Chapter 38
Implantable Cardioverter-Defibrillators
1. What are the components of an implantable cardioverter-defibrillator (ICD) system?
ICDs are composed of a pulse generator (typically implanted in the left pectoral region) and one or more intracardiac leads. Typically the right ventricular (RV) lead contains two distal electrodes (tip and ring) that are used to sense local electrical ventricular signals and to pace if necessary. This lead also contains one or two defibrillation coils (one sits in the RV and the other in the superior vena cava) specifically designed to deliver high voltages. Additional leads may include an atrial lead (for pacing, sensing, and arrhythmia discrimination) or a left ventricular (LV) lead for cardiac resynchronization (Fig. 38-1). All transvenous defibrillators are also capable of pacemaker functions.
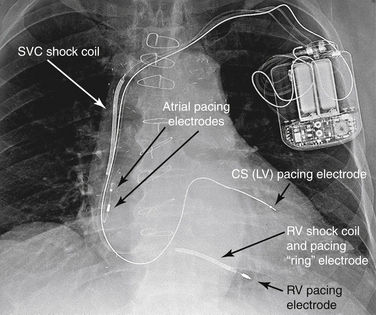
Figure 38-1 A radiograph of a patient with an implantable cardioverter-defibrillator (ICD). With this ICD, shock coils are present in both the right ventricle (RV) and the superior vena cava (SVC). There is also a coronary sinus (CS) lead present for biventricular pacing. (From Miller R, Eriksson L, Fleisher L, et al: Miller’s anesthesia, ed 7, Philadelphia, 2009, Churchill Livingstone.) LV, left ventricle.
2. How does an ICD deliver shocking energy?
ICDs use lithium-vanadium batteries that are reliable energy sources with predictable discharge curves. An ICD is able to deliver a charge larger than its battery voltage because of a system of internal capacitors. These hold a charge and then release it all at once when it is needed. Shocking energy travels around a circular circuit, usually formed between the defibrillator lead coils and the device titanium-housed can.
3. How does the ICD detect and define a rhythm?
4. How does ICD therapy improve survival?
5. What are the key clinical trials that evaluated the benefit of ICD for primary prevention?
Clinical trials have evaluated the risks and benefits of ICDs in prevention of sudden death and have improved survival in multiple patient populations, including those with prior myocardial infarction (MI) and heart failure caused by either coronary artery disease or nonischemic dilated cardiomyopathy (DCM). Table 38-1 summarizes the important trials that evaluated the mortality benefit of ICDs for primary prevention.
TABLE 38-1
TRIALS THAT EVALUATED THE BENEFIT OF IMPLANTABLE CARDIOVERTER-DEFIBRILLATORS FOR PRIMARY PREVENTION OF SUDDEN CARDIAC DEATH
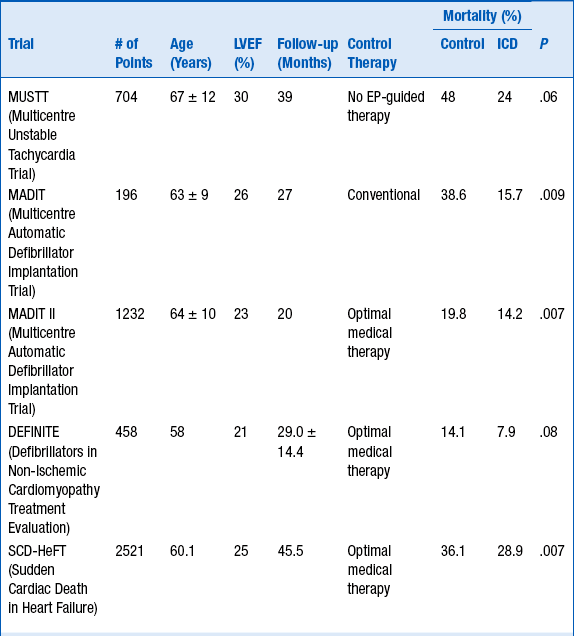
EP, Electrophysiologic; ICD, implantable cardioverter-defibrillator.
6. What are the current class I indications for ICD implantation for primary prevention of SCD?




