To determine the impact of amyloid on the prognosis of patients with hypertrophic cardiomyopathy (HC), we reviewed outcomes of patients who underwent septal myectomy for HC from March 7, 1996, to October 9, 2012, with amyloid deposits identified in operative specimens. Amyloid subtypes were differentiated by mass spectrometry–based proteomics. The survival rate was compared with that of an age-matched population (2:1) without amyloid who underwent septal myectomy for HC. Sixteen patients (mean age ± SD 71 ± 8 years; 12 men) met study criteria. All 16 had intraventricular peak systolic gradients reduced intraoperatively from 105 ± 53 mm Hg to 3 ± 7 mm Hg (p <0.001). Amyloid deposits in specimens ranged from minimal to mild. Nine patients had senile (transthyretin-type) amyloidosis, 4 had immunoglobulin-associated amyloidosis, 2 had apolipoprotein A4 amyloidosis type, and 1 had serum amyloid A type. There were no deaths before 30 days. Twelve patients had New York Heart Association class III or IV function preoperatively, and at last follow-up (median 3 years), class I or II. Only 1 patient received postoperative amyloidosis treatment. The postoperative survival rate at 2 and 4 years was 100% (n = 11 at risk) and 91% (n = 6 at risk), respectively, similar to that of the age-matched population with HC without amyloid who underwent myectomy (p = 0.13). Patients undergoing septal myectomy for HC who have histologic evidence of mild amyloidosis have early outcomes and midterm survival similar to those of patients with HC without amyloidosis who undergo myectomy. In conclusion, although longer follow-up is necessary, small amounts of amyloid, regardless of subtype, do not confer a poor prognosis on patients with HC who undergo septal myectomy.
Highlights
- •
We examined the impact of amyloid on the prognosis of patients with hypertrophic cardiomyopathy (HC).
- •
Mild amyloidosis in patients with left ventricular outflow tract obstruction and HC does not affect prognosis.
- •
Septal myectomy in patients with left ventricular outflow tract obstruction from HC and mild amyloidosis improves symptoms.
Cardiac amyloidosis is an infiltrative disorder of the myocardium typically producing diastolic dysfunction. However, 30% of patients with it have prominent subaortic thickening that produces left ventricular outflow tract obstruction, and the clinical features and hemodynamics of these patients are similar to those of patients with left ventricular outflow tract obstruction caused by hypertrophic cardiomyopathy (HC). The prognosis of patients with cardiac amyloid varies by subtype. Patients with senile amyloidosis have a median survival of 5 years versus 4 to 5 months for patients with primary amyloidosis presenting with heart failure. Incidental deposits of amyloid have been found in 1% (3 of 204) of septal myectomy surgical specimens from patients with HC and in 7% (7 of 98) of patients with other conditions (e.g., aortic stenosis, congenital aortic stenosis). To our knowledge, no studies have examined the prognostic impact of cardiac amyloid deposits in patients undergoing septal myectomy for presumed HC.
Methods
With permission from the Mayo Clinic Institutional Review Board, we retrospectively searched the medical records of all patients who underwent septal myectomy for HC from March 7, 1996, to October 9, 2012, at our tertiary care academic medical center to identify and review those with myocardial amyloid deposits. The study included data retrieval from the Mayo Clinic electronic health record, our cardiovascular surgical database, and follow-up questionnaires that include quality-of-life measurements. All patients had previously signed consent forms for their data to be included in research studies.
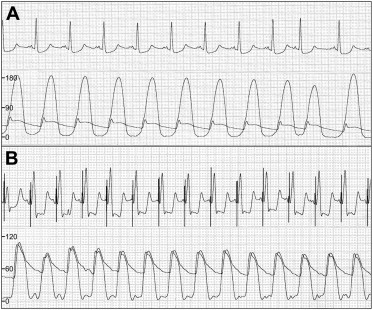
Preoperatively, all patients underwent comprehensive transthoracic echocardiography to measure the severity and location of the left ventricular outflow gradient. The gradient was measured by Doppler signal and estimated at maximal velocity of blood flow during contraction (maximal instantaneous gradient). Intraoperatively, the severity of the obstruction was measured by simultaneous direct pressure measurements.
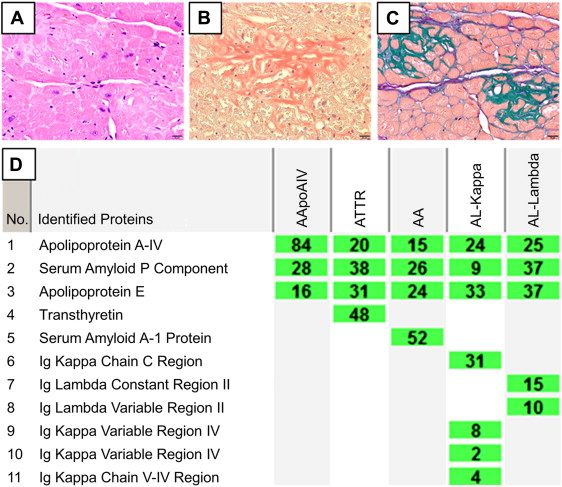
Septal myectomy was performed transaortically, as described previously. Resected myocardium from all patients was evaluated by a cardiovascular pathologist using a sulfated alcian blue amyloid stain. Classification of amyloid subtype was accomplished using laser microdissection and liquid chromatography tandem mass spectrometry–based proteomic analysis, as reported previously. The survival rate of study patients was compared 2:1 with that of an age-matched population with HC who also underwent septal myectomy.
Statistical analysis was performed using SAS statistical software (SAS Institute Inc, Cary, NC). Descriptive statistics for categorical variables are reported as frequency and percentage, whereas continuous variables are reported as mean ± SD or median (range), as appropriate. Categorical variables were compared between groups using the chi-square test or Fisher’s exact test, and continuous variables were compared using the 2-sample t test or the Wilcoxon rank sum test, as appropriate. The Kaplan-Meier method was used to estimate 2- and 4-year survival rates. p Value <0.05 was considered significant.
Results
During the study interval, a total of 1,714 patients underwent myectomy for HC; of these, 16 patients (0.9%) were found to have myocardial amyloid. The mean age ± SD of the 16 patients with amyloid deposits in septal myectomy tissue was 71 ± 8 years, and 12 were men. Presenting symptoms varied, with 75% (n = 12) of the patients having dyspnea, 13% (n = 2) fatigue, 6% (n = 1) syncope, and 6% (n = 1) angina ( Table 1 ). In 13 patients, amyloidosis was not suspected preoperatively; 2 patients had renal amyloidosis, and 1 patient had abnormal serum protein electrophoresis.
| Patient No. | Age, y | Sex | Amyloid Type | Symptoms | Preop NYHA Class | Preop EF, % | Preop Gradient, mm Hg |
|---|---|---|---|---|---|---|---|
| 1 | 52 | M | IgK | Dyspnea | 2 | 70 | 70 |
| 2 | 62 | F | IgL | Dyspnea | 3 | 70 | 180 |
| 3 | 65 | F | ApoA4 | Dyspnea | 3 | 60 | 77 |
| 4 | 66 | M | Senile | Dyspnea | 3 | 70 | 194 |
| 5 | 68 | M | Senile | Dyspnea | 3 | 75 | 150 |
| 6 | 69 | M | Senile | Fatigue | 1 | 60 | 100 |
| 7 | 69 | M | IgL | Fatigue | 2 | 70 | 217 |
| 8 | 70 | M | Senile | Dyspnea | 3 | 70 | 76 |
| 9 | 74 | M | Senile | Syncope | 3 | 80 | 80 |
| 10 | 74 | M | Senile | Dyspnea | 4 | 65 | 80 |
| 11 | 77 | M | IgK | Dyspnea | 3 | 60 | 57 |
| 12 | 77 | F | SAA | Dyspnea | 3 | 75 | 120 |
| 13 | 77 | F | Senile | Dyspnea | 3 | 76 | 79 |
| 14 | 80 | M | Senile | Dyspnea | 3 | 65 | 90 |
| 15 | 81 | M | Senile | Dyspnea | 3 | 65 | 80 |
| 16 | 81 | M | ApoA4 | Angina | 1 | 70 | 30 |
Nine patients had additional operative procedures: coronary artery bypass graft surgery (n = 4), closure of a patent foramen ovale (n = 2), mitral valve repair for flail posterior leaflet (n = 1), ligation of the left atrial appendage (n = 1), and maze procedure for atrial fibrillation (n = 1). Left ventricular outflow gradients were reduced from 105 ± 53 mm Hg preoperatively to 3 ± 7 mm Hg (p <0.001) postoperatively after myectomy ( Figure 1 ). There were no complications or early deaths.
Amyloid deposits were identified in surgical specimens from each patient, with the distribution minimal to mild. Amyloid subtypes were classified by mass spectrometry–based proteomics in all patients ( Figure 2 ). Nine patients had senile age-related transthyretin amyloidosis diagnosed on the basis of a finding of transthyretin. Four patients had immunoglobulin-associated amyloidosis (2 patients with AL-kappa and 2 patients with AL-lambda), 2 patients had apolipoprotein A4 amyloidosis, and 1 patient had serum amyloid A amyloidosis.