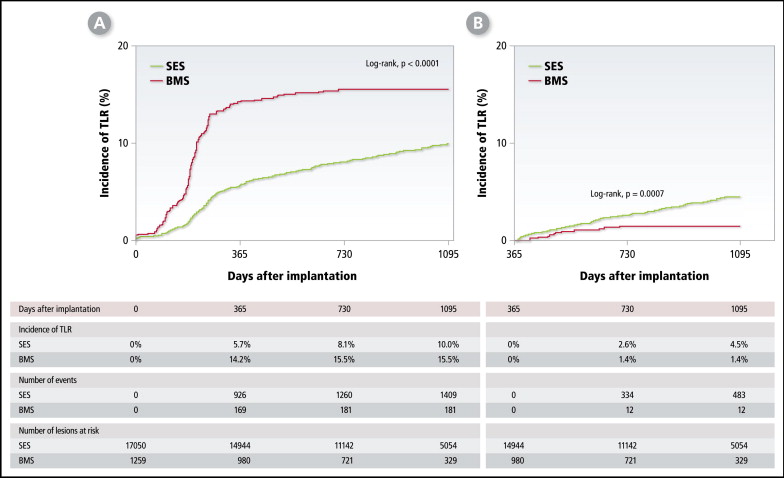
It yet has not been clarified whether there is a late catch-up phenomenon in target lesion revascularization (TLR) after sirolimus-eluting stent (SES) compared to bare metal stent (BMS) implantation. In 12,824 patients enrolled in the j-Cypher Registry, incidences of early (within first year) and late (1 year to 3 years) TLR were compared between 17,050 lesions treated with SESs and 1,259 lesions treated with BMSs. Incidences of TLR in SES-treated lesions were 5.7% at 1 year, 8.1% at 2 years, and 10.0% at 3 years, whereas those in BMS-treated lesions were 14.2%, 15.5%, and 15.5%, respectively (p <0.0001, log-rank test). Incidences of late TLR were significantly higher with SESs compared to BMSs (2.6% vs 1.4% at 2 years and 4.5% vs 1.4% at 3 years, p = 0.0007, log-rank test). A multivariable logistic regression model identified 7 independent risk factors for late TLR at 3 years after SES implantation: hemodialysis, low estimated glomerular filtration rate, ostial right coronary artery, lesion length ≥30 mm, 2 stents for bifurcation, American Heart Association/American College of Cardiology type B2/C, and vessel size <2.5 mm. Of these, 5 factors were common to those for early TLR. In conclusion, a late catch-up phenomenon was observed as indicated by the increasing incidence of late TLR after SES, but not after BMS, implantation. Risk factors for late TLR were generally common to those for early TLR.
Percutaneous coronary intervention (PCI) with bare metal stents (BMSs) often requires retreatment for restenosis, and some patients become refractory to repeated target lesion revascularization (TLR). Drug-eluting stents (DESs), including sirolimus-eluting stents (SESs), have significantly decreased the rate of restenosis and TLR compared to BMS. However, late lumen loss beyond 6 months suggesting delayed intimal hyperplasia has been reported after DES implantation. Further, a case report and results from a few studies have suggested occurrence of late TLR after DES implantation. However, there is not a large-scale study demonstrating the existence of “a late catch-up phenomenon” after DES implantation compared to BMS implantation as indicated by a differentially increasing incidence of late TLR. Furthermore, identification of risk factors of late TLR might provide an insight into the mechanism of the late catch-up phenomenon, if it does exist. However, there is thus far no report analyzing the risk factors of early and late TLR separately. In this report, we compared the incidences of early and late TLR between 2 groups of lesions treated with SESs or BMSs and evaluated risk factors for early and late TLR after SES implantation by analyzing 3-year follow-up data from the j-Cypher Registry.
Methods
The design and patient enrollment of the j-Cypher Registry has been published previously. In brief, this registry is a multicenter observational study in Japan enrolling all consecutive patients in whom placement of SESs had been attempted. Data were collected on all lesions treated during index hospitalization including those treated with BMSs. Follow-up data were obtained from hospital charts or by contacting patients and/or referring physicians at 30 days, 6 months, 1 year, and yearly thereafter. In this study, planned follow-up coronary angiography was left to the discretion of individual site investigators. Relevant review boards in all 37 participating centers approved the study protocol. Written informed consent was obtained from all patients.
From August 2004 to November 2006, 12,824 patients with 19,675 lesions were enrolled in the registry. Of these, 17,050 lesions treated exclusively with SESs and 1,259 lesions treated exclusively with BMSs constituted the study population. Treatment for the remaining 1,366 lesions involved a combination of SESs and other stent types (495 lesions), other DESs (60 lesions), nonstent PCI (672 lesions); and failed procedures (139 lesions).
The decision regarding therapeutic strategies, such as use of intravascular ultrasound and stent expansion pressure, was left to the discretion of each physician. The recommended antiplatelet regimen was aspirin indefinitely and thienopyridine for ≥3 months. Duration of therapy with thienopyridine was left to the discretion of each attending physician. Complete 1-year follow-up was achieved in 97% of patients; median duration of follow-up was 812 days (interquartile range 450 to 1,095).
In comparing SESs to BMSs, analyses were done on a lesion basis. A lesion was defined as the area covered by single or multiple overlapping stents. Lesions located within 3 mm from the ostium were regarded as ostial lesions. A bifurcation lesion was defined as that involving a side branch ≥2.2 mm in diameter. On-label use was defined according to entry criteria of the Sirolimus-Eluting Stents Versus Standard Stents in Patients with Stenosis in a Native Coronary Artery (SIRIUS) trial. Lesions with on-label indication were defined as de novo lesions <30 mm in length and 2.5 to 3.5 mm in diameter; culprit lesions of recent myocardial infarction, ostial lesions, bifurcation lesions, thrombus containing lesions, and severely calcified lesions were excluded. The latter excluded lesions and all other lesions were classified as lesions with off-label indication. Renal function was expressed as estimated glomerular filtration rate calculated by the Modification of Diet in Renal Disease formula modified for Japanese patients.
Stent thrombosis was defined according to the Academic Research Consortium definition. TLR was defined as retreatment (PCI or coronary artery bypass grafting surgery) because of a significant lesion within the stented segment or within 5 mm from the stent borders. Retreatment for stent thrombosis was included in TLR. TLR procedures were divided into those performed within the first year (early TLR) and those done >1 year after the index stent implantation procedure (late TLR).
Categorical variables were compared using chi-square test. Continuous variables were expressed as mean ± SD unless otherwise indicated and were compared using Student’s t test or Wilcoxon rank-sum test based on distribution. Cumulative incidence was estimated by the Kaplan-Meier method, and differences in rates of early and late TLR between SES-treated and BMS-treated lesions were assessed with log-rank test.
Risk factors of early and late TLR after SES implantation were analyzed separately. A multivariable logistic regression model instead of a Cox proportional hazard model was used to identify independent risk factors of early and late TLR, because restenosis has been well known to be a time-related phenomenon and the timing of TLR can be highly influenced by physicians’ and patients’ decisions. Actually, proportional hazard assumption for the variables was not verified. Using a logistic regression model, we could minimize the influence of timing of TLR on analysis of risk factors for TLR. Eligible lesions for logistic regression analysis of early and late TLR risk factors included those lesions with TLR events within the first year and from 1 year to 3 years, respectively, compared to those lesions with complete follow-up and without TLR events at 1 year and 3 years, respectively. Continuous variables were dichotomized by clinically meaningful reference values. We selected variables with a p value <0.05 in univariate models and included them simultaneously in multivariable models. Independent risk factors for early and late TLR identified by multivariable logistic regression analysis were confirmed by forward and backward procedures and expressed as odds ratios and their 95% confidence intervals.
All analyses were conducted by physicians (Y. Nakagawa and T. Kimura) and a statistician (T. Morimoto) using SAS 9.1 (SAS Institute, Cary, North Carolina) and reported p values were 2-sided.
Results
Patients with high-risk features such as age ≥80 years, diabetes, and renal failure were commonly enrolled in the registry as were complex lesions such as long-term total occlusion, long lesions, and small vessels ( Table 1 ). TLR rates on a patient basis were significantly lower in patients treated exclusively with SESs compared to those treated with SESs and BMSs (12.2% vs 25.1% at 3 years, p = 0.0001).
| Patient characteristics | |
| Age (years) | 68.4 ± 10.2 |
| Age >80 years | 1,667 (13%) |
| Men | 9,653 (75%) |
| Body mass index (kg/m 2 ) | 23.9 ± 3.39 |
| Hypertension | 9,559 (75%) |
| Diabetes mellitus | 5,320 (42%) |
| Taking insulin | 1,205 (9.4%) |
| Smoker | 2,606 (20%) |
| Estimated glomerular filtration rate <30 ml/min/1.73 m 2 | |
| Without hemodialysis | 630 (4.9%) |
| With hemodialysis | 682 (5.3%) |
| Acute coronary syndrome | 3,179 (25%) |
| ST-elevation myocardial infarction | 1,253 (9.8%) |
| Non–ST-elevation myocardial infarction | 307 (2.4%) |
| Unstable angina | 1,619 (13%) |
| Previous myocardial infarction | 3,488 (27%) |
| Previous stroke | 1,218 (9.5%) |
| Peripheral vascular disease | 1,524 (12%) |
| Previous heart failure | 1,793 (14%) |
| Previous percutaneous coronary intervention | 5,954 (46%) |
| Previous coronary artery bypass grafting | 919 (7.2%) |
| Multivessel disease | 7,054 (55%) |
| Target of unprotected left main coronary artery | 582 (4.5%) |
| Ejection fraction (%) | 57.8 ± 13.4 |
| Number of coronary vessels treated | 1.32 ± 0.56 |
| Multivessel coronary stenting | 2,430 (19%) |
| Number of coronary lesions treated | 1.38 ± 0.78 |
| Lesion characteristics | |
| Number of lesions | 19,675 |
| Coronary lesion location | |
| Left anterior descending coronary artery | 7,841 (40%) |
| Ostial left anterior descending coronary artery | 547 (2.8%) |
| Left circumflex coronary artery | 4,354 (22%) |
| Ostial left circumflex coronary artery | 138 (7.0%) |
| Right coronary artery | 6,625 (34%) |
| Ostial right coronary artery | 425 (2.2%) |
| Left main coronary artery | 686 (3.5%) |
| Saphenous vein graft | 144 (0.7%) |
| ST-elevation myocardial infarction culprit lesion | 1,321 (6.7%) |
| In-stent restenosis | 2,198 (11%) |
| Long-term total occlusion | 1,796 (9.1%) |
| Severe calcification | 1,789 (9.1%) |
| Bifurcation lesion | 3,716 (19%) |
| Side branch stenting | 757 (3.8%) |
| Lesion length, (mm) | 18.9 ± 12.4 |
| Lesion length ≥30 mm | 2,833 (15%) |
| Preprocedure reference diameter (mm) | 2.75 ± 0.56 |
| Preprocedure reference diameter <2.5 mm | 5,748 (30%) |
| American College of Cardiology/American Heart Association type B2/C | 13,390 (68%) |
| Use of intravascular ultrasound | 8,214 (42%) |
| Direct stenting | 4,525 (23%) |
| After dilation | 8,195 (44%) |
| Maximum inflation pressure (atm) | 17.8 ± 3.4 |
| Number of stents used | 1.29 ± 0.57 |
| Length of stents used (mm) | 28.9 ± 15.7 |
| Minimal stent size (mm) | 2.89 ± 0.39 |
Clinical features were significantly different between SES-treated and BMS-treated lesions ( Table 2 ). Lesions treated with SESs included significantly more complex lesion characteristics such as long-term total occlusion, ostial left anterior descending coronary artery lesion, in-stent restenosis, small artery, and long lesion. Lesions treated with BMSs included more emergency procedures and ST-elevation myocardial infarction culprit lesions.
| Variables | SES | BMS | p Value |
|---|---|---|---|
| Number of lesions | 17,050 | 1,259 | |
| Patient factor | |||
| Age ≥80 years | 2,294 (13%) | 215 (17%) | 0.0005 |
| Men | 12,797 (75%) | 948 (75%) | 0.85 |
| Body mass index <25 kg/m 2 | 10,998 (65%) | 829 (66%) | 0.32 |
| Multivessel coronary disease | 10,703 (63%) | 1,121 (89%) | <0.0001 |
| Ejection fraction ≤40% | 1,773 (12%) | 129 (13%) | 0.2 |
| Estimated glomerular filtration rate <30 ml/min/1.73 m 2 and/or hemodialysis | 1,837 (11%) | 114 (9%) | 0.051 |
| Hemodialysis | 922 (5.4%) | 47 (3.7%) | 0.072 |
| Hypertension | 12,774 (75%) | 908 (72%) | 0.029 |
| Smoker | 3,448 (20%) | 368 (29%) | <0.0001 |
| Diabetes mellitus | 7,259 (43%) | 540 (43%) | 0.83 |
| Taking insulin | 1,710 (10%) | 98 (7.8%) | 0.0078 |
| Lesion factor | |||
| Emergency procedure | 1,633 (9.6%) | 619 (49%) | <0.0001 |
| ST-elevation myocardial infarction culprit lesion | 817 (4.8%) | 438 (35%) | <0.0001 |
| Use of intravascular ultrasound | 7,569 (45%) | 376 (31%) | <0.0001 |
| Unprotected left main coronary artery | 480 (2.8%) | 47 (3.7%) | 0.071 |
| Long-term total coronary occlusion | 1,469 (8.6%) | 53 (4.2%) | <0.0001 |
| Ostial left anterior descending coronary artery | 482 (2.8%) | 19 (1.5%) | 0.0027 |
| Ostial left circumflex coronary artery | 120 (0.7%) | 5 (0.4%) | 0.17 |
| Ostial right coronary artery | 397 (2.3%) | 13 (1.0%) | 0.0009 |
| In-stent restenosis | 2,036 (12%) | 16 (1.3%) | <0.0001 |
| Severe calcification | 1,499 (8.8%) | 91 (7.2%) | 0.051 |
| Vessel size <2.5 mm | 4,841 (29%) | 290 (25%) | 0.0099 |
| Lesion length ≥30 mm | 2,643 (15%) | 93 (8.3%) | <0.0001 |
| American College of Cardiology/American Heart Association type B2/C | 11,150 (68%) | 878 (73%) | <0.0001 |
| Bifurcation | 3,289 (19%) | 129 (10%) | <0.0001 |
| 2 stents for bifurcation | 578 (3.4%) | 22 (1.8%) | 0.0006 |
Incidence of TLR was compared between 17,050 SES-treated lesions and 1,259 BMS-treated lesions. Cumulative incidence of TLR during the overall 3 years of follow-up was significantly lower in SES-treated lesions compared to BMS-treated lesions as shown in Figure 1 (10.0% vs 15.5%, p <0.0001). TLR rate difference was most marked during the first year of stent implantation, whereas incidence of late TLR was significantly higher in SES-treated than in BMS-treated lesions (4.5% vs 1.4% from 1 years to 3 years, p = 0.0007; Figure 1 , Table 3 ). Late TLR procedures were shown to occur constantly up to ≥3 years after SES implantation. Of 449 late TLR procedures excluding TLR for stent thrombosis, only 11 procedures (2.4%) were performed in the setting of acute myocardial infarction.
| Early TLR | Late TLR | ||
|---|---|---|---|
| At 1 Year | At 2 Years | At 3 Years | |
| Sirolimus-eluting stent | |||
| Incidence of target lesion revascularization | 5.7% | 2.6% | 4.5% |
| Related to stent thrombosis | 0.35% | 0.14% | 0.38% |
| Not related to stent thrombosis | 5.3% | 2.4% | 4.2% |
| Bare metal stent | |||
| Incidence of target lesion revascularization | 14.3% | 1.4% | 1.4% |
| Related to stent thrombosis | 0.52% | 0% | 0% |
| Not related to stent thrombosis | 13.7% | 1.4% | 1.4% |
Cumulative incidences of definite stent thrombosis on a patient basis were 0.36% at 30 days, 0.61% at 1 year, and 1.2% at 3 years. Reflecting this low incidence of stent thrombosis, incidence of TLR for stent thrombosis was low (0.35% at 1 year and 0.38% from 1 year to 3 years after SES implantation), although there was no late TLR for stent thrombosis among BMS-treated lesions ( Table 3 ). Therefore, even after exclusion of TLR for stent thrombosis, incidence of late TLR was significantly higher in SES-treated lesions compared to BMS-treated lesions (4.2% vs 1.4% at 3 years, respectively, p = 0.0018).
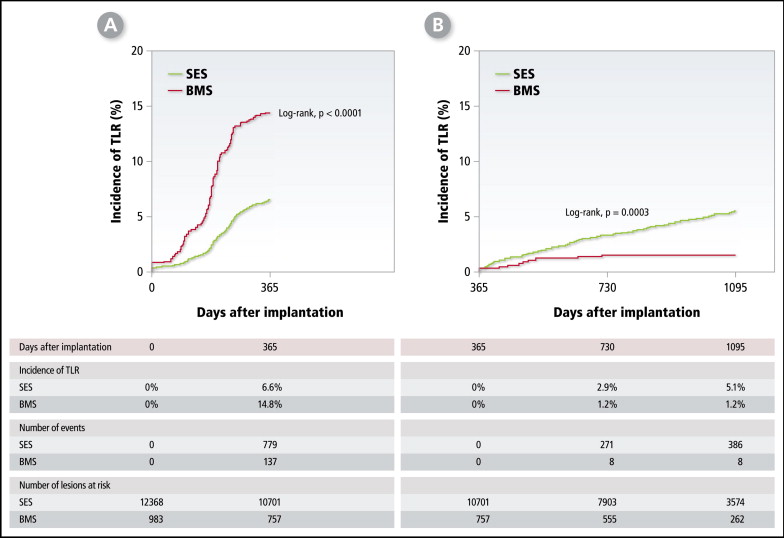
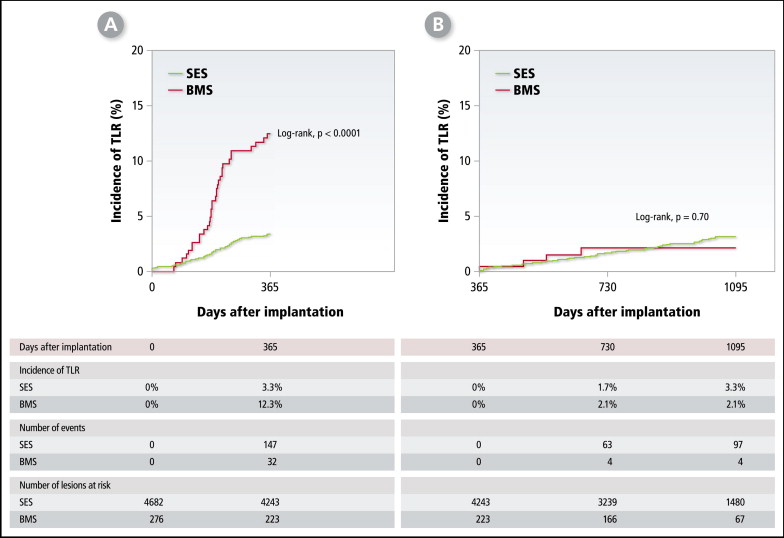
As an exploratory analysis, incidences of early and late TLR in SES- and BMS-treated lesions were compared according to complexity of the lesions (i.e., on-label and off-label indications; Figures 2 and 3 ). On-label indication lesions accounted for 27% (4,682 lesions) of SES-treated lesions and for 22% (276 lesions) of BMS-treated lesions. Incidence of early TLR at 1 year was significantly lower in SES-treated lesions compared to BMS-treated lesions for on- and off-label indications ( Figures 2 and 3 ). Incidence of late TLR beyond 1 year was significantly higher in SES-treated lesions than in BMS-treated lesions with off-label indication but not with on-label indication ( Figures 2 and 3 ).
Risk factors of early TLR after SES implantation were evaluated by univariate and multivariable analyses ( Table 4 ). Lesions included in analysis for early TLR were 926 lesions with TLR events within the first year and 14,844 lesions that completed 1-year follow-up without TLR events. The 25 potential variables listed in Table 4 were used for univariate analysis of risk factors for early TLR. Univariate analysis showed 8 patient-related and 9 lesion-related factors with a p value <0.05. The multivariable model using these 17 factors identified 10 independent risk factors of early TLR (4 patient-related and 6 lesion-related factors) including hemodialysis, diabetes, male gender, body mass index <25 kg/m 2 , 2 stents for bifurcation, ostial right coronary artery lesion, lesion length ≥30 mm, in-stent restenosis, severe calcification, and lesions classified as American College of Cardiology/American Heart Association type B2 or C.
| Variables | Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|---|
| Incidence of TLR (%) | OR | p Value | OR | 95% CI | p Value | ||
| Yes | No | ||||||
| Patient factor | |||||||
| Age ≥80 years | 4.9 | 6.0 | 0.81 | 0.048 | 0.92 | 0.71–1.17 | 0.48 |
| Men | 6.1 | 5.1 | 1.22 | 0.012 | 1.25 | 1.04–1.51 | 0.020 |
| Body mass index <25 kg/m 2 | 6.3 | 5.2 | 1.20 | 0.0081 | 1.20 | 1.02–1.41 | 0.029 |
| Multivessel coronary disease | 6.4 | 5.0 | 1.29 | 0.0002 | 1.70 | 0.99–1.38 | 0.062 |
| Ejection fraction ≤40% | 7.7 | 5.5 | 1.40 | 0.0004 | 1.16 | 0.93–1.43 | 0.19 |
| Estimated glomerular filtration rate <30 ml/min/1.73 m 2 and/or hemodialysis | 13.3 | 5.1 | 2.59 | <0.0001 | 1.07 | 0.74–1.53 | 0.73 |
| Hemodialysis | 20.1 | 5.2 | 3.89 | <0.0001 | 3.01 | 1.99–4.54 | <0.0001 |
| Hypertension | 5.9 | 5.7 | 1.03 | 0.66 | |||
| Smoker | 5.5 | 6.0 | 0.92 | 0.29 | |||
| Diabetes mellitus | 7.6 | 4.6 | 1.64 | <0.0001 | 1.41 | 1.21–1.65 | <0.0001 |
| Lesion factor | |||||||
| Emergency procedure | 6.6 | 5.8 | 1.15 | 0.19 | |||
| ST-elevation myocardial infarction culprit lesion | 5.9 | 5.9 | 1.01 | 0.97 | |||
| Use of intravascular ultrasound | 6.0 | 5.8 | 1.02 | 0.74 | |||
| Unprotected left main coronary artery | 10.4 | 5.8 | 1.81 | <0.0001 | 1.19 | 0.80–1.79 | 0.39 |
| Long-term total coronary occlusion | 8.4 | 5.6 | 1.50 | <0.0001 | 1.15 | 0.90–1.46 | 0.27 |
| Ostial left anterior descending coronary artery | 6.5 | 5.9 | 1.11 | 0.56 | |||
| Ostial left circumflex coronary artery | 14.6 | 5.8 | 2.50 | 0.0001 | 1.67 | 0.88–3.18 | 0.12 |
| Ostial right coronary artery | 17.9 | 5.6 | 3.20 | <0.0001 | 2.82 | 2.03–3.93 | <0.0001 |
| In-stent restenosis | 9.1 | 5.4 | 1.67 | <0.0001 | 1.75 | 1.44–2.14 | <0.0001 |
| Severe calcification | 12.7 | 5.2 | 2.43 | <0.0001 | 1.73 | 1.39–2.14 | <0.0001 |
| Vessel size <2.5 mm | 6.5 | 5.7 | 1.15 | 0.079 | |||
| Lesion length ≥30 mm | 11.0 | 5.0 | 2.18 | <0.0001 | 2.01 | 1.68–2.41 | <0.0001 |
| American College of Cardiology/American Heart Association type B2/C | 7.2 | 3.3 | 2.20 | <0.0001 | 1.51 | 1.24–1.85 | <0.0001 |
| 2 stents for bifurcation | 16.5 | 5.5 | 3.00 | <0.0001 | 3.30 | 2.47–4.40 | <0.0001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


