Takotsubo cardiomyopathy (TC) is a medical entity mimicking an acute coronary syndrome (ACS). Ventricular arrhythmia (VA) in TC has been reported in small studies, leading to uncertain knowledge of its incidence. We sought to describe the characteristics, incidence, predictive factors, and outcomes of VA in patients presenting with TC. Over a 12-year period, we reviewed all patients (n = 5,484) referred to our coronary care unit for a suspicion of ACS. TC was diagnosed in 90 patients according to the Mayo Clinic criteria. Incidence of VA among TC was 10%. In multivariate analysis, the factors significantly associated with an increased risk of VA were syncope (p = 0.007), age <55 years (p = 0.008), atypical TC (p = 0.04), a troponin I peak >7 μg/L (p = 0.04), and dobutamine use during hospitalization (p = 0.04). During follow-up, there was no significant difference in mortality rate between patients with or without VA. In conclusion, VA occurred in 10% of patients at the acute phase of TC and independent predictive factors of VA were syncope, atypical pattern of TC, high troponin peak, dobutamine use, and a relatively young age in a female and menopausal population. During the acute phase, identification of high-risk patients with VA allows better management, with electrocardiographic monitoring and therapeutic intervention in the coronary care unit.
Takotsubo cardiomyopathy (TC) is a medical entity mimicking acute coronary syndrome (ACS) and is characterized by distinctive and reversible left ventricular (LV) systolic dysfunction, not mediated by epicardial coronary artery obstruction. In the clinical setting, TC must be promptly individualized from ACS for its appropriate management. Prognosis of TC is generally favorable, but some serious complications may occur at the acute phase: heart failure, cardiogenic shock, right ventricular involvement, LV outflow tract obstruction, mitral regurgitation, and LV mural thrombus formation. Nevertheless, one of the less described complications is the occurrence of ventricular arrhythmia (VA). Consequently, the incidence of VA in the setting of TC and its clinical significance are not well known. The aims of the study were to (1) assess the incidence of VA at the acute phase of TC, (2) determine the predictive factors of VA, and (3) assess the prognosis of VA.
Methods
Over a 12-year period (from January 2001 to April 2013), we reviewed all consecutive patients referred to our coronary care unit (CCU) for ACS (n = 5,484). Criteria for selection included patients aged >18 years and with a clinical presentation of ACS. Patients were excluded if no coronary angiography was performed. All the clinical records were studied and reviewed, including demographics, cardiovascular risk factors, medical history, history of ACS, previous treatment before admission, and clinical examination at admission and electrocardiogram (ECG), echocardiographic and laboratory data, coronary and LV angiography, management during hospitalization, treatment at discharge, and inhospital and end of follow-up outcomes.
All patients underwent coronary angiography. Significant coronary artery stenosis was defined as at least 50% diameter narrowing. All patients without significant coronary artery stenosis or patients presenting with a suspicion of TC underwent LV angiography.
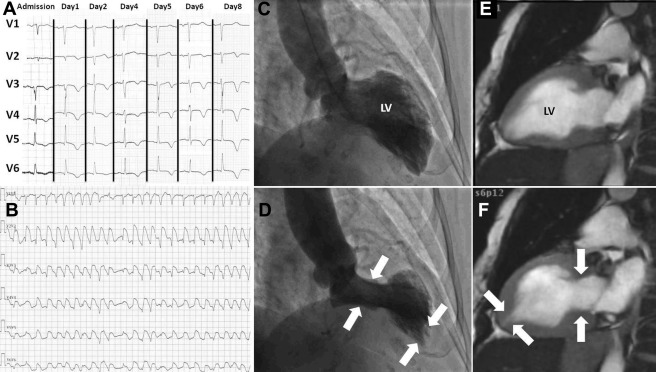
All cardiac examinations of patients with suspected TC were routinely reviewed by 3 independent experts blinded to the clinical data. They reviewed ECG, coronary angiography, LV angiography, echocardiography, and cardiac magnetic imaging. TC was defined according to the Mayo Clinic criteria and if there was full agreement between the experts. A follow-up of LVEF was carried out among the patient population suspected from a TC diagnosis. The normalization of the LVEF during follow-up was absolutely required to prove that TC was correctly diagnosed. We individualized patients presenting a typical pattern of TC (mid and apical LV systolic dysfunction) from patients presenting atypical TC (apical-sparing variant or inverted TC).
In the CCU, all patients were continually monitored by 12-lead ECG during at least 3 days to detect the occurrence of VA. Data from the monitoring ECG were reviewed by a cardiologist (OA) to confirm the diagnosis of VA. Occurrence of VA was defined according to guidelines, allowing to individualize nonsustained and sustained ventricular tachycardia (VT) and ventricular fibrillation (VF).
Statistical analysis was performed with R Studio, version 5.1 (R Studio, Boston, Massachusetts) and STATA 12.0 (Stata-Corp, College Station, Texas). Continuous variables are presented as mean ± SD and range, unless otherwise specified, and were compared using Student’s t test. Categorical data are presented as absolute values and percentages and compared using the chi-square test or Fisher’s exact test as appropriate. Binary variables were created from continuous variables using a cutoff point defined either by statistical values as mean, median, or interquartile range or by physiological or pathophysiological values. Associations with VA were first established invariably. Then, we performed a multivariate logistic regression analysis to identify sets of factors that together are significantly associated with the occurrence of VA. Variables introduced in the multivariate logistic regression were selected according to clinical criteria (age <55 years [rather than nonmenopausal women] and gender), laboratory values (troponin peak level >7 μg/L [75th percentile] and significant hypokalemia defined as serum potassium concentration <3 mmol/L), and the TC pattern (typical or atypical) with a p value <0.20 in univariate analyses. The adjusted odds ratio (aOR) was calculated with a 95% confidence interval (CI). All the tests were 2 sided, and the results were considered significant at p <0.05. Follow-up was obtained by consultation, by phone contact, or by consulting the French Center on Medical Causes of Death (CepiDc-INSERM). Cumulative mortality rates were estimated with the Kaplan-Meier method, and differences were tested with a log-rank test.
Results
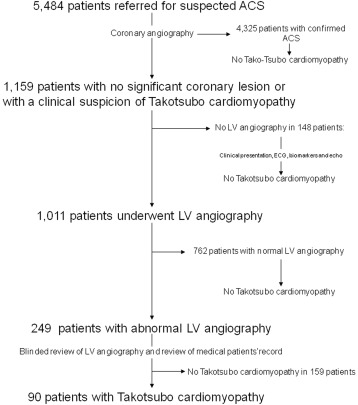
The study population included 5,484 consecutive patients referred for suspected ACS (3,805 men and 1,679 women, mean age 65.5 ± 12 years, range 20 to 96 years, Table 1 and Figure 1 ). A final diagnosis of ACS was made in 4,325 patients. Among patients without a diagnosis of ACS (n = 1,159), LV systolic dysfunction was found in 249 patients.
| Suspected ACS (n = 5484) | TC (n = 90) | P | |
|---|---|---|---|
| Mean age (years) | 65.5± 12 | 71.9±12.7 | <0.001 |
| Women | 1679 (30%) | 87 (97%) | <0.001 |
| Current smoker | 2106 (38%) | 25 (28%) | 0.04 |
| Hypertension | 2508 (47%) | 41 (46%) | 0.97 |
| Diabetes mellitus | 943 (17%) | 8 (9%) | 0.04 |
| Dyslipidemia | 2536 (46%) | 26 (29%) | 0.001 |
| Family history of CAD | 965 (18%) | 7 (8%) | 0.01 |
| In-hospital mortality | 286 (5%) | 2 (2%) | 0.20 |
| Duration of hospitalization (days) | 4.7±4.6 | 9.8±9.2 | 0.001 |
A diagnosis of TC was confirmed in 90 patients (mean age 72 ± 13 years). Prevalence of TC was 2.1% in the population of ACS. Baseline characteristics of patients are presented in Table 2 . A precipitating factor was found in 76% of patients. Most patients presented with chest pain (63%), whereas syncope was found in 8%. At admission, T-wave inversion was the most common ECG finding (63%). Transient QT interval prolongation occurred in 43% of patients (mean corrected QT interval: 446 ± 49 ms). We did not observe any bradyarrhythmias (AV block, asystole) during hospitalization. Mean peak of troponin was 6.4 ± 8.8 μg/L (range 0.01 to 52 μg/L). Mean serum potassium was 4.2 ± 0.54 mmol/L (range 2.7 to 5.4 mmol/L) at admission, and its lowest value during hospitalization was 3.84 ± 0.45 mmol/L (range 2.5 to 5.2 mmol/L). Treatment by vasoactive drugs was initiated in 11 patients (dobutamine infusion in 8 patients and norepinephrine infusion in 3 patients) for arterial hypotension or cardiogenic shock.
| Variables | All Patients Presenting With TC (n = 90) | Ventricular Arrhythmia | P | |
|---|---|---|---|---|
| No (n = 81) | Yes (n = 9) | |||
| Mean age (years) | 72 ± 13 | 73 ± 12 | 62 ± 17 | 0.01 |
| Female | 87 (97%) | 78 (96%) | 9 (100%) | 0.98 |
| Female < 55 years | 7 (8%) | 4 (5%) | 3 (33%) | 0.02 |
| Psychiatric history | 17 (19%) | 16 (20%) | 1 (11%) | 0.49 |
| Current smoker | 25 (28%) | 24 (30%) | 1 (11%) | 0.43 |
| Hypertension | 41 (46%) | 38 (47%) | 3 (33%) | 0.67 |
| Diabetes mellitus | 8 (9%) | 7 (9%) | 1 (11%) | 0.98 |
| Dyslipidemia | 26 (29%) | 23 (28%) | 3 (33%) | 0.99 |
| Family history of CAD | 7 (8%) | 6 (7%) | 1 (11%) | 0.98 |
| Systolic blood pressure (mmHg) | 125±29 | 127±29 | 104±22 | 0.02 |
| Diastolic blood pressure (mmHg) | 75±17 | 76±18 | 67.4±13 | 0.14 |
| Heart rate (bpm) | 88±19 | 88±19 | 87±16.5 | 0.80 |
| Chest pain | 57 (63%) | 52 (64%) | 5 (55.5%) | 0.88 |
| Syncope | 7 (8%) | 4 (5%) | 3 (33%) | 0.02 |
| Dyspnea | 17 (19%) | 13 (16%) | 4 (44%) | 0.11 |
| Sudden cardiac arrest | 1 (1%) | 0 (0%) | 1 (11%) | 0.10 |
| No symptoms | 6 (7%) | 6 (7%) | 0 (0%) | 0.99 |
| Precipitating factor | ||||
| Emotional stress | 37 (41%) | 33 (41%) | 4 (44%) | 0.97 |
| Medical stress | 25 (28%) | 20 (24.5%) | 5 (55%) | 0.31 |
| Surgical stress | 11 (13%) | 9 (11%) | 2 (22%) | 0.66 |
| None | 22 (27%) | 21 (26%) | 1 (11%) | 0.56 |
| Electrocardiogram | ||||
| Sinus rhythm | 83 (92%) | 74 (91%) | 9 (100%) | 0.79 |
| New atrial fibrillation | 12 (13%) | 12 (15%) | 0 (0%) | 0.60 |
| ST-segment elevation | 39 (44%) | 36 (44%) | 3 (33%) | 0.99 |
| New LBBB | 5 (6%) | 5 (6%) | 0 (0%) | 0.99 |
| T-wave inversion | 57 (63%) | 52 (64%) | 5 (55%) | 0.74 |
| Corrected QT interval (ms) | 446 ± 50 | 447 ± 52 | 439 ± 46 | 0.63 |
| QT prolongation (>450 ms) | 39 (43%) | 36 (44%) | 3 (33%) | 0.67 |
| Initial average of LVEF | 42.3±9.5 | 42.5±9.9 | 40.4±5.7 | 0.72 |
| Coronary stenosis < 50% | 14 (15.5%) | 12 (15%) | 2 (25%) | 0.60 |
| LVOT obstruction | 10 (11%) | 8 (80%) | 2 (20%) | 0.27 |
| Congestive heart failure | 23 (26%) | 19 (23.5%) | 4 (44%) | 0.22 |
| Cardiogenic shock | 10 (11%) | 6 (7%) | 4 (44%) | 0.007 |
| Variant of TC | ||||
| Apical | 63 (71%) | 60 (95%) | 3 (5%) | 0.03 |
| Apical-sparing variant | 26 (28%) | 20 (77%) | 6 (23%) | 0.03 |
| Inverted | 1 (1%) | 1 (100%) | 0 (0%) | / |
| Troponin peak (μg/L) | 6.4±8.8 | 5.98±8.6 | 10.27±10.1 | 0.17 |
| CK peak (U/L) | 363±663 | 336.07±619.9 | 591.22±977 | 0.27 |
| Serum potassium (mmol/L) ∗ | 3.8±0.4 | 3.85±0.4 | 3.72±0.7 | 0.41 |
| Hospitalization treatment | ||||
| Defibrillation | 3 (3%) | 0 (0%) | 3 (33%) | 0.0007 |
| Aspirin | 77 (85%) | 70 (86%) | 7 (78%) | 0.61 |
| Heparin | 63 (70%) | 56 (69%) | 7 (78%) | 0.71 |
| Beta-blockers | 16 (18%) | 14 (17%) | 2 (22%) | 0.65 |
| ACE inhibitor/ARA | 31 (34.5%) | 28 (35%) | 3 (33%) | 0.99 |
| Diuretics | 21 (23%) | 18 (22%) | 3 (33%) | 0.74 |
| Nitroglycerin | 16 (18%) | 15 (18.5%) | 1 (11%) | 0.99 |
| Dobutamine | 8 (9%) | 5 (6%) | 3 (33%) | 0.03 |
| In-hospital mortality, n (%) | 2 (2%) | 2 (2.5%) | 0 (0%) | 0.97 |
| Duration of hospitalization, days | 9.8±9.2 | 9.7±9.5 | 11.3±6.6 | 0.62 |
VA was documented in 9 patients (9 women, mean age 62 ± 17 years [range 32 to 87], Table 2 , Figure 2 ) and was always detected in the first 48 hours of hospitalization. Patients with VA were significantly younger (p = 0.01) and had lower systolic blood pressure (p = 0.02). Incidence of VA in our patients presenting with TC was 10%. VA was distributed as follows: VT in 89% (n = 8; nonsustained VT/sustained VT ratio: 3/1) and VF in 11% (n = 1). Concerning therapeutic interventions, dobutamine infusion was more frequently used in patients with VA at admission (p = 0.03). There was no difference between QT interval prolongation in the 2 groups (p = 0.38). Patients presenting cardiogenic shock developed VA more frequently during hospitalization (p = 0.007), but no significant difference was observed in the case of LV outflow tract obstruction (p = 0.27). The presence of a significant coronary lesion on angiography was not significantly linked to the occurrence of VA (p = 0.60). No recurrent VA was observed.
Univariate analyses are presented in Table 3 . The multivariate analysis ( Table 4 ) identified variables independently associated with the occurrence of VA: syncope (aOR 82.5, 95% CI 3.3 to 2,032, p = 0.007), age <55 years (aOR 9.5, 95% CI 1.7 to 52.6, p = 0.009), atypical pattern of TC (aOR 13, 95% CI 1.09 to 175, p = 0.04), high level of troponin (aOR 14, 95% CI 1.11 to 194, p = 0.04), and use of dobutamine infusion (aOR 28.7, 95% CI 1.1 to 708, p = 0.04) were independently related to the occurrence of VA at the acute phase of TC.
| Univariate Predictor | Unadjusted Odds-Ratio | 95% Confidence Interval | P |
|---|---|---|---|
| Age <55 yrs | 9.5 | 1.7-52.6 | 0.01 |
| Sex | 1 | / | / |
| Troponin peak > 7 μg/L | 2.4 | 0.4-12.7 | 0.19 |
| Serum potassium <3.0 mmol/L | 6 | 0.4-68.5 | 0.08 |
| Creatinine | 0.97 | 0.11-1.01 | 0.06 |
| Syncope | 9.6 | 1.7-53.5 | 0.01 |
| Cardiogenic shock | 9.86 | 2.1-46.7 | 0.004 |
| Systolic blood pressure | 0.96 | 0.93-0.99 | 0.03 |
| Corrected QT prolongation (ms) | 0.99 | 0.97-1.02 | 0.63 |
| QT prolongation (>450 ms) | 0.5 | 0.02-12.9 | 0.67 |
| Atypical TC by echo | 4.4 | 1.01-19.5 | 0.04 |
| LVEF (LV angiography) | 0.98 | 0.91-1.07 | 0.73 |
| Treatment ∗ | |||
| Dobutamine infusion | 7.6 | 1.4-39.7 | 0.01 |
| Diuretics | 1.74 | 0.4-7.7 | 0.4 |
| ACE inhibitor/ARA | 0.94 | 0.2-4 | 0.9 |
| Beta-blockers | 3.57 | 0.4-30 | 0.2 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


