We evaluated the effects of myocardial perfusion after primary percutaneous coronary intervention (PCI) for acute myocardial infarction (AMI) on gender-based mortality rates. Research has demonstrated a gender-specific response of cardiomyocytes to ischemia and a potential increase in myocardial salvage in women compared with men. Myocardial blush grade (MBG), an angiographic surrogate of myocardial perfusion, is an independent predictor of early and late survival after AMI. Whether the incidence and prognosis of myocardial perfusion differs according to gender among patients with AMI undergoing PCI is unknown. MBG and short- and long-term mortality were evaluated in 1,301 patients (male = 935; female = 366) with AMI randomized to primary angioplasty ± abciximab versus stent ± abciximab. Following PCI, >96% of patients achieved final Thrombolysis In Myocardial Infarction 3 flow, of which MBG 2/3 was present in 58.3% of women versus 51.1% of men (p = 0.02). Worse MBG was an independent predictor of mortality in women at 30 days (7.4% for MBG 0/1 vs 2.4% for MBG 2/3, p = 0.04) and at 1-year (11.0% for MBG 0/1 vs 3.4% for MBG 2/3, p = 0.01); however, MBG was not associated with differences in mortality for men. In conclusion, impaired myocardial perfusion following PCI for AMI, indicated by worse MBG, is an independent predictor of early and late mortality in women but not in men. These findings imply an enhanced survival benefit from restoring myocardial perfusion for women compared with men during primary angioplasty and may have clinical implications for interventional strategies in women.
The aim of this study is to evaluate the incidence and implications of myocardial reperfusion, as assessed by myocardial blush grade (MBG), on gender-based short- and long-term mortality in patients with acute myocardial infarction (AMI) undergoing primary percutaneous coronary intervention (PCI).
Methods
Our study was a subset analysis of patients enrolled in the prospective, blinded, multicenter CADILLAC (Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications) trial, described previously. In brief, between December 1997 and December 1999, 2,082 patients presenting with AMI due to native coronary artery occlusion who presented within 12 hours of symptom onset were randomized at 76 international centers in a 2 × 2 factorial design to primary balloon angioplasty ± abciximab versus primary stenting ± abciximab. Pertinent exclusion criteria included cardiogenic shock, bleeding diatheses, renal insufficiency, and coronary anatomy not suitable for stent placement.
The primary end point was the occurrence of major adverse cardiovascular events, defined as the composite of death, reinfarction, ischemia-driven target vessel revascularization, and disabling stroke. Procedure success was defined as final residual stenosis <50%, final Thrombolysis In Myocardial Infarction (TIMI) 3 flow, and freedom from major adverse cardiovascular events within 7 days of the procedure. Follow-up data was collected for 1 year.
Myocardial blush was not prespecified during the initial angiographic analysis. A voluntary recall of angiographic films was performed to assess MBG, and 1,500 index angiograms (72%) were returned for reanalysis, of which 1,301 (87%) were technically suitable for MBG determination. All angiograms were analyzed by an independent angiographic core laboratory (the Cardiovascular Research Foundation, New York, New York).
Angiograms were considered technically adequate for blush analysis if (1) at least 1 view was present that isolated the myocardial infarct zone, (2) angiographic runs were of adequate duration to assess tissue-level perfusion (completed filling of the coronary venous system), and (3) there was complete arterial opacification with backflow of contrast into the aorta, indicating adequate contrast filling of the epicardial coronary artery without occlusive catheter wedging.
Myocardial blush was graded in the distribution of the target vessel based on the maximal densitometric degree of contrast opacification. MBG 0/1 indicated absent or minimal myocardial contrast opacification; MBG 2 indicated moderate contrast opacification, but less than in an ipsilateral or contralateral noninfarct artery; MBG 3 indicated normal myocardial blush or contrast opacification. When myocardial blush persisted, the so-called staining phenomenon, MBG 0 was assigned. As in previous studies, MBG 2 and 3 were grouped together for analysis.
Categorical data are presented as frequencies and were compared using the likelihood ratio chi-square test or Fisher’s exact test. Continuous variables are presented as median with interquartile ranges and were compared by 1-way analysis of variance or the Kruskal-Wallis test. Time-to-event data are summarized as actuarial estimates, displayed as Kaplan-Meier curves and compared with the log-rank test. Stepwise logistic regression analysis selecting baseline variables with an entry/stay criterion of p <0.10 was used to determine the independent predictors of normal myocardial blush after PCI. Cox proportional hazards regression was used to identify independent correlates of 1-year mortality. Variables entered into the model included age, gender, diabetes, hypertension, previous AMI or bypass surgery, Killip class, infarct-artery, triple-vessel disease, time to reperfusion (symptoms onset to first balloon inflation), baseline TIMI flow, final MBG, stent implantation, abciximab use, and body surface area.
Results
The study population of 1,301 patients consisted of 366 women and 935 men. Procedure success was achieved in >90% of cases. Baseline clinical demographics and procedure data are presented in Table 1 . Final TIMI 3 flow was present in the majority of patients (97.3% of women and 95.8% of men). Despite older age, increased frequencies of comorbidities, and longer delays to treatment, women demonstrated better myocardial perfusion at baseline (MBG 2/3) compared with men (13.3% vs 8.8%, p = 0.02) and after PCI (56.8% vs 49.2%, p = 0.02; Table 2 ).
| Variable | Women (n = 366) | Men (n = 935) | p Value |
|---|---|---|---|
| Age (yrs) | 67 (57–75) | 57 (49–66) | <0.0001 |
| Hypertension (history) | 59.8% | 43.4% | <0.0001 |
| Dyslipidemia (history) | 45.4% | 36.5% | 0.004 |
| Diabetes mellitus | 25.4% | 14.9% | <0.0001 |
| Current smoker | 36.1% | 47.1% | 0.0004 |
| Previous myocardial infarction | 7.7% | 16.6% | <0.0001 |
| Previous percutaneous coronary intervention | 6.3% | 13.3% | 0.0005 |
| Previous coronary artery bypass grafting | 1.6% | 2.6% | 0.38 |
| Multivessel coronary artery disease | 48.9% | 48.8% | 0.97 |
| Renal insufficiency (history) | 35.7% | 13.2% | <0.0001 |
| Body surface area (m 2 ) | 1.73 | 2.02 | <0.0001 |
| Time: symptoms onset to first balloon inflation (h) | 4.93 | 3.83 | <0.0001 |
| Infarct location | |||
| Anterior | 34.2% | 36.0% | 0.56 |
| Lateral | 13.9% | 19.0% | 0.04 |
| Inferior | 51.9% | 45.0% | 0.04 |
| Stent implanted | 56.6% | 56.5% | 1.0 |
| Abciximab use | 48.9% | 53.9% | 0.10 |
| Procedure success | 91.6% | 92.0% | 0.82 |
| Variable | Women (n = 366) | Men (n = 935) | p Value |
|---|---|---|---|
| Lesion length (mm) | 13.20 | 12.69 | 0.48 |
| Thrombus | 54.2% | 56.5% | 0.45 |
| Left ventricular ejection fraction (%) | 56.9 | 56.4 | 0.52 |
| Preprocedure TIMI | |||
| 0 | 58.7% | 61.8% | 0.34 |
| 1 | 7.4% | 7.5% | 0.96 |
| 2 | 9.3% | 10.0% | 0.79 |
| 3 | 24.6% | 20.8% | 0.13 |
| Final TIMI | |||
| 0 | 0.3% | 0.7% | 0.55 |
| 1 | 1.1% | 0.4% | 0.32 |
| 2 | 1.4% | 3.0% | 0.13 |
| 3 | 97.3% | 95.8% | 0.25 |
| Preprocedure MBG | |||
| 0/1 | 86.7% | 91.2% | 0.02 |
| 2/3 | 13.3% | 8.8% | 0.02 |
| Final MBG | |||
| 0/1 | 43.2% | 50.8% | 0.02 |
| 2/3 | 56.8% | 49.2% | 0.02 |
| Patients with Final TIMI 3 flow | Women (n = 355) | Men (n = 896) | |
| Preprocedure MBG | |||
| 0/1 | 86.3% | 90.8% | 0.03 |
| 2/3 | 13.7% | 9.2% | 0.03 |
| Final MBG | |||
| 0/1 | 41.7% | 48.9% | 0.02 |
| 2/3 | 58.3% | 51.1% | 0.02 |
Among patients with final TIMI 3 flow, anterior infarct location and greater delay to mechanical reperfusion were associated with worse final MBG in both men and women; a history of diabetes was also associated with final MBG 0/1 in women ( Table 3 ). Furthermore, time to reperfusion >6 hours was significantly associated with final MBG 0/1 regardless of gender ( Table 4 ). A history of smoking and inferior infarct location were associated with better final MBG.
| Variable | Women | p Value | Men | p Value | ||
|---|---|---|---|---|---|---|
| MBG 0/1 (n = 148) | MBG 2/3 (n = 207) | MBG 0/1 (n = 438) | MBG 2/3 (n = 458) | |||
| Mean age (yrs) | 67 | 67 | 0.8 | 58 | 57 | 0.6 |
| Hypertension (history) | 57.4% | 61.8% | 0.4 | 44.3% | 48.0% | 0.5 |
| Dyslipidemia (history) | 42.6% | 47.8% | 0.3 | 37.0% | 34.3% | 0.4 |
| Diabetes mellitus | 31.8% | 21.7% | 0.03 | 16.7% | 12.4% | 0.07 |
| Current smoker | 29.7% | 40.1% | 0.04 | 45.0% | 51.1% | 0.07 |
| Previous myocardial infarction | 6.8% | 8.7% | 0.5 | 16.9% | 16.6% | 0.9 |
| Previous percutaneous coronary intervention | 5.4% | 7.2% | 0.5 | 13.9% | 12.9% | 0.6 |
| Previous coronary artery bypass grafting | 0.7% | 2.4% | 0.2 | 1.8% | 3.3% | 0.2 |
| Multivessel coronary artery disease | 48.6% | 49.8% | 0.8 | 49.1% | 47.8% | 0.7 |
| Renal insufficiency | 35.3% | 35.9% | 0.9 | 13.1% | 12.6% | 0.8 |
| Body surface area (m 2 ) | 1.73 | 1.74 | 0.4 | 2.03 | 2.0 | 0.1 |
| Time symptoms onset to first balloon inflation (h) | 5.56 | 4.32 | <0.0001 | 4.05 | 3.67 | 0.009 |
| Infarct location | ||||||
| Anterior | 51.4% | 20.8% | <0.0001 | 49.1% | 34.5% | <0.0001 |
| Lateral | 16.9% | 14.0% | 0.5 | 20.3% | 18.6% | 0.5 |
| Inferior | 31.8% | 65.2% | <0.0001 | 30.6% | 60.0% | <0.0001 |
| Final Myocardial Blush Grade | Time from Symptoms Onset to First Balloon Inflation (h) | p Value | ||
|---|---|---|---|---|
| <3 (n = 310) | 3 to 6 (n = 565) | >6 (n = 334) | ||
| 0 | 7.1% | 11.2% | 12.9% | 0.0492 |
| 1 | 35.8% | 33.8% | 41.9% | 0.0484 |
| 2 | 36.5% | 37.0% | 29.6% | 0.0644 |
| 3 | 20.6% | 18.1% | 15.6% | 0.2462 |
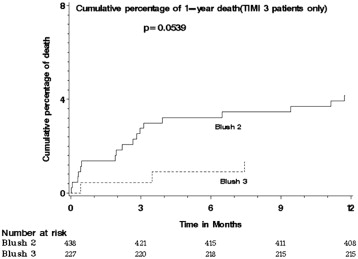
Women demonstrated increased overall mortality rates at 30 days (5.5% vs 1.0%, p <0.0001), and at 1 year (7.5% vs 3.6%, p = 0.002). Among patients with final TIMI 3 flow, unadjusted mortality was higher in women at 30 days (4.5% vs 1.1%, p = 0.0004), and at 1 year (6.7% vs 3.3%, p = 0.01). Worse final MBG after PCI was also associated with increased 30-day (3.2% for MBG 0/1 vs 1.1% for MBG 2/3, p = 0.01) and 1 year (5.6% vs 3.2%, p = 0.04) mortality rates. An increased cumulative mortality rate at 1 year was even found in patients with MBG 2 versus MBG 3 ( Figure 1 ).
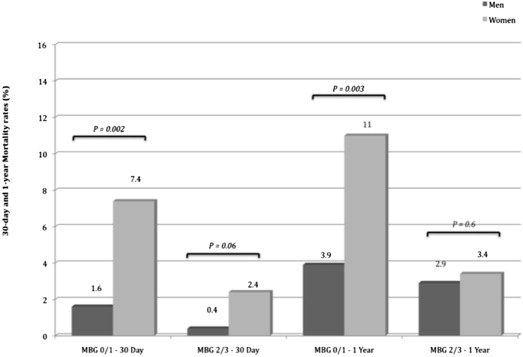
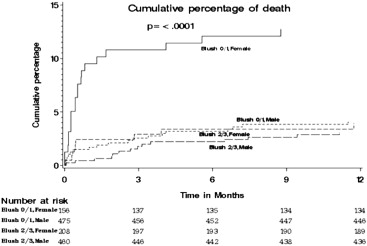
When myocardial reperfusion was not achieved (MBG 0/1) in patients with final TIMI 3 flow, women had higher 30-day and 1-year mortality rates compared with men. In contrast, when myocardial reperfusion was achieved (MBG 2/3), women and men had similar 30-day and 1-year mortality rates ( Figures 2 and 3 ).
Cox proportional hazards regression identified final MBG as an independent predictor of death at 1 year for women only (odds ratio: 0.17, 95% confidence interval: 0.05 to 0.53, p = 0.0025). Other independent predictors of 1-year mortality for women included body surface area and history of hypertension. For men, acute infarction of the left anterior descending artery and triple vessel disease were independent predictors. Age and creatinine were independent predictors for both genders ( Table 5 ).



