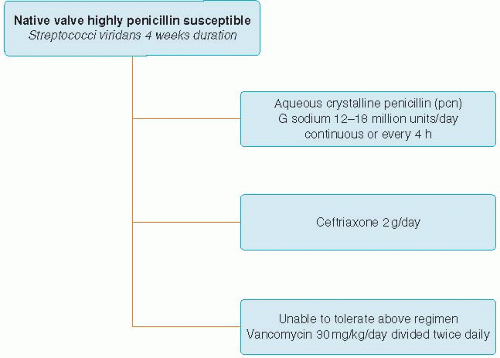
TREATMENT OF STREPTOCOCCI VIRIDANS ENDOCARDITIS
Aqueous crystalline penicillin (pcn) G sodium 12 to 18 million units per day continuous or every 4 hours for 4 weeks duration (Figure 26.4) or
Ceftriaxone 2 g per day for a 4-week duration
Vancomycin 30 mg/kg/day divided twice daily for 4 weeks for those unable to tolerate the above antibiotics
A 2-week regimen can be done if there is no evidence of cardiac or extracardiac abscess or evidence of decreased renal
function. However, addition of gentamicin at 3 mg/kg/day in one dose should be added for the entire 2 weeks.
function. However, addition of gentamicin at 3 mg/kg/day in one dose should be added for the entire 2 weeks.
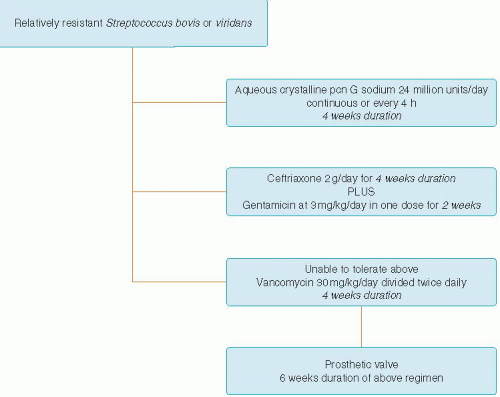
TREATMENT OF RELATIVELY RESISTANT STREPTOCOCCUS BOVIS OR VIRIDANS ENDOCARDITIS
Relatively resistant Streptococcus bovis or viridians group.
Aqueous crystalline pcn G sodium 24 million units per day continuous or every 4 hours for a 4-week duration (Figure 26.5)
or
Ceftriaxone 2 g per day for a 4-week duration plus gentamicin at 3 mg/kg/day in one dose for 2 weeks
Vancomycin 30 mg/kg/day divided twice daily for 4 weeks for those unable to tolerate the above antibiotics.
Prosthetic valve endocarditis viridans group streptococci.
Above regimens for a 6-week duration of therapy.
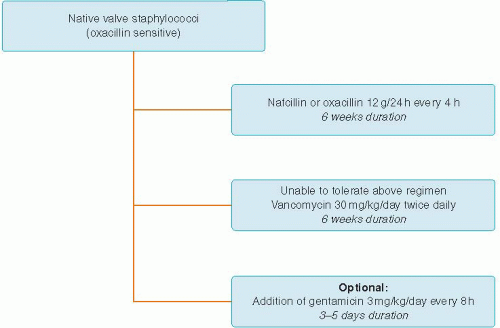
TREATMENT OF NATIVE VALVE STAPHYLOCOCCI OXACILLIN-SENSITIVE ENDOCARDITIS
Staphylococci endocarditis without prosthetic involvement.
Nafcillin or oxacillin 12 g per day divided equally every 4 hours for 6 weeks (Figure 26.6)
Optional addition of gentamicin 3 mg/kg/day divided in two or three equal doses for 3 to 5 days16
Vancomycin 30 mg/kg/day divided twice daily for those unable to tolerate the above antibiotics for 6 weeks.
TREATMENT OF NATIVE VALVE STAPHYLOCOCCI OXACILLIN-RESISTANT ENDOCARDITIS
Oxacillin resistant strains.
Vancomycin 30 mg/kg/day divided twice daily for 6 weeks or daptomycin 6 mg/kg/day (not FDA-approved for left-sided endocarditis; Figure 26.7).
TREATMENT OF PROSTHETIC VALVE STAPHYLOCOCCI ENDOCARDITIS
Staphylococci endocarditis with prosthetic involvement.
Nafcillin or oxacillin 12 g per day divided equally every 4 hours plus rifampin 900 mg per day divided in three equal doses for at least 6 weeks




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree