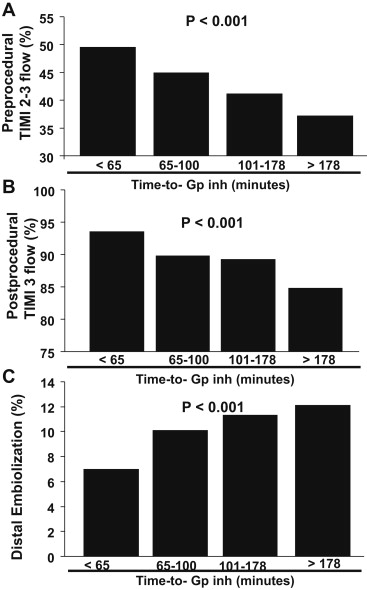
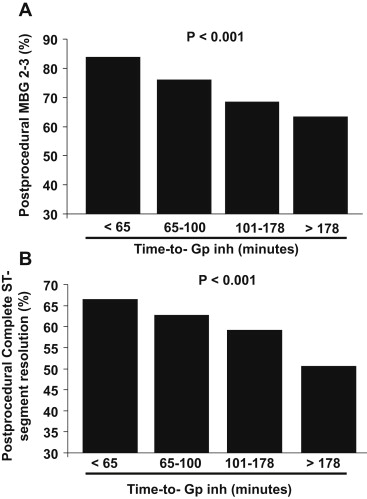
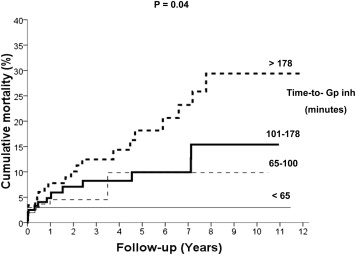
Contrasting data have been so far reported on facilitation with glycoprotein IIb-IIIa inhibitors (GpIIbIIIa) in patients who underwent primary percutaneous coronary intervention. However, it has been demonstrated a time-dependent composition of coronary thrombus in ST-segment elevation myocardial infarction, with more platelets in the first hours. Subsequently, the benefits of early administration of GpIIbIIIa may be affected by the time from symptoms onset to GpIIbIIIa, that therefore is the aim of this study. Our population is represented by 814 patients who underwent GpIIbIIIa facilitated primary angioplasty included in the Early glycoprotein IIb-IIIa inhibitors in primary angioplasty database. Patients were divided according to quartiles of time from symptom onset to GpIIbIIIa administration (≤65 minutes; 65 to 100 minutes; 101 to 178 minutes; and >178 minutes). Myocardial perfusion was evaluated by myocardial blush grade and ST-segment resolution. Time from symptoms onset to GpIIbIIIa was linearly associated with hypertension, diabetes, hypercholesterolemia, and previous myocardial infarction but inversely associated with smoking. Abciximab was more often administrated later from symptoms onset. Time from symptoms onset to GpIIbIIIa was significantly associated with the rate of preprocedural recanalization (thrombolysis in myocardial infarction [TIMI] 2 to 3; p <0.001), postprocedural TIMI 3 flow (p <0.001), the rate of complete ST-segment resolution (p <0.001), and the rate of myocardial blush grade 2 to 3 (p <0.001) and inversely associated with the occurrence of distal embolization (p <0.001). Follow-up data were collected at a median (twenty-fifth to seventy-fifth) of 360 (30 to 1,095) days. A total of 52 patients had died. Time to GpIIbIIIa had a significant impact on mortality (hazard ratio [95% confidence interval] 1.46 [1.11 to 1.92], p = 0.007) that was confirmed after correction for baseline confounding factors (adjusted hazard ratio [95% confidence interval] 1.41 [1.02 to 2.21], p = 0.042). In conclusion, this study showed that in patients who underwent primary angioplasty with upstream GpIIbIIIa, time from symptoms onset to GpIIbIIIa strongly impacts on preprocedural recanalization, distal embolization, myocardial perfusion, and long-term survival.
Mechanical reperfusion has significantly improved clinical outcome in ST-segment elevation myocardial infarction (STEMI) patients, and large attention has been paid to optimization of adjunctive antithrombotic therapies. However, ischemia time is a major determinant of mortality and timely application of mechanical reperfusion cannot be guaranteed to all patients. Therefore, great attention has been focused in the last decade on facilitation with glycoprotein IIb-IIIa inhibitors (GpIIbIIIa), fibrinolysis, or their combination. Contrasting data have been so far reported, with significant benefits in mortality observed with early GpIIbIIIa administration in the Early glycoprotein IIb-IIIa inhibitors in primary angioplasty (EGYPT) cooperation and in registries, whereas no benefits were observed in the Facilitated Intervention with Enhanced Reperfusion Speed to Stop Events (FINESSE) trial that was prematurely stopped because of slow recruitment. A factor that can certainly contribute to explain the difference in outcome is the longer delay to treatments as compared to previous experiences. In fact, it has been demonstrated a time-dependent composition of coronary thrombus in the setting of STEMI, with larger prevalence of platelet in the first hours and larger prevalence of fibrin in the later hours. Subsequently, the benefits of early upstream administration of GpIIbIIIa are expected to be affected by the time of administration from symptom onset that is, therefore, the aim of the present study.
Methods
Our population is represented by STEMI patients treated by primary angioplasty included in the EGYPT cooperation. All patients were admitted within 12 hours from symptom onset. All patients received aspirin (500 mg intravenously) and heparin (10,000 IU intravenously). All patients received upfront GpIIbIIIa (abciximab: bolus of 0.25 μg/kg and 12-hour infusion at 0.125 μg/kg/min; tirofiban: bolus of 10 μg/kg and 24-hour infusion at 0.15 μg/kg/min; eptifibatide: bolus of 180 μg/kg × 2, followed by 12- to 24-hour infusion at 2 μg/kg/min). In all cases, the bolus of clopidogrel (300 mg) was administrated after the procedure. All patients were on double oral antiplatelet therapy (aspirin and clopidogrel) for at least 4 weeks after stent implantation. Thereafter, aspirin or clopidogrel (in case of aspirin side effects) were continued as monotherapy.
Angiograms and electrocardiograms were not analyzed by a central core laboratory, but data were provided by each principal investigator. Analysis of angiograms was based on standard definitions. Angiographic myocardial perfusion was evaluated by myocardial blush grade (MBG). Distal embolization was defined as an abrupt “cutoff” in the main vessel or 1 of the coronary branches of the infarct-related artery (IRA), distal to the angioplasty site. Although ST-segment analysis was performed according to the prespecified criteria of each trial, data were provided according to uniform thresholds (<30%: no resolution; 30% to 70%: partial resolution; >70%: complete resolution). Infarct size was estimated using peak creatine kinase and creatine kinase-myocardial band.
Clinical outcome was assessed at follow-up by telephone interview or at medical visit. Clinical end point was overall mortality.
Statistical analysis was performed with the SPSS 17.0 statistical package. Continuous data were expressed as mean ± SD and categorical data as percentage. The analysis of variance test was used for continuous variables. The chi-square test or the Fisher’s exact test was used for categorical variables. Patients were divided according to quartiles of time from symptoms onset to GpIIbIIIa administration. Multiple logistic regression analysis was used to evaluate the impact of time from symptoms onset to GpIIbIIIa administration on impaired myocardial perfusion after adjustment for significant (p <0.05) confounding baseline characteristics. The difference in event rates between groups during the follow-up period was assessed by the Kaplan–Meier method using the log-rank test. Cox regression analysis was used to evaluate the impact of time from symptoms onset to GpIIbIIIa administration on survival after adjustment for significant (p <0.05) baseline confounding characteristics.
Results
Our population is represented by a total of 814 STEMI patients who underwent primary angioplasty with early GpIIbIIIa inhibitors. Patient’s characteristics according to quartiles of time from symptoms onset to drug administration (≤65 minutes; 65 to 100 minutes; 101 to 178 minutes; and >178 minutes) are summarized in Table 1 . Time from symptoms onset to drug administration was linearly associated with hypertension, diabetes, hypercholesterolemia, and previous myocardial infarction but inversely associated with the prevalence of smoking. Abciximab was more often administrated in later from symptoms onset. Time from symptoms onset to drug administration was significantly associated with the rate of preprocedural recanalization (thrombolysis in myocardial infarction [TIMI] 2 to 3; p <0.001, Figure 1 ), postprocedural TIMI 3 flow (p <0.001, Figure 1 ), the rate of complete ST-segment resolution (p <0.001, Figure 2 ), and the rate of MBG 2 to 3 (p <0.001, Figure 2 ) and inversely associated with the occurrence of distal embolization (p <0.001, Figure 1 ). Follow-up data were collected at a median (twenty-fifth to seventy-fifth) of 360 (30 to 1,095) days. Nine patients were lost to follow-up. A total of 52 patients had died. As shown in Figure 3 , the time to GpIIbIIIa administration had a significant impact on mortality (hazard ratio [95% confidence interval] 1.46 [1.11 to 1.92], p = 0.007), that was confirmed after correction for baseline confounding factors (age, gender, diabetes, smoking, hypertension, hypercholesterolemia, previous myocardial infarction, symptom onset to balloon >3 hours, Killip class I, abciximab; hazard ratio [95% confidence interval] 1.41 [1.02 to 2.21], p = 0.042).
| Variables | I Q (≤ 65 min) (n = 209) | II Q (65-100 min) (n = 202) | III Q (101-178 min) (n = 201) | IV Q (> 178 min) (n = 204) | p value (trend) |
|---|---|---|---|---|---|
| Age (years) | 61.4 ± 10.2 | 59.9 ± 11.4 | 59.6 ± 12.3 | 62.1 ± 12.4 | 0.65 |
| Age > 75 years | 11% | 11.9% | 11.4% | 17.2% | 0.21 |
| Women | 18.2% | 21.8% | 26.9% | 28.4% | 0.007 |
| Hypertension | 28.2% | 40.6% | 48.3% | 53.2% | <0.001 |
| Diabetes Mellitus | 10.5% | 16.3% | 15.4% | 22.5% | 0.002 |
| Smoker | 57.9% | 55.0% | 48.8% | 46.8% | 0.01 |
| Hypercholesterolemia | 28.7% | 29.7% | 37.3% | 47.1% | 0.001 |
| Previous MI | 5.7% | 6.9% | 8.5% | 11.3% | 0.033 |
| Anterior MI | 46.4% | 43.8% | 42.9% | 42.0% | 0.36 |
| Previous revascularization | 8.9% | 8.6% | 5.6% | 8.6% | 0.66 |
| Killip class > 1 | 5.9% | 10.1% | 12.4% | 15.1% | 0.004 |
| SOB time (minutes) | 172 ± 76 | 168 ± 79 | 207 ± 108 | 385 ± 268 | < 0.001 |
| Time from Gp IIb-IIIa to balloon inflation (minutes) | 131 ± 78 | 114 ± 84 | 110 ± 58 | 125 ± 163 | 0.35 |
| Angiographic and procedural variables | |||||
| Multivessel coronary disease | 59.4% | 51.4% | 54.9% | 63.2% | 0.24 |
| Coronary stenting | 83.3% | 83.3% | 87.3% | 86.0% | 0.3 |
| Type of Gp IIb-IIIa inhibitor | <0.001 | ||||
| Abciximab | 21.1% | 34.2% | 46.8% | 46.2% | |
| Tirofiban | 79.9% | 56.1% | 38.9% | 25.3% | |
| Eptifibatide | 0 | 9.7% | 15.3% | 29.5% |