Indirect Physiologic Assessment of Lower Extremity Arteries
Gregory L. Moneta
Molly J. Zaccardi
The noninvasive vascular laboratory, in combination with the history and physical examination, plays a critical role in providing objective diagnosis of lower extremity arterial occlusive disease. In many patients, the clinical history and physical examination are all that is necessary to establish a diagnosis of lower extremity intermittent claudication or ischemic rest pain. Almost all such patients will have diminished or absent lower extremity pulses. Palpation of pulses is, however, subjective and poorly reproducible. Therefore, the pulse examination in a patient suspected of having arterial occlusive disease should be supplemented with objective testing in the noninvasive vascular laboratory. Occasionally, a patient will give a history suggesting intermittent claudication yet will have what appear to be normal resting pedal pulses. In this setting, evaluating the response of the ankle systolic pressure to walking exercise is crucial to confirm the diagnosis of intermittent claudication.
Many patients with peripheral arterial disease (PAD) have atypical leg symptoms or are asymptomatic, and these individuals have an increased risk of cardiovascular death similar to that of patients with typical intermittent claudication symptoms. Awareness of these patients has resulted in a renewed interest in screening for the presence of PAD in patients with atypical leg symptoms or atherosclerotic risk factors. Patients with exercise-induced lower extremity or buttock pain should be asked about the location of the pain, its relationship to walking, severity and duration of symptoms, and progression of symptoms over time. Only exercise-induced muscular pain of the calf, thigh, or buttock, relieved within a few minutes of rest and reproduced by additional walking, can be reliably improved by lower extremity arterial revascularization. There are no data on the response of atypical leg symptoms to revascularization in patients with evidence of PAD.
Ischemic rest pain is suspected when a patient complains of pain or numbness in the forefoot, toes, or instep in the resting state. This pain pattern is typically aggravated by elevating the extremity and improved by placing the limb in a dependent position, most likely due to the effect of gravity on hydrostatic pressure and dilatation of collateral vessels. It is also worsened by leg exercise, because patients with ischemic rest pain are clearly at risk for intermittent claudication whenever they walk. Nocturnal leg cramps are generally not manifestations of ischemic rest pain. However, true ischemic rest pain is often worse at night, and some patients seek relief by sleeping in a chair with their legs dependent. As a result, these patients with chronic ischemic rest pain develop profound edema of the symptomatic extremity. This edema is not directly related to arterial insufficiency, but rather to prolonged dependency. Patients with ischemic rest pain will also frequently have thin, atrophic skin on the foot and lower leg, and they exhibit pallor with elevation and rubor with dependency of the foot. Gangrene and ulceration may develop or may be the initial presenting symptoms.
The overall purpose of the vascular laboratory in patients with known or suspected lower extremity PAD is to confirm the presence of arterial insufficiency, provide quantitative and reproducible physiologic data concerning its severity, and document the location and hemodynamic significance of individual arterial lesions. With the exception of determining hemodynamic significance of individual arterial lesions, nonimaging physiologic testing can be used to confirm the presence of arterial disease and provide a very good estimation of disease location.
Lower extremity arterial testing is the one testing area in the vascular laboratory in which nonimaging or indirect physiologic methods are still widely used and provide valuable clinical information. The two categories of nonimaging physiologic testing methods for lower extremity arterial occlusive disease are plethysmography and Doppler ultrasound.
PLETHYSMOGRAPHY
Plethysmography is based on the detection of limb volume changes in response to arterial inflow and venous outflow. In addition to assessing volume flow, this method can be used to measure digit pressures and record pulse volume waveforms. Mercury strain-gauge plethysmography, air plethysmography, and photoplethysmography (PPG) are examples of plethysmographic techniques used clinically.
Volume Flow
Calf or foot blood flow can be recorded with a mercury-in-Silastic strain gauge. The electrical resistance of the mercury column depends on the length of the gauge, and when the gauge is wrapped around the limb, small changes in gauge length are proportional to changes in the volume of the extremity. However, there are typically no significant differences in resting calf or foot blood flow between normal subjects and patients with intermittent claudication, even when the symptoms are severe.1 Hyperemic volume flow is often lower in limbs of patients with arterial occlusive disease, but reactive hyperemia testing can be quite painful for the patient.2 Therefore, measurements of volume flow are not very useful in the clinical evaluation of lower extremity ischemia.
Pulse Volume Recording
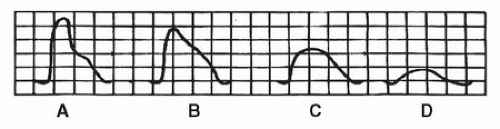
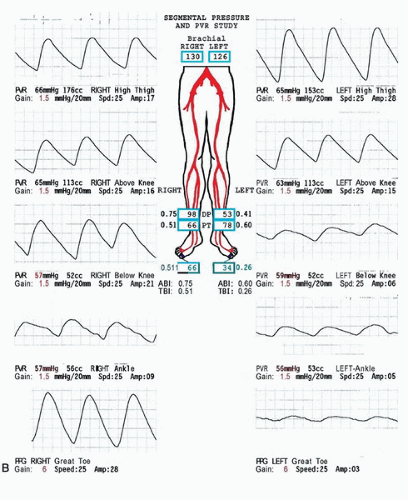
Air plethysmography can be used to generate pulse volume waveforms, a technique referred to as pulse volume recording (PVR).3 PVR waveforms are obtained with partially inflated air-filled cuffs that detect volume changes sequentially down a limb. The arterial pulse wave causes volume changes in the limb and produces small pressure changes within the cuffs; these changes are displayed as waveforms with the use of appropriate transducers. A normal pulse volume waveform has a sharp systolic upstroke, a narrow peak, and a downstroke that bows toward the baseline and contains a prominent dicrotic notch (Fig. 13.1A). As proximal arterial occlusive disease progresses, the systolic upstroke is delayed, the peak becomes rounded, and the dicrotic notch is lost as the downstroke bows away from the baseline (Fig. 13.1B). With more severe disease, the pulse volume waveform decreases in amplitude and the upstroke and down-stroke times become nearly equal (Fig. 13.1C and D). With very severe proximal disease, the pulse volume waveform is absent.4 Evaluation of pulse volume waveforms is qualitative and based on the shape of the curve, the presence or absence of the dicrotic notch, and the amplitude.5 Lack of more quantitative data limits the utility of PVR. An example of normal and abnormal lower extremity segmental PVR examinations is shown in Figure 13.2.
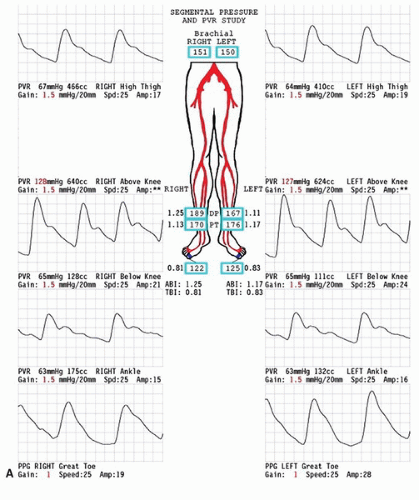 FIGURE 13.2. A, Normal lower extremity segmental PVR examination. The pulse volume waveforms at all levels display the normal features shown in Figure 13.1 and described in the text. In addition to the four standard levels (high thigh, above knee, below knee, and ankle), PPG waveforms from the great toes are also shown. The ankle-brachial index (ABI) and toe-brachial index (TBI) are normal bilaterally. |
Digit Waveforms and Pressure Measurements
One of the best current applications for plethysmography is in the evaluation of digit blood flow. Air plethysmography, strain-gauge plethysmography, and PPG can all be adapted for this purpose; however, PPG is probably the most widely used technique (Fig. 13.3). It should be noted that the PPG does not record a true volume change and therefore it is not, strictly speaking, a plethysmograph. It consists of an infrared light-emitting diode and a photosensor that detects the light reflected from the tissue. Because red light is attenuated in proportion to the blood content of tissue, the pulse waveform produced by the photosensor has the same features as the true plethysmographic methods. This technique is easily used in combination with pneumatic cuffs to measure digit systolic pressures, as discussed in Chapter 14 for the upper extremity. Digit pressures, as well as comparisons between digit pressures and brachial pressures, are utilized in clinical practice. The toe-to-brachial artery systolic pressure ratio (toe-brachial index or TBI) in normal subjects is greater than 0.70. An absolute digit pressure of less than 50 mm Hg indicates critical ischemia.
PPG-derived digit pressures are particularly useful in patients with highly calcified, noncompressible tibial arteries at the ankle. Digital arteries are less subject to calcification, and in the setting of calcified ankle arteries, toe pressures are a better indicator of the degree of distal ischemia than measurement of ankle pressures. The presence of normal digit PPG waveforms in patients with calcified proximal arteries indicates minimal restriction to blood flow despite the calcific arterial disease. Conversely, an obstructive digit waveform in the presence of normal ankle arterial pulses is frequently an indicator of pedal artery occlusive disease, a situation encountered in many patients with diabetes and those with atheroembolism or connective tissue disorders.
DOPPLER ULTRASOUND
Ankle-Brachial Index
A simple continuous-wave Doppler flow detector can be used along with a set of pneumatic cuffs to measure systolic blood pressures in the lower limb. The site of pressure measurement is determined by cuff placement, and any arterial Doppler signal distal to the cuff can be used. The ratio of ankle systolic pressure to brachial systolic pressure is a very useful measure of overall lower extremity perfusion. This test is performed with the patient supine and after resting for a few minutes to make sure that limb blood flow is at baseline levels. A pneumatic cuff is placed just above the ankle, and the continuous-wave Doppler probe is positioned over the posterior tibial or dorsalis pedis artery distal to the cuff to monitor the flow signal. The cuff is then inflated to suprasystolic levels until the Doppler signal disappears and slowly deflated; the pressure in the cuff when the Doppler signal returns is recorded as the systolic pressure. This sequence is repeated with the other artery at that ankle, and the values compared with the highest brachial artery systolic pressure, also
obtained with the Doppler. For clinical purposes, the higher ipsilateral dorsalis pedis or posterior tibial artery pressure is divided by the higher brachial artery systolic pressure, yielding the ankle-brachial index (ABI) for that lower extremity. The use of a ratio makes the test relatively independent of day-to-day variations in systemic arterial blood pressure and facilitates serial follow-up and comparisons between patients. As discussed in Chapter 5, a normal ABI is in the range of 1.0 to 1.2, with progressively lower values corresponding to worsening arterial occlusive disease (Table 13.1).6 A decreased ABI also correlates with an increased risk of cardiovascular death, with the risk increasing as the ABI falls, as discussed in Chapter 26.
obtained with the Doppler. For clinical purposes, the higher ipsilateral dorsalis pedis or posterior tibial artery pressure is divided by the higher brachial artery systolic pressure, yielding the ankle-brachial index (ABI) for that lower extremity. The use of a ratio makes the test relatively independent of day-to-day variations in systemic arterial blood pressure and facilitates serial follow-up and comparisons between patients. As discussed in Chapter 5, a normal ABI is in the range of 1.0 to 1.2, with progressively lower values corresponding to worsening arterial occlusive disease (Table 13.1).6 A decreased ABI also correlates with an increased risk of cardiovascular death, with the risk increasing as the ABI falls, as discussed in Chapter 26.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree