and Mark C. Mammel2, 3
(1)
Division of Neonatal-Perinatal Medicine, C.S. Mott Children’s Hospital University of Michigan Health System, Ann Arbor, MI, USA
(2)
Neonatal Medicine, Children’s Hospitals and Clinics of Minnesota, St. Paul, St. Paul, MN, USA
(3)
University of Minnesota, Minneapolis, MN, USA
Keywords
Ventilator modesSynchronizationPatient-triggered ventilationPressure support ventilation3.1 Introduction
The interaction of mechanical ventilation and pulmonary mechanics is easier to appreciate by waveform monitoring. This enables the clinician to more objectively assess patient-ventilator synchrony and to adjust ventilator parameters to the individual needs of the baby based on both the underlying pathophysiology and the baby’s response to changes in ventilator settings.
3.2 Ventilator Modes
The ventilator mode refers to the sequencing or pattern of mechanical breaths delivered to the patient. There are essentially four modes of ventilation used in neonatal intensive care: intermittent mandatory ventilation (IMV), synchronized intermittent mandatory ventilation (SIMV), assist/control ventilation (A/C), and pressure support ventilation (PSV). Within these modes, different breath types or combination of breath types may be used without changing their definitions, and analysis of waveforms may be necessary to distinguish these.
3.2.1 IMV
IMV was the first interactive mode, allowing the patient to breathe fresh gas via the bias flow in the ventilator circuit supported by positive end-expiratory pressure (PEEP) circuit between mandatory breaths. During IMV, mechanical breaths are delivered to the patient at fixed intervals determined by setting a fixed respiratory rate. For example, if a clinician chooses a rate of 30 breaths/min, a mechanical breath will be delivered every 2 s, regardless of where the baby is in his or her own spontaneous cycle. Thus, asynchrony is a major drawback, because the baby may be trying to exhale against incoming inspiratory pressure, resulting in a small tidal volume (Vt), or to inhale with incoming positive pressure, resulting in a larger Vt. Asynchrony can lead to inefficient gas exchange, increase the risk of air leak, or require more sedation (prolonging the time on mechanical ventilation); irregularities in cerebral blood flow velocity and increased intraventricular hemorrhage have also been described.
Figure 3.1 displays flow and pressure volume waveforms during IMV. The ventilator rate has been set to deliver 30 breaths/min. Note that a mechanical breath is regularly delivered every 2 s. In between the mechanical breaths, the baby may breathe spontaneously, but these breaths are supported only by the applied PEEP.


Figure 3.1
Flow and pressure waveforms during IMV (a, schematic; b, actual). Mechanical breaths are provided every 2 s; in between, the patient may breathe spontaneously, supported only by PEEP
Figure 3.2 represents the effects of asynchrony. Variability in Vt delivery can be seen, even when the peak inspiratory pressure (PIP) is held constant. Thus when the baby is breathing with the ventilator, the Vt is higher than when the baby is breathing against the ventilator.
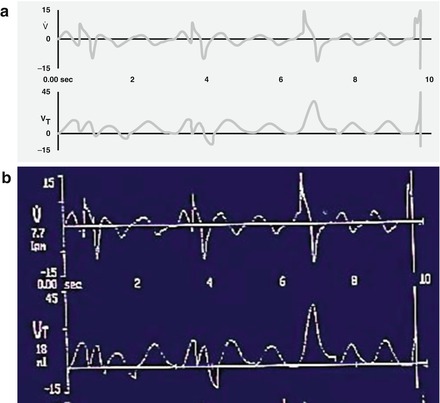
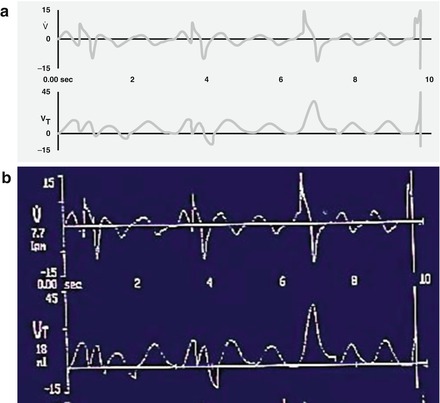
Figure 3.2
Dyssynchronous breathing during IMV (a, schematic; b, actual). The flow and volume waveforms demonstrate variability in delivered volume. The large volume breath occurred when the baby and the ventilator randomly synchronized
3.2.1.1 Patient-Triggered Ventilation
Patient-triggered ventilation (PTV) refers to modes of ventilation in which the patient’s own spontaneous effort may be used to trigger the initiation of a mechanical breath that is better synchronized than an IMV breath. Some measure of spontaneous breathing is used as a marker of patient effort. In newborns this is most commonly a change in airway flow or pressure and, more recently, diaphragmatic activity. The assist sensitivity is an adjustable trigger. It should be set low enough to enable the baby to easily exceed it, but not too low that leaks or non-respiratory flow changes induce auto-cycling (see Fig. 2.18). PTV has become more widespread since improvements in microprocessor and sensor technology have reduced trigger delay (system response time). This is the interval between reaching the assist sensitivity threshold and the rise in airway pressure at the proximal airway.
3.2.2 SIMV
SIMV was developed to help reduce some of the asynchrony that plagues IMV. A trigger signal is used initiate a mechanical breath in close temporal proximity to a spontaneous breath. As with IMV, the clinician selects the mechanical ventilator rate, but the ventilator may not cycle at exactly this interval. There is a “timing window” that extends for several milliseconds before or after the set interval. If the patient initiates a spontaneous breath within the timing window, the onset of the mechanical breath will be synchronized to it. If the patient fails to breathe spontaneously or cannot reach the trigger threshold within the timing window, a mechanical breath will be provided. As with IMV, spontaneous breathing between mechanical breaths is supported solely by PEEP, often resulting in two populations of breaths- assisted breaths, with relatively higher Vt, and unassisted breaths, with low Vt. Breaths may be either time-cycled or flow-cycled (see Figs. 2.15 and 2.16).
Figure 3.3 displays the use of SIMV. Breaths that are patient-triggered (the baby has created a flow change above the assist sensitivity [trigger] threshold) have a yellow inspiratory waveform. Breaths that are machine-initiated would have a red inspiratory waveform (none are shown).
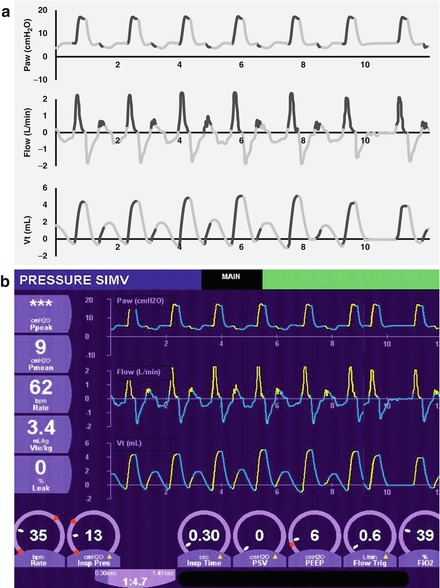
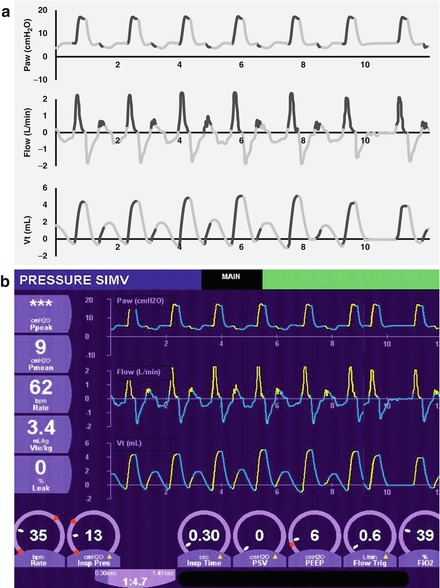
Figure 3.3




SIMV (a, schematic; b, actual). The ventilator is set at 35 breaths per minute or one breath every 1.7 s. If the baby initiates a spontaneous breath within the timing window, a mechanical breath will be synchronized to it. If the baby fails to breathe within this time, a mandatory breath will be given. In between, spontaneous breaths are supported with PEEP
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


