Type
Subtype
Thoracic indexes
Diagnostic indexes
Assessment indexes
Most commonly reported indexes
Clinical
Chest X-ray
Sternal
Haje Body Manubrial Index [2]
Haje Body Manubrial Xyphoid Index [2]
Severity
Deformity
Configuration Index [7]
Frontosagittal Index [16]
Chest CT scan
Sternal
Haje Width Length Index [1]
Severity
Modified Haller Index
For carinatum [7]
Deformity
Vertebral Index [28]
Frontosagittal Index [28]
Steepness Index [27]
Excavatum Volume Index [27]
Unbalance Index [28]
Flatness Index [29]
Circularity Index [29]
Cardiac
Cardiac Compression Index [31]
Cardiac Asymmetry Index [31]
Modified Cardiac Compression Index [24]
Chest and cardiac MRI
Sternal, severity, deformity and cardiac
All the aforementioned
Othera
Stress cardiac ultrasound [38]
Pletismography [39]
It must be pointed out however that, even though cardio-pulmonary function tests are rarely indicated for surgical decision making, evaluation of the impact of the sternal depression on the lung and heart are helpful for achieve a full diagnosis of the defect, deal with health insurance companies and enable the patient and family understand that the PE is not only an aesthetic problem.
Validation
Validation is the confirmation of the experience or judgment of one author by another and is achieved by repeating another author’s work and reaching the same results. The same materials, methods, inclusion and exclusion criteria have to be used. Publishing the validated results is encouraged to reinforce the author’s original experience and findings. The Haller Index cut-off point of 3.25 used for surgical indication, for example, has never been validated by other authors, even though a great deal of chest wall malformation experts use it routinely in their practice. Although a huge variety of indexes have been described in the literature, only few authors have validated some of them. An example of validation is the recent publication of Poston et. al. in which the Correction Index described by St. Peter et al. was analyzed obtaining similar results than those obtained by the original authors.
Description
The most frequently reported thoracic indexes will be hereby described.
Clinical Indexes
Anthropometric Index
As stated by its authors, the Anthropometric Index (AI) is a quickly administered and low-cost clinical assessment tool, which does not induce any adverse effects and is not vulnerable to environmental influences. The A and B clinical measurements are carried out with the patient in a horizontal supine position on a flat table parallel to the floor during deep inhalation. The A measurement is defined as the largest anteroposterior diameter at the level of the distal third of the sternum, and the B measurement, as the largest depth at the same level.
The AI for PE is calculated by dividing B by A (Fig. 7.1) [5]. The AI cut-off point for PE pre- and postoperatively is 0.12.
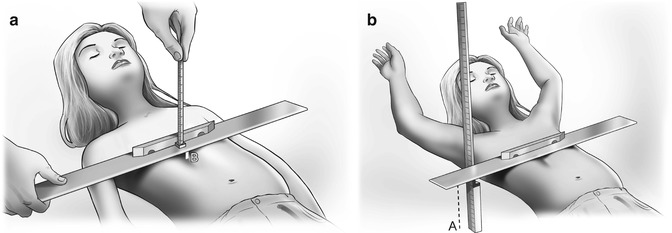
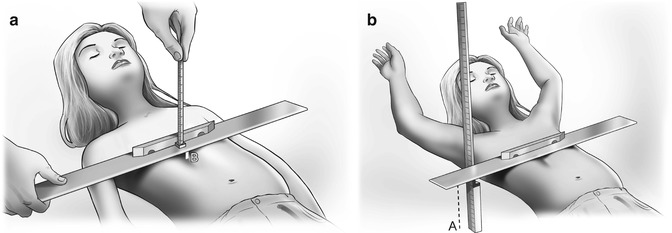
Fig. 7.1
Schematic representation of a PE patient for the calculation of the Anthropometric Index. (a) measurement of the anteroposterior distance during deep inhalation at the distal third of the sternum. (b) measurement during deep inhalation at the greater depth, at the distal third of the sternum. The instruments used were: an articulated square, a rigid ruler coupled to a level (the measuring device), a pinned limiting device and a conventional ruler
Anthropometric Index = B/A
The case series presented by Rebeis et al. [10] exhibited significant difference between male and female patients. The authors believed that the breasts accounted for this difference because measurements A and B were obtained using gauging devices that run across the chest. This belief is supported by no difference being found between male and female preteen subjects (3–10 years), when the breasts have not yet been developed. Authors such as Knutson [11] and Horst et al. [12] endorse the AI.
Chest X-ray Indexes
Because direct measurements are subject to variations in age, height, and body mass, radiographic indexes were also developed.
Vertebral Index
Authors such as Rebeis et al. [10], Welch [17], Backer et al. [13], Hummer and Willital [15], Haller et al. [22], and Derveaux et al. [7] formulated individual indexes to quantify the severity of the deformity and/or to enable the comparison between preoperative and postoperative results more objectively. All of them have in common that their indexes relate the approximation of the sternum to the spinal column. The Vertebral Index (VI) is calculated from a lateral thoracic radiography. It is defined as the ratio between the sagittal diameter of the vertebral body (BC) and the sagittal anteroposterior diameter of the posterior side of the sternum until the posterior side of the vertebral body (AC). The Lower Vertebral Index (LVI) is calculated at the xiphisternal junction [7, 10], whereas the Upper Vertebral Index (UVI) is calculated at the sternomanubrial junction [7].
Rebeis et al. [10] found that the LVI cut-off point for PE patients pre-operatively is within the means published by Derveaux et al., that is, 0.292 ± 0.067 (Fig. 7.2). Derveaux et al. [7] proposed three Chest-X-Ray indexes. The LVI (age dependent) was measured at the xiphisternal junction and calculated by BC/AC. The UVI (age independent) was measured at the sternomanubrial junction and calculated by EF/DF. The Configuration Index (ConI) was the result of the ratio between DE/AB where DE and AB are the sagittal anteroposterior diameter of the back side of the sternum to the front side of the vertebral body, at the xiphisternal and sternomanubrial junctions, respectively. The ConI was particularly valuable in patients with complex PE, often with axial sternal rotation and/or scoliosis (Fig. 7.2). Mean pre-operative UVI was equal to 0.235 ± 0.045. Mean pre-operative ConI was equal to 1.175 ± 0.214. The results obtained regarding LVI were compatible with those of Ohno et al. who expressed results as a percentage ratio. The pre-operative cut off point for LVI > 27 [16].
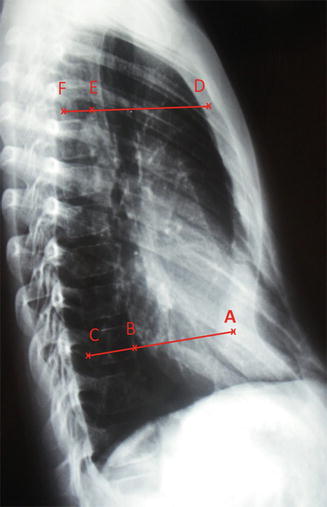
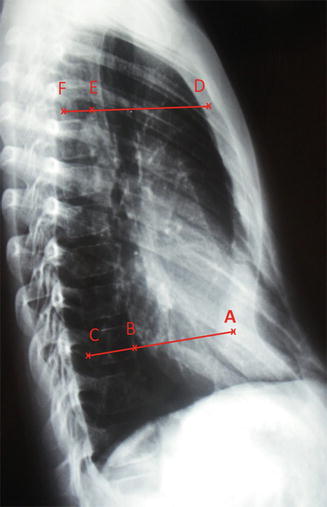
Fig. 7.2
Lateral Chest-X-Ray of a PE patient. Note Rebeis et al. and Derveaux et al. measurements to calculate the Lower Vertebral Index at the xiphisternal junction. BC = sagittal diameter of the vertebral body and AC = sagittal anteroposterior diameter of the back side of the sternum to the back side of the vertebral body. Derveaux et al. also measure the Upper Vertebral Index at the sternomanubrial junction. EF = sagittal diameter of the vertebral body and DE = sagittal anteroposterior diameter of the back side of the sternum to the back side of the vertebral body. The Configuration Index is the ratio between the sagittal anteroposterior diameter of the back side of the sternum to the front side of the vertebral body at the xiphisternal (DE) and sternomanubrial (AB) junctions
Lower Vertebral Index = BC/AC Upper Vertebral Index = EF/DF Configuration Index = DE/AB
Frontosagittal Index
According to Ohno et al. the Fronto Sagittal Index (FSI) is the percentage ratio between maximum internal transverse diameter (T) and minimum sagittal diameter of the chest, measured from the anterior surface of the vertebral body to the nearest point on the sternal body (D).
The authors concluded that the LVI decreased whereas the FSI increased significantly post-operatively (Fig. 7.3). They suspected that the abnormal post-operative indexes were the result of thin and flat chests, because of the short sagittal diameter of the thoracic cage, even though the sternum was adequately elevated and PE patients were satisfied with the cosmesis. The pre-operative cut off point for FSI < 29 [16].
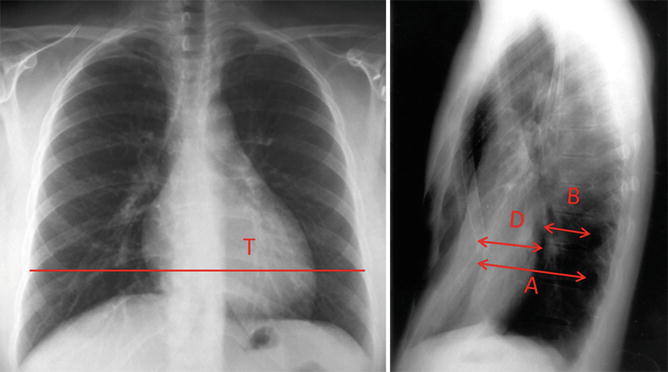
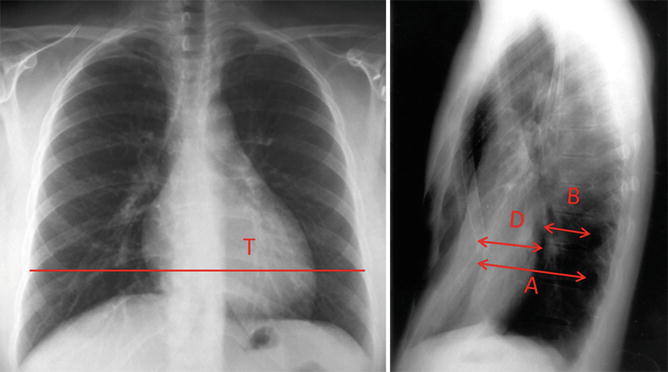
Fig. 7.3
PA and lateral Chest-X-Rays of a PE patient. Lower Vertebral Index: percentage ratio between minimum sagittal diameter of the chest measured from the posterior surface of the vertebral body to the nearest point on the sternal body (A) and the sagittal diameter of the vertebral body at the same level. (B) Fronto Sagittal Index: percentage ratio between maximum internal transverse diameter (T) and minimum sagittal diameter of the chest, measured from the anterior surface of the vertebral body to the nearest point on the sternal body (D)
Lower Vertebral Index = (B/A) × 100 Fronto Sagittal Index = (D/T) × 100
Welch Index
In 1958, Welch reported a technique for the correction of PE that emphasized total preservation of the perichondrial sheaths of the costal cartilage, preservation of the upper intercostal bundle, sternal osteotomy and anterior fixation of the sternum with silk sutures [17]. By the year 1988, Shamberger and Welch, had surgically corrected 704 PE patients with the same technique. Severity of the deformities was assessed on a scale 1–10 based on a series of measurements made from chest-x-rays (Fig. 7.4) [18]. According to the authors, surgical repair is recommended for PE patients beyond infancy with an inflexible deformity and a severity rating Welch Index (WI) of ≥5.
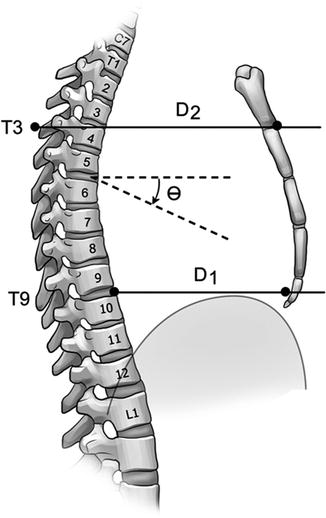
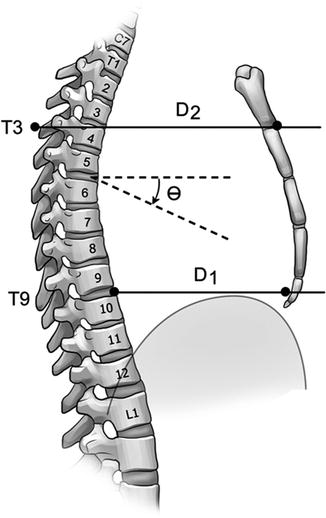
Fig. 7.4
Welch’s method of grading severity of the deformity (Welch Index) uses the distance from the anterior surface of the spine at T-9 to the posterior surface of the sternum (D-1), over the distance from the spinous process of T-3 to the angle of Louis (D-2). Additional 0.5 is added if the rib angle (Ø) is greater than 25° or the cardiothoracic ratio is >50 %
By calculating the:
The Welch Index is equal to:– DG + 0.5 if Rib angle (Ø) > 25°and/or DG + 0.5 if the Cardiothoracic ratio >50 %
1.
Depression ratio (DR) = D1/D2,
2.
Deformity Grade (DG) = (1−DR) × 10 and the,
3.
Cardiothoracic Ratio = maximal horizontal cardiac diameter/maximal horizontal thoracic diameter (inner edge of ribs/edge of pleural) multiplied by 100. It is measured form a PA Chest-X-Ray. Normal values are <50 %.
Haje Body Manubrial Index
This sternal index has been proposed by Haje et al. It is obtained from a lateral chest X-ray. To calculate it, the length of the manubrium and body of the sternum are measured in centimeters. A ratio resultant of the division of the length of the ossified body (B) by the length of the ossified manubrium (M) is called the Body Manubrium (BM) Index [2] (Fig. 7.5). It cannot be obtained when sternal segments are fused.
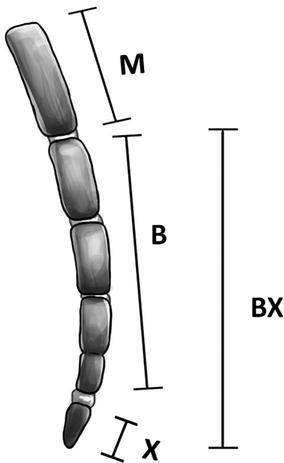
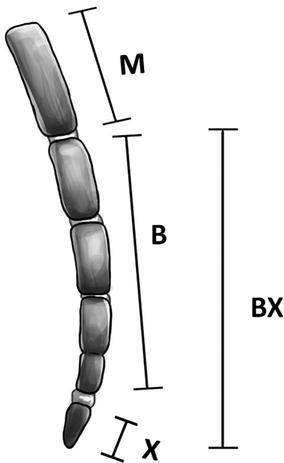
Fig. 7.5
Diagram of the measurements done on the lateral view of the sternum. (M) Manubrium length; (B) Body length; (BX) Body-Xyphoid distance. A lateral radiograph of a normal 11-year-old patient was used as a model
Body Manubrium Index = B/M
Haje Body Manubrium Xyphoid Index
This sternal index has also been proposed by Haje et al. It is obtained from a lateral Chest-X-Ray when ossification of the xyphoid process (X) is observed. A new ratio, representing the distance in centimeters from the top of the body to the bottom of the xyphoid process (BX) divided by the length of the manubrium (M), is obtained and called the Body Manubrium Xyphoid (BXM) Index (Fig. 7.5) [2].
Body Manubrium Xyphoid Index = BX/M
The sternal body in controls is slightly more than twice the length of the manubrium. The cut-off point for the BM Index is 2.16 and for the BMX Index is 2.73. Lower BM values depict shorter sternal bodies.
The study originally aimed to determine the influence of sternal growth on the development of pectus deformities and correlate imaging studies with clinical aspects of different types of deformities. Although it was not Haje’s main objective, when considering the BM and the BMX sternal indexes from a surgical point of view, these indexes might be useful to define surgical strategies as for example to predict the number of pectus bars needed for a Nuss procedure by correlating sternal length, age and thoracic elasticity.
Chest-X-ray Haller Index
The Haller Index (HI) will be explained in detail further in this chapter. It derives from dividing the greater transverse diameter (the horizontal distance of the inside of the ribcage) by the anteroposterior diameter (the shorter distance between the vertebrae and the sternum).
Poston et al. determined PE severity from Chest-X-Rays, instead of Chest CTs, to minimize radiation exposure of PE patients. Authors found a strong correlation between HIs calculated from Chest-X-Rays (Chest-X-Ray HIs) and those by Chest CT Scans. Both HIs demonstrated good inter-rater reliability. Nonetheless, even though the sensitivity of Chest-X-Rays in diagnosing severe PE (Chest CT HI ≥ 3.2) resulted high, specificity was less convincing. But when using a cut-off point for Chest-X-Ray HIs of 3.75 or greater, combined specificity resulted quite high (0.96). They finally suggested using Chest CT Scans as a confirmatory test for Chest- X-Ray HIs between 3.2 and 3.75 [19].
According to Khanna et al. [20], Chest-X-Ray HI correlates strongly with Chest CT HI, has good inter-observer correlation, and a high diagnostic accuracy for pre-operative evaluation of PE. Authors suggest that a Chest CT is not required for pre-operative evaluation of PE, and a two-view Chest-X-Ray is sufficient enough for preoperative imaging of the defect.
Mueller et al. [21] measurements, calculated from preoperative Chest-X-Rays yielded HIs equivalent to those taken from Chest CT Scans. Authors postulated that the replacement of preoperative Chest CT by radiographies would reduce unnecessary exposure to radiation in children with asymptomatic PE. They believe this is particularly desirable because radiation exposure may have long-term side effects in growing children that range from long bone growth derangements to fatal malignancies. When in doubt, a Chest CT Scan could be indicated for the preoperative evaluation (Fig. 7.6).
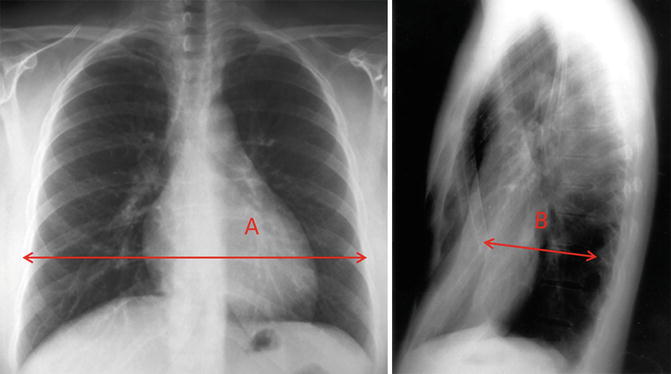
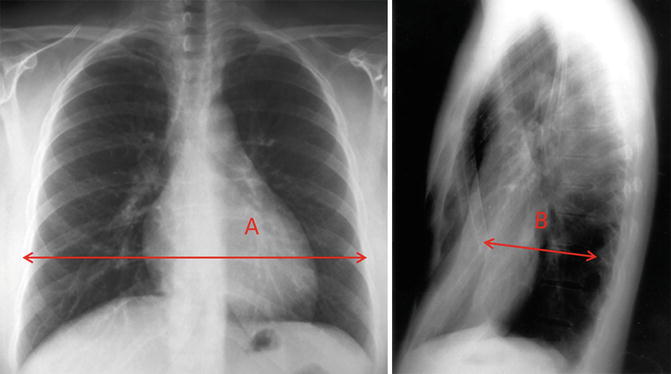
Fig. 7.6
Chest–X–Ray Haller Index measurement on two-view chest radiography. (A) The point of most posterior projection of the sternum is identified, and the distance between that segment and the anterior aspect of the corresponding vertebra is measured. (B) The lateral diameter is measured at the vertebral body level on the anteroposterior view
Chest–X–Ray Haller Index = A/B
Chest Scan Indexes
Haje Width Length Index
This index was proposed by Haje et al. from coronal CT Scans, traced out on a schematic representation of the anterior chest wall. The Width Length Index (WLI) is calculated by dividing the maximum width of the ossified sternal body by its length (Fig. 7.7). This implies higher WLI indexes for wide sternal bodies, with possible connotations for the prognosis and treatment of different types of pectus deformities [1]. The mean WLI Index for controls is 0.420. The mean WLI Index for PE patients is >0.446.
Fig. 7.7
Lines W (widest length of the ossified sternal body) and L (longest length of the ossified sternal body), are used for the study of the WL index in coronal CT Scans. The Width Length Index is calculated by the division of W by L
Width Length Index = W/L
Sternal Depression Index
The Sternal Depression Index (SDI) is the ratio between the maximal internal sagittal diameter of the left side of the chest (C) and the minimal distance between the anterior surface of the vertebral column and the posterior border of the deepest portion of the sternum (B).
The vertical distance between the higher and lowest point of the anterior chest wall (A) is a measure of the sternal depression.
Chu et al. [30] reported that the average depth of depression of the sternum (A) was 21 ± 7 mm whereas the SDI was 2.7 ± 1.4. When the SDI was arbitrarily used to classify the severity of sternal deformity, mild sternal deformity was associated to a SDI < 2.4; moderate sternal deformity was associated to a SDI between 2.4 and 2.9; and severe sternal deformity was associated to a SDI index >2.9 (Fig. 7.8). As the depression index increased, the cardiac rotation angle (Ø) increased with a correlation coefficient of 0.75.
Fig. 7.8
Chest CT Scan showing measurements to calculate the depth of sternal depression (A), Sternal Depression Index (C/B), and cardiac rotation angle (Ø). D = sagittal line from anterior border of the vertebral body and line from anterior border of vertebral body (E)
Haller Index
The Haller Index (HI), described in 1987 by Dr. Haller J, Dr. Kramer and Dr. Lietman, is a mathematical relationship, usually measured by chest CT scans [22]. As aforementioned, HI derives from dividing the transverse diameter (the widest horizontal distance of the inside of the ribcage) [T] by the anteroposterior diameter (the shorter distance between the vertebrae and the sternum) [A] (Fig. 7.9) [23].
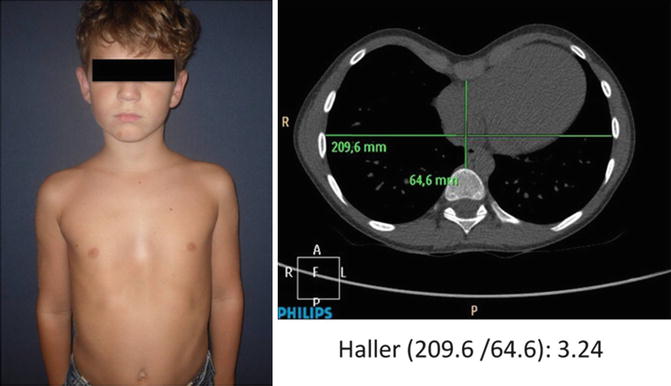
Fig. 7.9
CT axial image: Calculation of the Haller Index = 91 mm/16 mm = 5.68. The sternum is so severely depressed that it is 1.6 cm from the anterior portion of the vertebra
Haller Index = T/A
Despite several issues that will be discussed further, the HI remains a useful tool in judgment of operative indication. The cut-off point for PE patients is >3.25 [22].
The HI has been chosen as the gold standard for the majority of chest wall malformation experts. Presumably because it is easy to measure, and because surgeons and radiologists are used to calculate and interpret it. Moreover, it has a high inter-observational reliability as demonstrated by Lawson et al. [41] Nonetheless, it is thoroughly documented that the HI has several limitations (Table 7.2).
To start with, there is no convincing evidence regarding it provides accurate information to guide surgical correction of PE. Its cut-off point is quite variable among authors. Daunt et al. [4] for instance proposed an upper limit of 2.7, Khanna et al. [20] of 3.2, Kilda et al. [43] of 3.1 whereas most chest wall malformation experts adopt a cut-off point equal or greater than 3.25. In spite of this, as Lawson et al. [41] published, there is a considerable variability among medical practitioners in determining the HI depending on how the images are chosen and how measurements are taken from the chosen images. Secondly, the HI might be unreliable since it varies with age, gender [4, 5], thoracic shape [2, 5], and whether it is done in inspiration or expiration [30]. Thirdly HI is unpractical for surgical – decision making as it does not consider asymmetry [24], percentage of sternal and costal depression [24], cardiac compression or cardiac asymmetry [41, 44]. Also results from controls and PE patients overlap between each other [26]. While width serves as a surrogate for comparing dimensions of the chest, it does not depict the position of the sternum relative to the anterior ribcage. A wide chest increases HI whereas a narrow chest decreases HI regardless of the severity of the PE [24]. HI bares no conclusive relationship with the aesthetic complaints observed. For instance, the patient in (Fig. 7.10) clearly has a PE. But when calculating his HI it is equal to 3.24. St. Peter et al. proposed the Correction Index (CI), a novel thoracic index, which is independent of chest width and assesses the percentage of chest depth [26]. The CI will be described ahead in this chapter.