Guidelines for the use of cardiac pacemakers and the internal cardioverter-defibrillator (ICD) were first established in 1984 by a task force formed jointly by the American College of Cardiology (ACC) and the American Heart Association (AHA). These were most recently updated in 2008 in conjunction with the North American Society of Pacing and Electrophysiology, now named the Heart Rhythm Society (HRS).1 In 2006, the ACC, AHA, and European Society of Cardiology (ESC) published guidelines for prevention of sudden cardiac death, which included updated guidelines for ICD implantation.2 Based on the strength of available data and expert opinion, the indications have been divided into the following three classes:
Indications for Permanent Pacing
As the guidelines classification implies, some conduction disturbances are accepted as definite indications for permanent pacing, but for others there is general agreement that permanent pacing is not required. However, expert clinicians disagree about criteria for pacemaker use and whether to use single- or dual-chamber devices for many clinical scenarios, and in a number of conduction disturbances the need for permanent pacing depends on the unique circumstances of the patient. Because of changes in diagnosis and therapy, the absolute indications for permanent pacing are constantly evolving.
Before concluding that permanent pacing is indicated, the physician must carefully assess whether it is in the best interest of the patient. This assessment should include the specifics of the cardiac rhythm disturbance, the patient’s general medical status, and the patient’s concerns and preferences. As a rule of thumb, bradycardias caused by nontemporary conditions that are associated with symptoms warrant pacing. These are discussed in more detail below.
Indications for permanent pacing are categorized by the underlying conduction system disorder or disease process, including:
- Atrioventricular (AV) block
- Acute myocardial infarction
- Chronic bifascicular and trifascicular block
- Sinus node dysfunction
- Neurally mediated syncope
- Tachyarrhythmias
- Hypertrophic cardiomyopathy
- Congestive heart failure
- Cardiac transplantation
The ACC/AHA/HRS guidelines also include a section on pacing indications for pediatric patients. In this chapter, specific pediatric considerations are included within the broader categories; e.g., congenital AV block is included in the section on AV block.
Atrioventricular Block
AV block is the impairment of conduction of a cardiac impulse from the atrium to the ventricles. It can occur at different levels: proximal to the AV node, in the AV node, or in the His–Purkinje system. Indications for permanent pacing in patients with AV block are summarized in Table 3.1.
Table 3.1 Indications for pacing in atrioventricular (AV) block.
| Class I | |
| 1 | Third-degree or advanced second-degree AV block at any anatomic level associated with any one of the following conditions: |
| a | Symptoms (including heart failure) attributable to AV block |
| b | Arrhythmias and other medical conditions that require drugs that result in symptomatic bradycardia |
| c | Documented periods of asystole >3.0 s, any escape rate ≤40 bpm, or any esacpe rhythm below the AV junction (e.g., a wide QRS morphology) in awake, asymptomatic patients in sinus rhythm |
| d | A documented period of asystole >5 s in awake, asymptomatic patients in atrial fibrillation |
| e | After catheter ablation of the AV junction |
| f | Postoperative AV block that is not expected to resolve after cardiac surgery |
| g | Neuromuscular diseases, such as myotonic muscular dystrophy, Kearns–Sayre syndrome, Erb’s (limb-girdle) dystrophy, and peroneal muscular atrophy, with or without symptoms of bradycardia |
| 2 | Asymptomatic third-degree AV block at any anatomic site with an average awake ventricular rate >40 bpm in patients with cardiomegaly or left ventricular dysfunction |
| 3 | Second-degree or third-degree AV block during exercise in the absence of myocardial ischemia |
| 4 | Symptomatic second-degree AV block regardless of type or site of block |
| 5 | Congenital third-degree AV block with a wide QRS escape rhythm, complex ventricular ectopy, or ventricular dysfunction |
| 6 | Congenital third-degree AV block in an infant with a ventricular rate <50–55 bpm or with congenital heart disease and a ventricular rate <70 bpm |
| Class IIa | |
| 1 | Advanced second-degree or third-degree AV block at any anatomic site with an average ventricular rate >40 bpm in the absence of cardiomegaly or hypertrophy |
| 2 | Asymptomatic type I second-degree AV block at intra- or infra-His levels found at electrophysiologic study |
| 3 | First-degree or second-degree AV block with symptoms similar to those of pacemaker syndrome |
| 4 | Congenital third-degree AV block after the first year of life with an average ventricular rate <50 bpm or abrupt pauses in ventricular rate that are two to three times the basic cycle length |
| 5 | Long QT syndrome with third-degree or advanced second-degree AV block |
| 6 | Congenital heart disease and loss of AV synchrony with impaired hemodynamics |
| Class IIb | |
| 1 | Severe first-degree AV block (>0.30 s) in patients with ventricular dysfunction and symptoms of heart failure in whom a shorter AV interval results in hemodynamic improvement |
| 2 | AV block due to drug use or toxicity when the block is expected to recur even after withdrawal of the drug |
| 3 | Neuromuscular diseases, such as myotonic muscular dystrophy, Kearns–Sayre syndrome, Erb’s (limb-girdle) dystrophy, and peroneal muscular atrophy with any degree of AV block (including first-degree AV block), with or without symptoms of bradycardia |
| 4 | Pediatric patient with transient postoperative third-degree AV block that reverts to sinus rhythm with residual bifascicular block |
| 5 | Infant, child, adolescent, or young adult with asymptomatic congenital third-degree AV block, an acceptable rate, narrow QRS complex, and normal ventricular function |
| Class III | |
| 1 | Asymptomatic first-degree AV block |
| 2 | Asymptomatic type I second-degree AV block at a site above the His (i.e., the AV node) or not known to be intra- or infra-Hisian by electrophysiology study |
| 3 | AV block expected to resolve and unlikely to recur (e.g., drug toxicity, Lyme disease, nocturnally in sleep apnea, early postoperative status, transient increases in vagal time) |
Electrocardiographically, AV block is divided into first-degree, second-degree, and third-degree (complete) heart block. First-degree heart block is reflected by a prolonged PR interval with conduction to the ventricle. The normal PR interval is defined electrocardiographically as a range of 120–200 ms. First-degree AV block is usually secondary to a delay of impulse conduction through the atrium or AV node (Fig. 3.1).
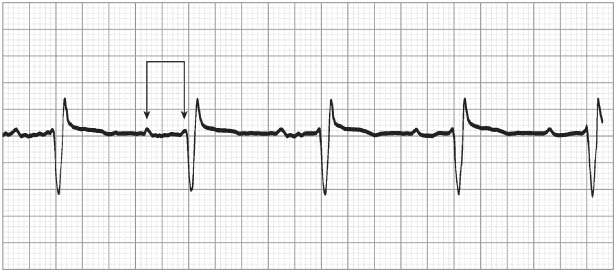
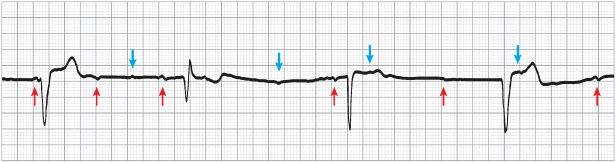
Second-degree AV block occurs when an atrial impulse that should be conducted to the ventricle is not conducted. The blocked impulses may be intermittent or frequent, at regular or irregular intervals, and preceded by fixed or lengthening PR intervals. A distinguishing feature of second-degree heart block is that impulse conduction occurs in a recurrent pattern rather than randomly (i.e., there is a recognizable pattern in the relationship between P waves and QRS complexes). Second-degree AV block is further classified as Mobitz type I (also called Wenckebach block), Mobitz type II block, or advanced second-degree AV block. Typical type I second-degree AV block is characterized by progressive PR interval prolongation that culminates with a nonconducted P wave (Fig. 3.2). In type II second-degree AV block, the PR interval remains constant before the nonconducted P wave (Fig. 3.3), and a P wave abruptly fails to conduct to the ventricles. The AV block is intermittent and generally repetitive. Advanced second-degree AV block is characterized by more than one nonconducted P wave in a row, with the presence of some conducted beats. Type II second-degree AV block often precedes the development of higher grades of AV block, whereas type I second-degree AV block is usually a less severe conduction disturbance that does not consistently progress to more advanced AV block.
Fig. 3.3 Advanced atrioventricular block, in which there is sporadic failure to conduct from the atrium to the ventricle. Here, the first and last P waves result in ventricular depolarization, with a PR interval of 220 ms. However, nine P waves are not conducted through the AV node, and the result is a 7.4-s period of ventricular asystole.
Anatomically, type I second-degree AV block with a normal QRS complex usually occurs at the level of the AV node, proximal to the bundle of His. AV block that is 2 : 1 may be type I or II second-degree AV block. If the QRS complex is narrow, the block is more likely to be type I and one should search for transition of the 2 : 1 block to 3 : 2 block, during which the PR interval lengthens in the second cardiac cycle (Fig. 3.4). If the QRS complex is wide, the level of block is more likely to be distal to the His bundle and the escape focus is usually less reliable (Figs 3.5 and 3.6). If pre-existing bundle branch block is present, it is difficult to distinguish whether the block is located in the AV node or the His–Purkinje system. An attempt to alter the AV conduction ratio, either by exercise or by pharmacologic means (e.g., with atropine) may allow localization of the conduction abnormality and assist with diagnosis. AV block that develops or worsens during exercise reflects conduction disease in the His–Purkinje system, which warrants implantation of a permanent pacemaker. During exercise, increased adrenergic drive facilitates AV nodal conduction; a diseased distal conduction system is unable to accommodate the increased rate and block occurs. In contrast, block in the AV node is more often physiologic, due to increased vagal tone. Exercise changes the autonomic balance, leading to diminished vagal tone and improved conduction. Pacing is generally not needed in this situation.
Fig. 3.4 Second-degree 2 : 1 atrioventricular block with a narrow QRS complex. With a 2 : 1 conduction ratio, it is impossible to tell from the electrocardiogram exactly where in the atrioventricular junction the conduction disturbance occurs. A narrow QRS complex suggests that the conduction defect is “supra-His” (at the level of the atrioventricular node or His bundle) rather than “infra-His,” which would result more commonly in a wide QRS complex.
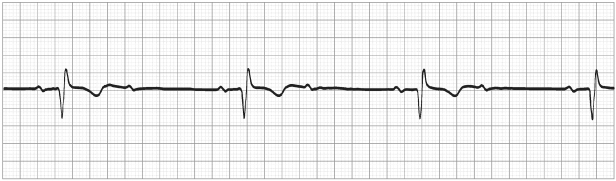
Fig. 3.5 Second-degree 2 : 1 atrioventricular block with left intraventricular conduction delay. This pattern suggests an infra-His conduction defect.
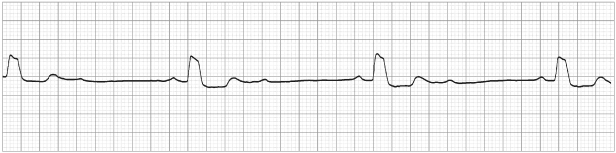
Fig. 3.6 Subsequent electrocardiogram from the patient whose recording is shown in Fig. 3.5. Here, there is intermittent third-degree atrioventricular block with junctional escape beats (arrows indicate P waves).
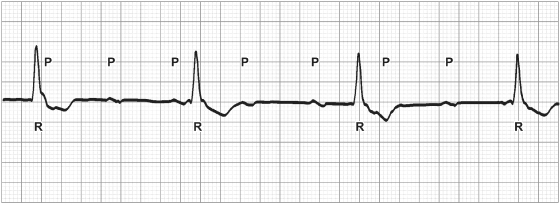
Third-degree AV block (complete heart block) is defined by lack of conduction of atrial impulses to the ventricle (Fig. 3.7). It is important to distinguish this from AV dissociation due to a subsidiary pacemaker, usually junctional, that discharges more rapidly than the underlying sinus rate. In contrast, in third-degree AV block, the atrial rate is faster than the ventricular escape and there is no AV nodal conduction.
Fig. 3.7 Third-degree atrioventricular block (complete heart block) is characterized by complete lack of conduction from atrium to ventricle and dissociation of atrial and ventricular activity. Here, the atrial activity (identified by P’s on the tracing) occur at approximately 100 bpm, whereas the ventricular complexes (R’s) occur at just under 40 bpm.
Third-degree AV block may be congenital or acquired. In the congenital form, there is anatomic discontinuity in the conduction pathway. Pacing for this disorder was controversial for many years, because many patients with congenital complete heart block consider themselves asymptomatic, and there was conflicting information on the risk of sudden death associated with the condition. However, subjective improvement is usually noted once chronotropic competency is restored with permanent pacing. In addition, data support improved survival with permanent pacing.3,4 Indications for pacing in patients with congenital complete heart block are the presence of a wide QRS escape rhythm, complex ventricular ectopy, or ventricular dysfunction; or, in an infant, a ventricular rate of <50–55 bpm, or a ventricular rate <70 bpm if congenital heart disease is also present. In addition, a class IIa indication is congenital complete heart block after the first year of life with an average ventricular rate <50 bpm or abrupt pauses in ventricular rate that are two or three times the basic cycle length. Finally, congenital complete heart block in an asymptomatic infant, child, adolescent, or young adult with an acceptable rate, narrow QRS, and normal ventricular function is considered a class IIb indication.1 In summary, pacing can be justified in any patient with congenital complete heart block, although the strength of evidence varies depending on the clinical circumstance.
Acquired third-degree AV block is due most commonly to aging, with or without calcification of the conduction system, or ischemic disease (e.g., myocardial infarction with damage involving the conduction system). Complete heart block has been associated with a number of systemic illnesses, many of which have been described in case reports (Table 3.2). Iatrogenic complete heart block can occur with open heart surgery or with inadvertent AV node ablation during treatment of supraventricular tachyarrhythmias. Acquired complete heart block can be either intermittent or fixed. Patients may be asymptomatic or experience severe symptoms related to profound bradycardia, AV dissociation, or ventricular arrhythmias. It has been well documented that patients with complete heart block have improved survival with permanent pacing.5
Table 3.2 Causes of acquired atrioventricular (AV) block.
| Idiopathic (senescent) AV block |
| Coronary artery disease |
| Calcific valvular disease |
| Postoperative or traumatic |
| AV node ablation |
| Therapeutic radiation to the chest |
| Infections: |
|
| Collagen-vascular diseases: |
|
| Infiltrative diseases: |
|
| Neuromuscular diseases: |
|
| Drug effects: |
|
The most important factor in the decision to implant a pacemaker in a patient with AV block is whether or not the patient has symptoms that may be directly attributed to the arrhythmia. These symptoms include overt or near syncope, lightheadedness, fatigue, activity intolerance, dyspnea, confusion or other cognitive changes, or symptoms of heart failure. Another important factor in the decision to implant a pacemaker for AV block is the expected irreversibility of the conduction disturbance. Potentially reversible causes of AV block include electrolyte abnormalities, Lyme disease, perioperative hypothermia or inflammation, sleep apnea, and vagally mediated bradyarrhythmias related to medical illness or physiologic changes in autonomic tone (e.g., bradycardia during emesis).
Atrial fibrillation with a slow ventricular response reflects the presence of AV block, although it is often categorized as sinus node dysfunction. Patients with this condition should receive a pacemaker if the bradycardia is causing symptoms (Fig. 3.8).
Areas of controversy exist in the indications for permanent pacing for AV block, and there are situations in which deviations from the ACC/AHA/HRS guidelines may be appropriate. Although the guidelines designate asymptomatic complete heart block with ventricular escape rates >40 bpm as a class IIa indication for pacing, we believe it should be a class I indication. The rate cut-off of 40 bpm is arbitrary, and it is not the escape rate per se that is critical to stability, but rather the site of origin of the escape rhythm (i.e., the AV node, His bundle, His–Purkinje system, or the ventricle). No definitive evidence exists regarding the conduction system localization or long-term stability of an escape rate of 40 bpm. Unfortunately, rate stability is not obvious or predictable. Clinically, one must grapple with whether the patient is truly asymptomatic and whether any diagnostic procedures, such as ambulatory monitoring or exercise testing, should be performed. No clinical trials or observational studies provide answers to these questions. From a practical and safety standpoint, we believe that permanent pacing is warranted for irreversible, acquired, complete heart block.
Some asymptomatic patients with type I second-degree AV block have as poor a prognosis as patients with type II second-degree AV block, and permanent pacing improves survival in those patients >45 years old.6,7 Asymptomatic type I second-degree AV block not known to be at intra- or infra-Hisian levels is a class III indication (a contraindication) for pacing. Generally, an electrophysiology study to obtain His bundle recordings is not recommended. However, if an electrophysiology study is performed for other reasons and asymptomatic type I second-degree AV block with a narrow QRS is found to be infranodal, then pacemaker implantation is a class IIa indication according to the current guidelines. In this setting, a patient is likely to have diffuse conduction system disease, and we believe permanent pacing is warranted.
In patients with specific neuromuscular diseases, pacing is advocated as a class I indication in third-degree AV block and as a class IIb indication in first-degree or second-degree AV block. The potential for sudden death in this group of patients is well documented.8–11 Because of the unpredictable progression to symptomatic bradycardia in patients with first-degree or second-degree AV block, the safest and most rational approach may be to offer pacing once any conduction abnormality is noted and subsequent follow-up reveals any progression. As discussed later, ICD therapy may also need to be considered for these patients.12
Acute Myocardial Infarction
Conduction disturbances associated with acute myocardial infarction are largely related to the site of the infarction and the extent of myocardial injury.13,14 Given a greater awareness of the symptoms of acute myocardial infarction, the seeking of healthcare earlier, and more aggressive acute intervention, there are fewer extensive infarcts and permanent pacing is becoming less frequently required in this situation. Inferior myocardial infarctions are accompanied by a variety of conduction disturbances, including sinus bradycardia, sinus arrest, atrial fibrillation, atrial flutter, and all grades of AV block.15 Anterior myocardial infarctions are more likely to be accompanied by AV block or intraventricular conduction defects (or both).16
The indications for permanent pacemaker implantation after an acute myocardial infarction are based on the persistence of AV block and the presence of concomitant intraventricular conduction disturbances (Table 3.3). A general rule is that a permanent pacemaker is not indicated in a patient with an acute myocardial infarction if AV block is expected to resolve and if the conduction disturbance is not associated with a poor long-term prognosis.15,16 The indications are less dependent on the presence or absence of symptoms, unlike pacing indications in other clinical settings. Clear class I indications are persistent, severe conduction disturbances (second-degree AV block in the His–Purkinje system with bilateral bundle branch block, or third-degree AV block at or below the His–Purkinje system). Also considered a class I indication is transient advanced (second-degree or third-degree) infranodal AV block and associated bundle branch block. A reasonable rule of thumb is useful in the patient with transient second-degree or third-degree AV block and associated bundle branch block: after an anterior wall myocardial infarction, a pacemaker is indicated if vagal block is excluded, because the block is almost certainly infranodal; after an inferior wall myocardial infarction no pacemaker is needed, because the prognosis is good and is not adversely affected by the AV block. Also, it is important to note that a requirement for temporary pacing in a patient with acute myocardial infarction does not constitute an indication for permanent pacing for that patient.
Table 3.3 Indications for permanent pacing after acute myocardial infarction (MI).
| Class I | |
| 1 | Third-degree atrioventricular (AV) block within or below the His–Purkinje system after ST-segment elevation MI or persistent second-degree AV block in the His–Purkinje system with alternating bundle branch block |
| 2 | Transient second- or third-degree infranodal AV block and associated bundle branch block. If the site of block is uncertain, an electrophysiologic study may be necessary |
| 3 | Persistent and symptomatic second- or third-degree AV block |
| Class IIa | |
| None | |
| Class IIb | |
| Persistent second- or third-degree transient AV block at the AV node level, with or without symptoms | |
| Class III | |
| 1 | Transient AV block without intraventricular conduction defects |
| 2 | Transient AV block with isolated left anterior fascicular block |
| 3 | Acquired left anterior fascicular block without AV block |
| 4 | Asymptomatic first-degree AV block with bundle branch or fasicular block |
Chronic Bifascicular and Trifascicular Block
Bifascicular block is defined as a conduction disturbance of two fascicles of the ventricular conduction system (e.g., isolated left bundle branch block, right bundle branch block [RBBB] and left anterior fascicular block, or RBBB and left posterior fascicular block). Trifascicular block is defined as a conduction disturbance in all three fascicles (either simultaneously or in successive ECGs) or the presence of first-degree AV block and bifascicular block. A special example of trifascicular block is alternating bundle branch block (also referred to as bilateral bundle branch block).
Indications for permanent pacing in patients with bifascicular or trifascicular block depend on the risk of development of transient or permanent advanced AV block (Table 3.4).17 This is because patients with bifascicular or trifascicular block and advanced AV block have higher rates of sudden death and all-cause death. Syncope is common in patients with bifascicular block, but it is not associated with an increased risk of sudden death. Thus, defining the cause of syncope in patients with bifascicular and trifascicular block is important, and a permanent pacemaker should be implanted if transient or persistent, advanced AV block is documented. If, after investigation, the cause of syncope is undetermined, then implantation of a permanent pacemaker is reasonable (class IIa indication), because the syncope may be due to intermittent advanced AV block. However, it is notable that the incidence of progression of bifascicular block to complete heart block is low, and that there are no reliable predictors of death from progression of the conduction disease. Patients with RBBB and left anterior hemiblock are at higher risk of cardiovascular death, but this is not specifically due to bradycardia or conduction disease, and permanent pacing is not recommended in these patients in the absence of symptoms or advanced AV block.
Table 3.4 Indications for pacing in chronic bifascicular and trifascicular block.
| Class I | |
| 1 | Intermittent third-degree or advanced second-degree atrioventricular (AV) block |
| 2 | Type II second-degree AV block |
| 3 | Alternating bundle branch block. |
| Class IIa | |
| 1 | Syncope not demonstrated to be due to AV block when other likely causes, specifically ventricular tachycardia, have been excluded |
| 2 | Incidental finding at electrophysiologic study of markedly prolonged HV interval (≥100 ms) in asymptomatic patients |
| 3 | Incidental finding at electrophysiologic study of pacing-induced infra-His block that is not physiologic |
| Class IIb | |
| Neuromuscular diseases, such as myotonic muscular dystrophy, Kearns–Sayre syndrome, Erb’s (limb-girdle) dystrophy, and peroneal muscular atrophy with any degree of fascicular block, with or without symptoms of bradycardia | |
| Class III | |
| 1 | Fascicular block without AV block or symptoms |
| 2 | Fascicular block with first-degree AV block without symptoms |
Although the incidence of progression to advanced AV block is relatively low in patients with bifascicular or trifascicular block, measurement of the HV interval (a measure of conduction of the His–Purkinje system) may rarely help in identifying patients at higher risk of developing symptomatic advanced AV block. The degree of HV interval lengthening necessary to justify prophylactic pacemaker placement is controversial. Some have advocated pacing for an HV interval of >100 ms, and others have considered pacing for an HV interval of >70 ms, especially if the patient is to receive cardioactive drugs that have the potential for further impairment of the conduction system. The development of nonphysiologic infra-His block with increasingly rapid atrial pacing during an electrophysiology study may reflect increased risk of progression to advanced AV block or symptomatic bradycardias (and thus has a class IIa indication for permanent pacing); however, failure to develop infra-His block is not a reliable indicator that advanced AV block will not develop in the future. Electrophysiologic studies to measure HV intervals are not routinely performed in patients with bifascular or trifascular block in the absence of symptoms or other findings.
Sinus Node Dysfunction
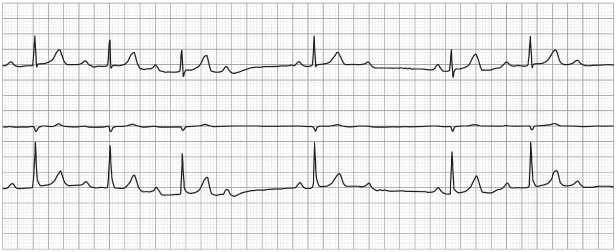
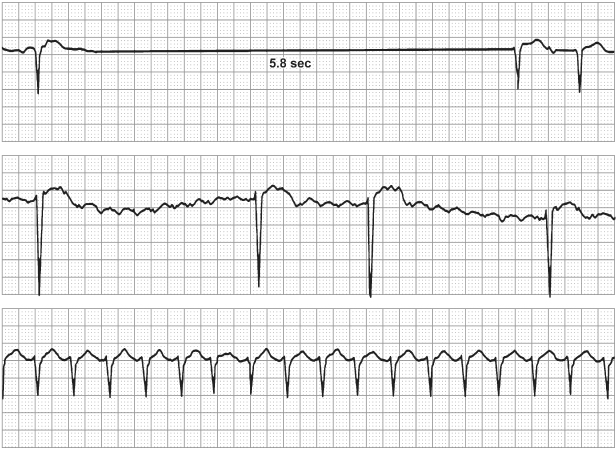
Sinus node dysfunction (sick sinus syndrome) includes a variety of cardiac arrhythmias, including sinus bradycardia (Fig. 3.9), sinus arrest (Fig. 3.10), and sinoatrial block. It also includes the tachycardia-bradycardia syndrome, in which paroxysmal supraventricular tachycardias alternate with periods of bradycardia or asystole (Fig. 3.11). Indications for permanent pacing in patients with sinus node dysfunction are summarized in Table 3.5.
Table 3.5 Indications for pacing in sinus node dysfunction.
| Class I | |
| 1 | Sinus node dysfunction with symptomatic bradycardia or frequent symptomatic sinus pauses. In some patients, bradycardia is iatrogenic and occurs as a consequence of essential long-term drug therapy for which there is no acceptable alternative. The definition of bradycardia varies with the patient’s age and expected heart rate |
| 2 | Symptomatic chronotropic incompetence |
| Class IIa | |
| 1 | Sinus node dysfunction occurring spontaneously or as a result of necessary drug therapy, with heart rate <40 bpm, when a clear association between significant symptoms consistent with bradycardia and the actual presence of bradycardia has not been documented |
| 2 | Syncope of unknown etiology when sinus node dysfunction is provoked or discovered during electrophysiologic testing that is felt to be clinically significant |
| Class IIb | |
| In minimally symptomatic patients, chronic heart rate <40 bpm while awake | |
| Class III | |
| 1 | Sinus node dysfunction in asymptomatic patients |
| 2 | Sinus node dysfunction in patients with symptoms that are clearly documented in the absence of bradycardia |
| 3 | Sinus node dysfunction with symptomatic bradycardia due to nonessential drug therapy |
Fig. 3.9 Sinus bradycardia with a rate of 39 bpm. The patient had symptoms that resolved after DDD pacing.
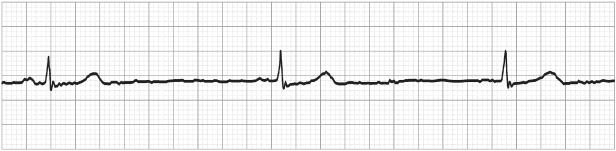
Fig. 3.10 Continuous electrocardiographic tracing from a patient with tachycardia-bradycardia syndrome (sinus node dysfunction). Here, sinus rhythm alternates with atrial flutter, and an episode of sinus arrest with a 4.5-s pause occurs.
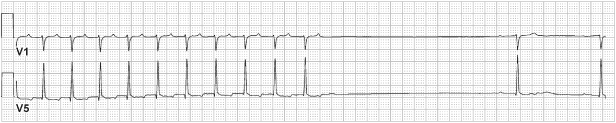
Fig. 3.11 Three electrocardiographic tracings obtained from the same patient over a 12-h period. The top tracing shows sinus arrest with a 5.8-s pause terminated by a junctional escape beat. The middle tracing shows atrial flutter with a slow ventricular response. The bottom tracing shows supraventricular tachycardia.
The definition of clinically significant bradycardia varies, but it is generally agreed to denote rates of <40 bpm during waking hours. Sinus pauses of ≥3 s or symptomatic sinus rates <40 bpm in the awake patient are indications for permanent pacing. However, it should be recognized that there is disagreement about the absolute cycle length of an asystolic period that requires pacing. The patient’s entire clinical condition should be considered, including age, associated diseases, medications, and symptoms. For example, sleeping endurance athletes have sinus rates as low as 30 bpm, but are asymptomatic and do not require pacing. Sinus bradycardia during sleep in an asymptomatic patient is not an indication for pacing. Sleep apnea is a potential cause of nocturnal bradycardias that should be treated if considered clinically significant.18,19 This is particularly true if atrial fibrillation is also present, because approximately half of patients with atrial fibrillation also have obstructive sleep apnea.20
In sinus node dysfunction, correlation of symptoms with the specific arrhythmia is essential. The use of ambulatory ECG monitors and event loop recorders is helpful to document patients’ rhythms during specific symptoms. Patients who develop symptomatic bradycardias due to required pharmacologic therapy for other conditions require permanent pacing, but pacing is unnecessary if the bradycardias are asymptomatic. Chronotropic incompetence may be demonstrated by the absence of an appropriate physiologic increase in sinus rate with exercise, and it is a class I indication for implantation of a rate-responsive permanent pacemaker.
When permanent pacing is indicated for patients with sinus node dysfunction, special thought should be given to selection of the appropriate device and programming. Single-chamber ventricular pacemakers are not appropriate for patients with sinus node dysfunction. Single-chamber atrial pacemakers with rate-responsive capability are attractive because of their relative simplicity and lower cost compared with dual-chamber pacemakers. In patients without coexisting AV block, AAIR pacing may be appropriate. The major concern is that AV block develops in patients with sinus node dysfunction after atrial pacemaker implantation at an annual rate of 0.6–5%, with a higher risk in patients with pre-existing bundle branch block.21,22 Although this risk is relatively low, there is some benefit to provide ventricular pacing in the event it is needed. Conversely, pacing the ventricle unnecessarily can result in a higher incidence of atrial fibrillation and congestive heart failure.23–26 Avoidance of ventricular pacing can be accomplished by programming a very long AV interval, or by use of an algorithm that effectively avoids ventricular pacing except when absolutely required by predefined criteria (discussed further in Chapter 8: Programming). Thus, the best options for sinus node dysfunction are either a single-chamber atrial pacemaker or a dual-chamber pacemaker that is programmed either manually or via an algorithm to avoid ventricular pacing. The decision must be made on an individual basis, with consideration of the extent of conduction disease, severity of its clinical manifestations, comorbidities, risk of future revision to a dual-chamber system, and the patient’s own preferences. In the USA, dual-chamber pacemakers are most commonly used.
Neurally Mediated Reflex Syncope
Permanent pacing is indicated in the proper clinical setting for some types of neurally mediated reflex syncope, which includes carotid sinus syndrome and neurocardiogenic (vasovagal) syncope (Table 3.6). Understanding the physiology involved in these different types of syncope is crucial to understanding their clinical manifestations and the appropriateness of permanent pacing.27
Table 3.6 Indications for pacing in neurally mediated reflex syncope.
| Class I | |
| Recurrent syncope caused by carotid sinus hypersensitivity, defined as minimal carotid sinus pressure inducing ventricular asystole of ≥3 s in patients not receiving medication that depress the sinus node or AV conduction | |
| Class IIa | |
| Syncope in the absence of definite provocative event with a pause of ≥3 s with carotid massage | |
| Class IIb | |
| Recurrent symptomatic neurocardiogenic syncope with a cardioinhibitory response during tilt-table testing | |
| Class III | |
| 1 | A cardioinhibitory response during carotid sinus stimulation without symptoms or vague symptoms |
| 2 | Situational vasovagal syncope in which avoidance behavior is effective |
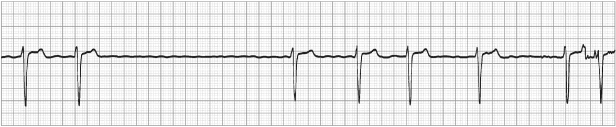
The carotid sinus reflex is the physiologic bradycardic response to stimulation of the carotid sinus baroreceptors. Although this reflex is normal, some individuals have an exaggerated response that may be pathologic. This reflex has two components. The first, a cardio-inhibitory response, results from increased parasympathetic tone and may be manifested by any or all of the following: sinus bradycardia, sinus arrest (Fig. 3.12), PR prolongation, and advanced AV block. The second component, a vasodepressor response, is due to decreased sympathetic activity and results in peripheral vasodilatation and hypotension (independently of changes in heart rate). Pure cardio-inhibitory or pure vasodepressor responses may occur, but a mixed response is most common.
Fig. 3.12 Carotid sinus massage may demonstrate carotid sinus hypersensitivity, which may be a cause of syncope. Here, carotid sinus massage produced prolonged sinus arrest with a junctional escape.
The definitions of normal and abnormal responses to carotid sinus stimulation are somewhat arbitrary. Generally, an abnormal response is defined as development of ventricular asystole of ≥3 s and/or a decrease in blood pressure of 30–50 mmHg. As many as 40% of patients ≥65 years old have carotid sinus hypersensitivity;28 thus, the causal relationship between carotid sinus hypersensitivity and symptoms is critical to decisions regarding therapy. Patients with syncope may have a typical history related to a tight collar or neck extension, but more commonly definite provocative maneuvers cannot be identified. If carotid sinus massage reproduces the patient’s symptoms and is associated with significant cardio-inhibition or vasodepression, a diagnosis of carotid sinus syndrome can be made and treatment should be initiated. If carotid sinus massage yields a positive result but does not reproduce the patient’s symptoms, a hypersensitive carotid reflex has been demonstrated, but it may not be of clinical significance, and other causes for syncope should be investigated. Situations exist where it is difficult to correlate symptoms. If the result of carotid sinus massage is negative, tilt testing may be indicated to identify other mechanisms of neurally mediated reflex syncope.
Neurocardiogenic (vasovagal) syncope may be benign or malignant. The exact pathophysiology of these syndromes is unclear, but important mechanisms include prolonged orthostatic stress, venous pooling, activation of cardiac mechanoreceptors, and an abnormal decrease in sympathetic activity. These processes result in bradycardia, peripheral vasodilatation, and syncope.27 The episodes can be triggered by various stimuli, such as pain, warm environments, visceral sensations, and acute psychologic stress. Manifestations include a prodrome of nausea, diaphoresis, and light-headedness followed by a brief episode of unconsciousness, after which there is quick and complete cognitive recovery. In the elderly, prodromal symptoms are often absent and loss of consciousness may occur suddenly, mimicking other causes of syncope.29
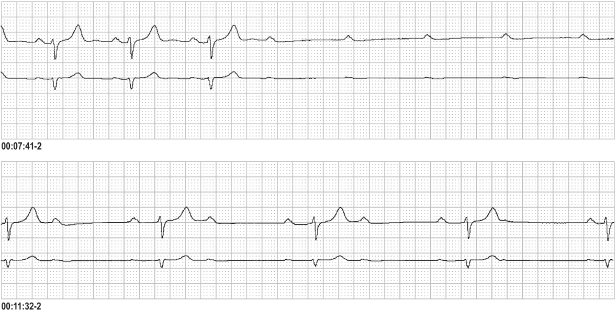
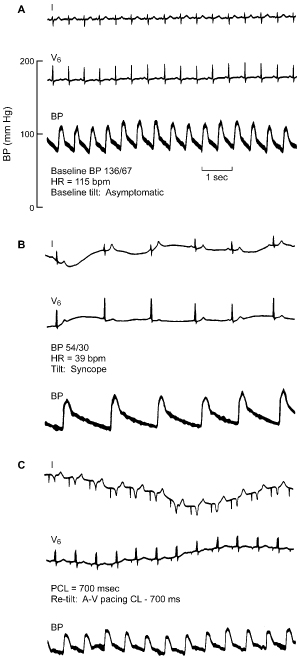
Head-up tilt-table testing can reproduce neurocardiogenic syncope in susceptible patients. Passive head-up tilt creates an exaggerated orthostatic state by stressing the autonomic system in the absence of the usual compensatory skeletal muscle tone. This triggers the cascade of mechanisms described above. Tilt-table testing can help identify whether the predominant cause of symptoms is vasodepressor or cardio-inhibitory in origin (Fig. 3.13), which is important because therapy may differ for each situation.
Fig. 3.13 Electrocardiographic and arterial blood pressure recordings obtained during head-up tilt-table testing. (A) Recordings made during tilt with the patient asymptomatic demonstrate normal sinus rhythm at a heart rate (HR) of 115 bpm and baseline blood pressure (BP) of 136/67 mmHg. (B) Recordings during syncope, at which time the HR was 39 bpm and the BP was 54/30 mmHg. (C) After atrioventricular sequential pacing at a cycle length of 700 ms (86 ppm), a subsequent tilt-table test produced significant vasodepression, but the patient experienced only presyncope.
(Courtesy of Dr. W.K. Shen, Mayo Clinic, Rochester, MN.)
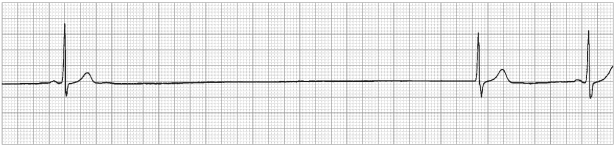
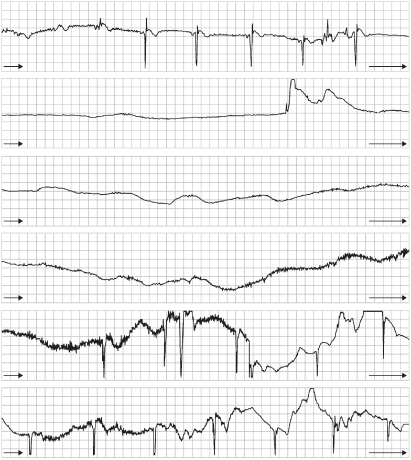
Benign vasovagal syncope, or a “simple faint,” usually does not require therapy. Associated rhythms are usually prolonged sinus arrest without a junctional or ventricular escape rhythm (Fig. 3.14). Situational syncope, which occurs stereotypically with swallowing, cough, micturition, or defecation, does not significantly increase mortality and usually does not require permanent pacing. However, recurrent events may be disabling to some patients, and the situations during which the events occur, such as operation of a motor vehicle or heavy machinery, may predispose the patient or bystanders to danger. In these cases, permanent pacemaker implantation may be an effective means of preventing syncope; however, this is unproven and controversial.
Fig. 3.14 Continuous electrocardiographic recording in a 55-year-old man who has hypervagotonia, with an asystolic period >30 s. Recovery with sinus bradycardia occurs in the fifth panel.
In patients with significant cardio-inhibition, permanent pacing is a seemingly intuitive intervention. Despite early promise,30–32 randomized trials have shown that permanent pacing does not improve outcomes in patients with neurocardiogenic syncope.33,34 The data suggested a benefit with permanent pacing only in patients with severe cardio-inhibition (i.e., asystole) compared with those with less severe bradycardias during tilt-table testing. The indications for permanent pacing in patients with neurocardiogenic syncope include: (i) a significant cardio-inhibitory component with severe bradycardia or asystole during syncope; (ii) lack of a prodrome; and (iii) recurrent syncope despite maximally tolerated medical therapy.35 Pacemakers with the capability of triggering a faster pacing rate for a defined period of time in response to a specified sudden drop in heart rate have been developed specifically for this syndrome. For all patients with neurocardiogenic syncope, principal therapy includes diet and lifestyle modification, compression stockings, and pharmacologic agents. Most patients have a mixed cardio-inhibitory and vasodepressor response, and it is most common for hypotension to precede bradycardia during an episode, so the medical therapies must continue even after pacemaker implantation, when pacing is offered.
Tachyarrhythmias
Previously, national guidelines recognized a number of class I indications for implantation of permanent pacemakers that detect and pace to terminate tachyarrhythmias. These devices initiate programmed stimulation or bursts of rapid pacing to terminate re-entrant arrhythmias after their automatic detection or after user activation (by magnet application). However, because of the wide availability and success of treatment by catheter ablation, there are currently no class I indications for permanent pacemakers to treat supraventricular tachyarrhythmias (Tables 3.7 and 3.8). Indications for device implantation in the treatment of ventricular tachyarrhythmias is discussed in a subsequent section (see Indications for the implantable cardioverter-defibrillator).
Table 3.7 Indications for pacemakers to terminate tachycardia.
| Class I | |
| None | |
| Class IIa | |
| Symptomatic recurrent supraventricular tachycardia that is reproducibly terminated by pacing in the unlikely event that catheter ablation and/or drugs fail to control the arrhythmia or produce intolerable side effects | |
| Class III | |
| The presence of accessory pathways with the capacity for rapid anterograde conduction | |
Table 3.8 Indications for pacemakers to prevent tachycardia.
| Class I | |
| Pause-dependent sustained ventricular tachycardia with or without prolonged QT | |
| Class IIa | |
| Pacing is reasonable for patients with congenital long-QT syndrome considered to be high-risk | |
| Class IIb | |
| Prevention of symptomatic, drug-refractory recurrent atrial fibrillation in patients with coexisting sinus node dysfunction | |
| Class III | |
| 1 | Frequent or complex ventricular ectopic activity without sustained ventricular tachycardia in patients without long QT syndrome |
| 2 | Torsades de pointes ventricular tachycardia due to reversible causes |
The implantation of a permanent pacemaker to prevent or treat tachyarrhythmias is still indicated in rare situations. A class I indication is for patients with or without a long QT interval who experience recurrent pause-dependent ventricular tachycardia (VT). The device of choice in these individuals is an implanted cardioverter-defibrillator with a bradycardia pacing function. The use of pacemakers to terminate supraventricular tachycardias or to prevent AV node re-entrant or AV re-entrant tachycardias when drugs or catheter ablation fail are class IIa indications. The success rate typically exceeds 95% with catheter ablation for these arrhythmias, so pacing is rarely used. Atrial fibrillation, atrial flutter, and atrial tachycardia are common in patients with sinus node dysfunction and an implanted pacemaker. Some devices have atrial fibrillation-prevention algorithms, including rate-adaptive atrial overdrive pacing, pacing to suppress premature atrial complexes, and rate response to limit the rate of decrease in heart rate after exercise. Some devices also provide atrial antitachycardia pacing therapy, which is about 50% effective in terminating organized atrial arrhythmias. These algorithms have been shown to reduce the overall burden of atrial arrhythmias in some patient populations.36–40 However, important improvements in clinical outcomes have not been shown, limiting the role of pacing for prevention or termination of atrial arrhythmias to patients who also have another device indication. Implantation of a pacemaker for prevention, reduction, or treatment of atrial arrhythmias is a class IIb indication. In patients with an implanted pacemaker and recurrent symptomatic atrial arrhythmias, consideration could be given to the use of a device with atrial antitachycardia pacing capabilities. However, in patients with atrial tachyarrhythmias and no bradycardia pacing indication, atrial ablation is offered for patients who are candidates, whereas AV nodal ablation and pacing controls symptoms when atrial ablation is not appropriate.
Hypertrophic Cardiomyopathy
Standard indications for permanent pacing related to sinus node dysfunction or AV block, discussed above, apply equally to patients with hypertrophic cardiomyopathy (HCM). Patients who undergo transcatheter septal ablation to alleviate an outflow gradient have an estimated 11% chance of developing subacute complete heart block, and they are treated with dual-chamber permanent pacing.41 Although an additional class IIb indication exists for the use of dual-chamber pacing in patients with HCM who have a demonstrable significant left ventricular outflow gradient and continue to have symptoms despite medical and/or surgical treatment, randomized trials have not demonstrated that this intervention significantly improves symptoms or outcomes.42–44 Indications for ICD therapy in patients with HCM are discussed in a subsequent section (see Indications for the implantable cardioverter-defibrillator).
Congestive Heart Failure
One-quarter to one-third of patients with congestive heart failure have left bundle branch block,45 which has been associated with increased mortality.45,46 With left bundle branch block, the left ventricle is initially activated at the anteroseptum, with delayed activation and contraction of the left ventricular lateral wall (Fig. 3.15). This dyssynchrony of ventricular activation leads to impaired pumping efficiency. In selected patients with refractory heart failure, pacing both ventricles (referred to as biventricular pacing or cardiac resynchronization therapy [CRT]) restores synchrony and improves exercise tolerance, clinical and biochemical markers of heart failure, ejection fraction, quality of life, and survival.47–52 The left ventricle is most commonly paced by placing an electrode in a coronary sinus tributary (Fig. 3.16). The implant technique is discussed in detail in Chapter 5. Most patients with depressed ventricular function and heart failure are also at risk for sudden cardiac arrest due to ventricular tachyarrhythmias, and they commonly receive a device capable of both resynchronization and defibrillation (CRT-D, as opposed to a device solely for resynchronization pacing [CRT-P]). The indications for CRT-D are discussed in a subsequent section (see Indications for the implantable cardioverter-defibrillator).
Fig. 3.15 Sequence of left ventricular activation in patients with left bundle branch block. The left ventricular lateral wall is depolarized last and leads to dyssynchronous global ventricular function that impairs hemodynamics.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree