Hypertension is a well-known risk factor for atherosclerosis. However, data on the impact of hypertension in patients with ST elevation myocardial infarction (STEMI) are inconsistent and mainly related to studies performed in the thrombolytic era, with very few data on patients undergoing primary angioplasty. The aim of the present study was to evaluate the impact of hypertension on distal embolization, myocardial perfusion, and mortality in patients with STEMI undergoing primary percutaneous coronary intervention. Our population is represented by 1,662 patients undergoing primary angioplasty for STEMI included in the Early Glycoprotein IIb-IIIa inhibitors in Primary angioplasty database. Myocardial perfusion was evaluated by myocardial blush grade and ST segment resolution. Follow-up data were collected within 1 year after primary angioplasty. Hypertension was observed in 700 patients (42.1%). Hypertension was associated with more advanced age (p <0.001), female gender (p <0.001), diabetes (p <0.001), hypercholesterolemia (p <0.001), previous revascularization (p <0.001), anterior myocardial infarction (p = 0.006), longer ischemia time (p = 0.03), more extensive coronary artery disease (p = 0.002), more often treated with abciximab (p <0.001), and less often smokers (p <0.001). Hypertension was associated with impaired postprocedural myocardial blush grade 2 to 3 (68.2% vs 74.2%, p = 0.019) and complete ST segment resolution (51.7% vs 61.1%, p = 0.001). By a mean follow-up of 206 ± 158 days, 70 patients (4.3%) had died. Hypertension was associated with a greater mortality (6.2% vs 2.9%, hazard ratio 2.31, 95% confidence interval 1.42 to 3.73, p <0.001), confirmed after correction for baseline confounding factors (hazard ratio 1.82, 95% confidence interval 1.03 to 3.22, p <0.001). In conclusion, this study showed that among patients with STEMI undergoing primary angioplasty, hypertension is associated with impaired reperfusion and independently predicts 1-year mortality.
Availability of pharmacologic and mechanical reperfusion therapies has significantly reduced cardiac mortality among patients with acute ST elevation myocardial infarction (STEMI). However, although primary angioplasty has been shown to provide larger benefits compared with thrombolysis, a suboptimal myocardial reperfusion is still observed in a relevant proportion of patients, despite optimal epicardial recanalization. Hypertension is an established risk factor for atherosclerosis. Data on the impact of hypertension in patients with STEMI are so far inconsistent, mainly related to studies performed in the thrombolytic era. In fact, although elevated levels of heart failure, stroke, cranial hemorrhage, and mortality risk have been shown in patients with antecedent hypertension receiving thrombolytic therapy, the prognostic role of hypertension in terms of survival after primary angioplasty is still controversial. In particular, few data focused on the impact of hypertension on angiographic and clinical outcomes. Therefore, the aim of the present study was to evaluate the impact of hypertension on myocardial perfusion and mortality in patients with STEMI undergoing primary angioplasty.
Methods
Our population is represented by 1,662 consecutive patients with STEMI treated by primary angioplasty who were enrolled in 11 randomized trials, conducted from 1998 to 2005, comparing early versus late administration of glycoprotein IIb/IIIa inhibitors. Informed consent was obtained from each patient included in the trials, which were approved by local ethical committees.
All patients were admitted within 12 hours from symptom onset. All patients received aspirin (500 mg intravenously) and heparin (10,000 IU intravenously) before the procedure. All patients were treated with glycoprotein IIb/IIIa inhibitors and were prescribed aspirin after the procedure. Double oral antiplatelet therapy was prescribed for at least 4 weeks after stent implantation. Patients were categorized as having antecedent hypertension if this diagnosis was known by the patient to have been made by the family physician or after specialist referral and/or the admission note indicated a history of hypertension. Thrombolysis In Myocardial Infarction flow grade, angiographic myocardial perfusion (myocardial blush grade or myocardial perfusion grade), and distal embolization were assessed after primary angioplasty. Analysis of ST segment resolution was performed by comparison between baseline and 1- to 3-hour 12-lead electrocardiograms. ST segment resolution was defined as complete: >70%, partial: 30% to 70%, and no resolution: <30%. Clinical outcome was assessed within 1 year after primary angioplasty by telephone interview or at medical visit.
Statistical analysis was performed with the SPSS 10.0 statistical package (SPSS Inc., Chicago, Illinois). Continuous data are expressed as mean ± SD and categorical data as percentage. The analysis of variance was appropriately used for continuous variables. The chi-square test or the Fisher’s exact test was used for categorical variables. The difference in event rates between groups during the follow-up period was assessed by the Kaplan-Meier method using the log-rank test. Cox proportional hazard method analysis was used to calculate the hazard ratio adjusted for differences in baseline clinical and angiographic characteristics that were all entered in block.
Results
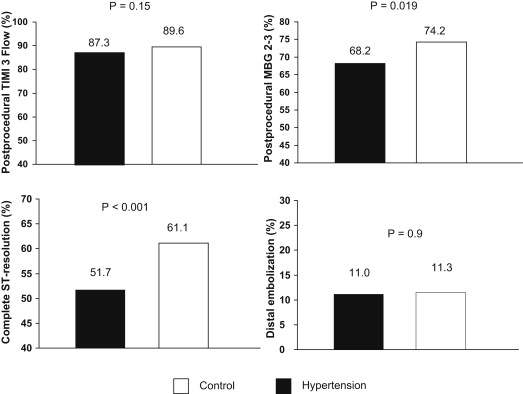
Hypertension was observed in 700 patients (42.1%). Patients’ characteristics according to hypertension are listed in Table 1 . Hypertension was associated with more advanced age (63 ± 11.7 years vs 59.5 ± 11.6 years, p <0.001), female gender (28.4% vs 18.7%, p <0.001), diabetes (23.6% vs 12.1%, p <0.001), hypercholesterolemia (45.6% vs 30%, p <0.001), previous revascularization (11.3% vs 5%, p <0.001), anterior myocardial infarction (MI; 48.2% vs 41.3%, p = 0.006), longer ischemia time (251 ± 166 minutes vs 229 ± 189 minutes, p = 0.03), more extensive coronary artery disease (62.7% vs 54.9%, p = 0.002), more often treated with abciximab (40.9% vs 33.8%, p <0.001), and less often smokers (43% vs 58.1%, p <0.001). Hypertension was associated with impaired postprocedural myocardial perfusion as evaluated by myocardial blush grade 2 to 3 (68.2% vs 74.2%, odds ratio 0.75, 95% confidence interval [CI] 0.59 to 0.95, p = 0.019) and complete ST segment resolution (51.7% vs 61.1%, odds ratio 0.68, 95% CI 0.55 to 0.85, p = 0.001), whereas no difference was observed in terms of postprocedural Thrombolysis In Myocardial Infarction 3 flow and distal embolization ( Figure 1 ).
| Variable | Hypertension (n = 700) | Control (n = 962) | p |
|---|---|---|---|
| Age (yrs) | 63 ± 11.7 | 59.5 ± 11.6 | <0.001 |
| Women | 28.4 | 18.7 | <0.001 |
| Diabetes mellitus | 23.6 | 12.1 | <0.001 |
| Smoker | 43 | 58.1 | <0.001 |
| Hypercholesterolemia ∗ | 45.6 | 30.0 | <0.001 |
| Previous myocardial infarction | 10 | 8.0 | 0.16 |
| Anterior wall myocardial infarction | 48.2 | 41.3 | 0.006 |
| Previous revascularization | 11.3 | 5.0 | <0.001 |
| Killip class >II | 3.6 | 5.3 | 0.14 |
| Time to treatment (minutes) | 251 ± 166 | 229 ± 189 | 0.03 |
| Multivessel coronary disease | 62.7 | 54.9 | 0.002 |
| Preprocedural TIMI 3 | 19 | 17.6 | 0.46 |
| Coronary stenting | 85.8 | 83.7 | 0.26 |
| Early glycoprotein IIb/IIIa inhibitors | 50.4 | 50.6 | 0.95 |
| Postprocedural TIMI 3 flow | 87.3 | 89.6 | 0.15 |
| Postprocedural MBG 2–3 | 68.2 | 74.2 | 0.019 |
| Distal embolization | 11 | 11.3 | 0.9 |
| Complete ST resolution | 51.7 | 61.1 | <0.001 |
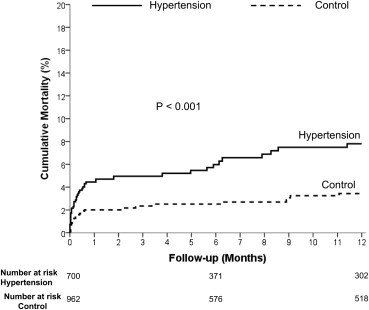
By a mean follow-up of 206 ± 158 days, 70 patients (4.3%) had died. Hypertension was associated with a significantly greater mortality (6.2% vs 2.9%, hazard ratio 2.31, 95% CI 1.42 to 3.73, p <0.001) ( Figure 2 ), confirmed after correction for baseline confounding factors (age, gender, diabetes, smoking, hypercholesterolemia, anterior MI, previous revascularization, ischemia time, multivessel disease, and myocardial perfusion; hazard ratio 1.82, 95% CI 1.03 to 3.22, p <0.001).