In this study, the clinical and implantable cardioverter-defibrillator (ICD)–related follow-up of patients with catecholaminergic polymorphic ventricular tachycardia (CPVT) with homogenous missense mutations in CASQ2 was summarized. Patients were followed in a pediatric cardiology clinic and an ICD clinic. All patients were treated with high-dose β blockers. ICDs were recommended for patients who remained symptomatic despite medical treatment. Twenty-seven patients were followed for 1 to 15 years (median 9). Twenty patients (74%) were symptomatic at diagnosis; 13 (65%) remained symptomatic after treatment with high-dose β blockers and thus were advised to receive ICDs. Eight of these patients refused ICDs, and eventually 6 (75%) died suddenly. Four of the 5 patients who received ICDs had ventricular tachycardia storms treated but not terminated by recurrent ICD shocks. These ventricular tachycardia storms (2 episodes in 2 patients and 1 episode in 2 patient) terminated spontaneously after finishing the programmed ICD shocks, without degeneration to ventricular fibrillation. None of the patients who received ICDs died. In conclusion, patients with CASQ2-associated CPVT should be recommended to receive ICDs to prevent sudden death when medical therapy is not effective. These patients may have recurrent ventricular tachycardia storms treated but not terminated by recurrent ICD shocks, without degeneration to ventricular fibrillation.
Although several mutations of 2 different genes have been related to catecholaminergic polymorphic ventricular tachycardia (CPVT), the exact genotype-phenotype relation remains far from settled. Patients are treated mainly with high-dose β blockers. Implantable cardioverter-defibrillators (ICD) are recommended for patients who remain symptomatic despite medical treatment. During follow-up, some of these patients experience appropriate and inappropriate shocks. The aim of this study was to summarize the clinical and ICD-related follow-up of a relatively large group of Bedouin patients with CPVT from Israel with missense mutations in CASQ2, described previously.
Methods
A highly inbred Bedouin tribe in northern Israel (about 2,500 subjects) were studied after a history of 9 cases of sudden death and a few cases of “familial epilepsy” in the past decade. Genetic workup from 1998 to 2001 mapped the disease to chromosome 1p13–21. A missense mutation in a highly conserved region of CASQ2 was found to be associated with autosomal recessive CPVT in this population. The subjects who were found to have homogenous mutations (homozygous for CASQ2-D307H mutation) were followed by a pediatric cardiologist and an electrophysiologist. All patients were treated with high-dose β blockers. The maximum doses of β blocker were determined clinically and by exercise test results. Dual-chamber ICD implantation was recommended for patients who had symptoms despite optimal therapy. Patients who received ICDs were followed by the ICD clinic routinely every 3 months and when necessary for analyzing arrhythmias and therapies. Antitachycardia pacing and shocks were considered appropriate if the triggering rhythm was determined to be ventricular fibrillation (VF) or ventricular tachycardia (VT). Appropriate ICD therapy in this analysis refers to ICD therapy that was triggered for a single rhythm event, regardless of the total number of actual shocks that were required to satisfy the criteria for termination of tachycardia. Three or more appropriate ICD shocks within 24 hours was considered a VT storm.
Results
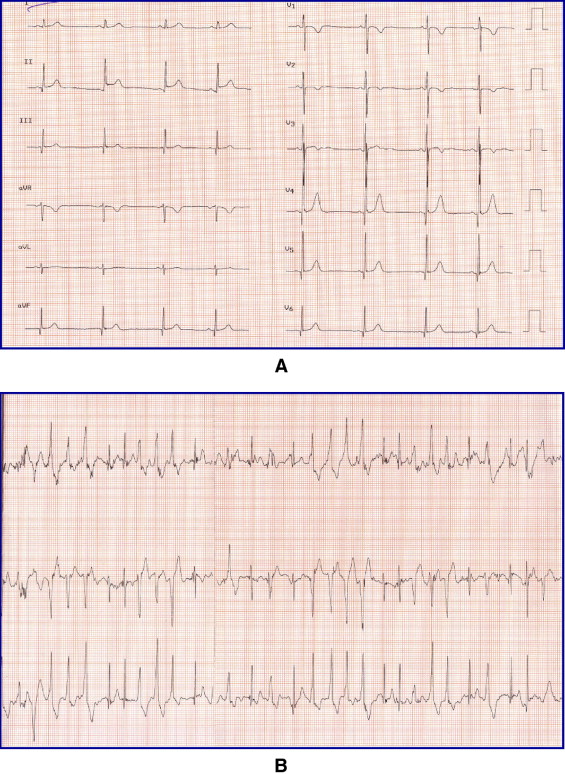
Twenty-seven patients (18 female, 9 male) from 12 families were diagnosed by genetic analysis (homozygous for CASQ2-D307H mutation). The age at genetic diagnosis ranged from 0 to 22 years (mean 8 ± 7). The patients were followed for 1 to 15 years (median 9). Twenty patients (74%) were symptomatic at diagnosis, of whom 13 (65%) had syncope and 7 (35%) had seizures. The age at first symptoms ranged from 2 to 10 years (mean 6 ± 4). These patients had relative bradycardia at rest with heart rates of 47 to 93 beats/min (mean 66 ± 14) and normal corrected QT intervals (0.36 to 0.43 seconds according to Bazett’s formula; Figure 1 ). All had normal hearts by echocardiography, and 10 patients had normal findings on cardiac magnetic resonance imaging. All patients had positive stress test results (treadmill or isoproterenol) for ventricular arrhythmia ( Figure 1 ). All patients were treated with high-dose β blockers, 26 with propranolol and 1 with atenolol.
All 7 patients (26%) who were asymptomatic continued to be asymptomatic on β blockers. Seven of the symptomatic patients (35%) became asymptomatic with β-blocker treatment. These patients (asymptomatic patients at baseline or after treatment) did not receive ICDs except for 1 patient who received an ICD according to the request of his parents. The remaining 13 symptomatic patients (65%) continued to experience symptoms (presyncope or syncope) despite high-dose β blockers. ICD implantation was recommended for all of them; 5 patients received ICDs and 8 patients refused. Defibrillation thresholds were checked for all patients with ICDs at implantation and were found to be normal, and VF was terminated by ICD shocks with an average output of 15 ± 3 J.
At the beginning of our experience, 3 patients received antibradycardia pacing for proposed long-QT diagnosis before the definitive diagnosis of CPVT. All these patients received ICDs later because of continuing symptoms (these patients are included among the 5 patients who received ICDs because of symptoms). Eventually, 6 patients received ICDs, 5 for symptoms and 1 according to family request.
Four of the 5 patients who received ICDs because of symptoms had episodes of VT. Episodes of VT storms were observed in all of these patients: 2 episodes in 2 patients and 1 episode in 2 patients. However, the episodes of VT storm in these patients were treated by repeated ICD shocks but did not terminate. The episodes terminated spontaneously later after the ICD therapies were stopped, without degeneration to VF ( Figure 2 ) . In 2 of these patients, episodes of VT that terminated after 1 shock were also observed. The patient who received an ICD according to the request of his family was free of arrhythmias during follow-up.
None of the asymptomatic patients at baseline or after treatment with high-dose β blockers died during follow-up (4 to 13 years after diagnosis, median 9 years; Figure 3 ) . All the symptomatic patients who received ICDs survived despite VT episodes during follow-up (9 to 16 years after diagnosis, median 12 years). Six of the 8 symptomatic patients who refused ICDs died suddenly despite treatment with high-dose β blockers and calcium antagonists during follow-up (1 to 10 years after diagnosis; median 7 years). The other 2 symptomatic patients who refused ICDs were alive 7 and 11 years after diagnosis.




