Our primary objective was to study postprocedural outcomes and hospitalization costs after peripheral endovascular interventions and the multivariate predictors affecting the outcomes with emphasis on hospital volume. The study cohort was derived from Healthcare Cost and Utilization Project Nationwide Inpatient Sample database (2006 to 2011). Peripheral endovascular interventions were identified using appropriate International Classification of Diseases, Ninth Revision diagnostic and procedural codes. Annual institutional volumes were calculated using unique identification numbers and then divided into quartiles. Two-level hierarchical multivariate mixed models were created. The primary outcome was inhospital mortality; secondary outcome was a composite of inhospital mortality and postprocedural complications. Amputation rates and hospitalization costs were also assessed. Multivariate analysis (odds ratio, 95% confidence interval, p value) revealed age (1.46, 1.37 to 1.55, p <0.001), female gender (1.28, 1.12 to 1.46, p <0.001), baseline co-morbidity status as depicted by a greater Charlson co-morbidity index score (≥2: 4.32, 3.45 to 5.40, p <0.001), emergent or urgent admissions(2.48, 2.14 to 2.88, p <0.001), and weekend admissions (1.53, 1.26 to 1.86, p <0.001) to be significant predictors of primary outcome. An increasing hospital volume quartile was independently predictive of improved primary (0.65, 0.52 to 0.82, p <0.001 for the fourth quartile) and secondary (0.85, 0.73 to 0.97, 0.02 for the fourth quartile) outcomes and lower amputation rates (0.52, 0.45 to 0.61, p <0.001). A significant reduction hospitalization costs ($−3,889, −5,318 to −2,459, p <0.001) was also seen in high volume centers. In conclusion, a greater hospital procedural volume is associated with superior outcomes after peripheral endovascular interventions in terms of inhospital mortality, complications, and hospitalization costs.
Peripheral arterial disease (PAD) afflicts a sizable proportion of population with significant clinical and financial implications. Recent advancements have led to widespread adoption of percutaneous endovascular interventions, replacing open surgical procedure as the primary modality for PAD. Endovascular stenting, which was primarily used for complications including intimal flaps and dissection, is now being increasingly expanded to perform primary peripheral interventions because of improvements in stent design and decreased restenosis rates. A number of recent studies have reported improved patency rates with endovascular stenting and more recently with the development of drug-eluting balloons (DEBs). The extensive adoption of any complex surgical or endovascular procedure requires critical appraisal of outcomes and their predictors with an aim to provide the most efficient and cost-effective patient care. Furthermore, despite continued emphasis on volume as an important surrogate of quality in endovascular procedures, there are sparse data on the impact of hospital volume on peripheral endovascular interventions. The primary objective of our study was 3-fold: (1) to assess inhospital mortality and postprocedural complications after peripheral endovascular interventions, (2) to evaluate the associated hospitalization costs, and (3) to further evaluate the multivariate predictors of clinical outcomes with a specific focus on the impact of hospital volume on such outcomes.
Methods
The study cohort was derived from the Nationwide Inpatient Sample (NIS) database from 2006 to 2011, a subset of the Healthcare Cost and Utilization Project (HCUP) sponsored by the Agency for Healthcare Research and Quality. The NIS is the largest publicly available all-payer inpatient care database in the United States, including data on approximately 7 to 8 million discharges per year, and is a stratified sample designed to approximate a 20% sample of United States (US) community (nonfederal, short-term, general, and specialty) hospitals. National estimates are produced using sampling weights provided by the sponsor. The details regarding the NIS data have been previously published. Annual data quality assessments of the NIS are performed, which guarantee the internal validity of the database. The NIS database results have been shown to correlate well with other hospitalization discharge databases in the United States and have also been used to explain trends in other acute medical and surgical conditions.
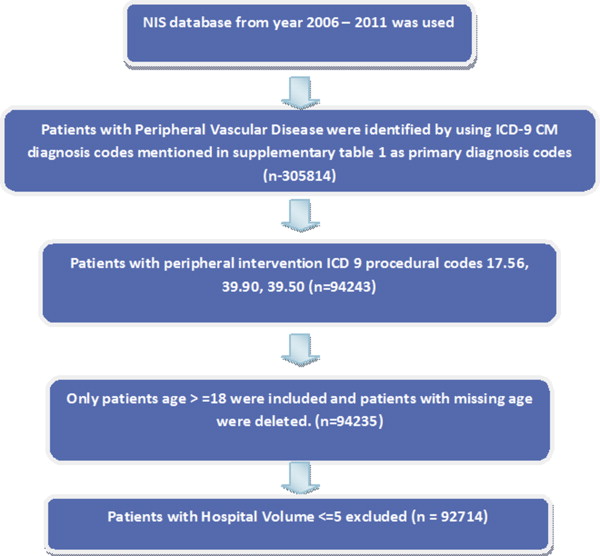
Ascertainment of all diagnoses and procedures was made using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes. Peripheral vascular disease was identified using appropriate ICD-9 codes as primary diagnosis codes. Patients aged <18 years were excluded, and peripheral endovascular interventions were identified using ICD-9 procedural codes 39.90, 39.50, or 17.56 (n = 92,714; Figure 1 ).
The primary outcome was occurrence of inhospital mortality; secondary outcome was a composite of inhospital mortality and periprocedural complications. Amputation rates were also assessed. Preventable procedural complications were identified by Patient Safety Indicators (PSIs), which have been established by the Agency for Healthcare Research and Quality to monitor preventable adverse events during hospitalization. These indicators are based on ICD-9-CM codes and Medicare severity Diagnosis-Related Groups, and each PSI has specific inclusion and exclusion criteria PSI individual measure technical specifications. Version 4.4, March 2012, was used to identify and define preventable complications. Amputation and other procedure-related complications, which included postprocedural hemorrhage requiring blood transfusion, other iatrogenic respiratory complications (which included ventilator associated pneumonia, postprocedural aspiration pneumonia, and other respiratory complications not elsewhere classified), and other vascular complications were identified using ICD-9-CM codes in any secondary diagnosis field and PSI codes. Vascular complications were defined as PSI code for accidental puncture or ICD-9-CM codes for injury to blood vessels; creation of arteriovenous fistula; vascular complications requiring surgery; vascular device, graft, or implant complications; and other vascular complications not elsewhere classified. “Any complications” was defined as occurrence of one or more postprocedural complications except amputation. Similar method has been used before.
NIS variables were used to identify patients demographic characteristics including age, gender, and race ( Table 1 ). We defined severity of co-morbid conditions using the Deyo modification of Charlson co-morbidity index (CCI). This index contains 17 co-morbid conditions with differential weights. The score ranges from 0 to 33, with greater scores corresponding to greater burden of co-morbid diseases. Facilities were considered to be teaching hospitals if they had an American Medical Association–approved residency program, were a member of the Council of Teaching Hospitals, or had a fulltime equivalent interns and residents to patient’s ratio of ≥0.25. Annual hospital volume was determined on a year-to-year basis using the unique hospital identification number to calculate the total number of procedures performed by a particular institution in a given year.
| 1st quartile | 2nd quartile | 3rd quartile | 4th quartile | Overall | P-value | |
|---|---|---|---|---|---|---|
| Hospital volume (range) | <=36 | 37 to 68 | 69 to 126 | >126 | Overall | |
| Overall (unweighted) | 22978(24.78%} | 23330(25.16%) | 23178(25.00%) | 23228(25.05%) | 92714 | |
| Overall (weighted) | 113300(24.95) | 114373(25.19) | 114284(25.17) | 112155(24.70) | 454112 | |
| Patient level variables | ||||||
| Age(Years) | <0.001 | |||||
| 18-34 | 0.22% | 0.3% | 0.25% | 0.21% | 0.25 | |
| 35-49 | 5.34% | 4.87% | 4.72% | 4.59% | 4.88 | |
| 50-64 | 29.06% | 29.19% | 28.69% | 26.5% | 28.37 | |
| 65-79 | 42.9% | 44.02% | 44.88% | 47.17% | 44.73 | |
| >=80 | 22.48% | 21.61% | 21.46% | 21.54% | 21.77 | |
| Gender | 0.775 | |||||
| Male | 54.76% | 54.81% | 54.75% | 54.95% | 54.82 | |
| Female | 45.24% | 45.19% | 45.25% | 45.05% | 45.18 | |
| Race | <0.001 | |||||
| White | 59.41% | 60.42% | 60.76% | 57.33% | 59.49 | |
| Non-white | 23.24% | 21.76% | 20.6% | 27.78% | 23.33 | |
| Missing | 17.35% | 17.82% | 18.64% | 14.88% | 17.18 | |
| Comorbidities | ||||||
| Charlson/Deyo comorbidity index | <0.001 | |||||
| 0 | 26.42% | 28.15% | 30.79% | 29.12% | 28.62 | |
| 1 | 28.5% | 29.47% | 30.74% | 32.56% | 30.31 | |
| >=2 | 45.08% | 42.38% | 38.47% | 38.32% | 41.07 | |
| Obesity ∗ | 6.36% | 6.33% | 5.67% | 6.01% | 6.09 | <0.001 |
| Hypertension(History) | 73.18% | 74.25% | 74.3% | 75.92% | 74.41 | <0.001 |
| Diabetes Mellitus | 42.14% | 41.91% | 40.46% | 45.01% | 42.37 | <0.001 |
| Heart failure | 5.63% | 4.88% | 4.08% | 3.19% | 4.45 | <0.001 |
| Pulmonary disease | 21.82% | 21.19% | 20.76% | 17.97% | 20.44 | <0.001 |
| Renal failure | 32.01% | 28.88% | 25.54% | 26.85% | 28.32 | <0.001 |
| Neurological disorder or paralysis | 6.37% | 5.69% | 4.88% | 4.26% | 5.3 | <0.001 |
| Anemia or coagulopathy | 19.37% | 16.85% | 13.61% | 12.86% | 15.68 | <0.001 |
| Hematological or oncological malignancy | 2.28% | 1.8% | 1.51% | 1.3% | 1.72 | <0.001 |
| Weight loss | 3.44% | 2.66% | 1.87% | 1.94% | 2.48 | <0.001 |
| Rheumatoid arthritis or other collagen vascular disorder | 2.28% | 2.34% | 2.05% | 1.75% | 2.11 | <0.001 |
| Depression, psychosis or substance abuse | 7.82% | 7.57% | 6.62% | 5.54% | 6.89 | <0.001 |
| Median household income category for patient’s zip code | ||||||
| 1. 0-25th percentile | 28.23% | 29.12% | 32.82% | 36.14% | 31.56 | <0.001 |
| 2. 26-50th percentile | 27.19% | 26.97% | 26.5% | 24.05% | 26.18 | <0.001 |
| 3. 51-75th percentile | 22.23% | 23.48% | 22.55% | 19.78% | 22.02 | <0.001 |
| 4. 76-100th percentile | 19.94% | 18.42% | 16.22% | 17.46% | 18.01 | <0.001 |
| Primary Payer | <0.001 | |||||
| Medicare / Medicaid | 75.26% | 76.43% | 76.28% | 77.95% | 76.48 | |
| Private including HMO | 19.69% | 19.49% | 19.96% | 19.21% | 19.59 | |
| Self pay/no charge/other | 4.88% | 3.93% | 3.68% | 2.74% | 3.81 | |
| Hospital characteristics | ||||||
| Hospital bed size | <0.001 | |||||
| Small | 12.8% | 7.39% | 7.3% | 12.63% | 10.01 | |
| Medium | 30.59% | 22.05% | 17.23% | 16.86% | 21.68 | |
| Large | 55.75% | 69.16% | 75.1% | 70.52% | 67.64 | |
| Hospital Location | <0.001 | |||||
| Rural | 12.16% | 6.76% | 5.37% | 3.84% | 7.03 | |
| Urban | 86.98% | 91.85% | 94.26% | 96.16% | 92.3 | |
| Hospital Region | <0.001 | |||||
| Northeast | 16.55% | 15.25% | 21.41% | 21.16% | 18.59 | |
| Midwest or North Central | 23.29% | 28.46% | 23.58% | 22.65% | 24.51 | |
| South | 36.52% | 37.77% | 39.16% | 40.23% | 38.42 | |
| West | 18.24% | 16.63% | 14.79% | 15.51% | 16.29 | |
| Hospital Teaching status | <0.001 | |||||
| Non-teaching | 62.69% | 52.17% | 42.2% | 34.57% | 47.94 | |
| Teaching | 36.44% | 46.43% | 57.43% | 65.43% | 51.4 | |
| Admission types | <0.001 | |||||
| Emergent/Urgent | 42.46% | 38.79% | 37.71% | 29.94% | 37.25 | |
| Elective admission | 46.27% | 52.79% | 52.66% | 66.12% | 54.42 | |
| Admission day | <0.001 | |||||
| Weekdays | 92.34% | 93.71% | 95.08% | 96.12% | 94.31 | |
| Weekend | 7.66% | 6.29% | 4.92% | 3.88% | 5.69 | |
| Type of Intervention | ||||||
| Bare metal stent | 49.95% | 53.71% | 56.2% | 48.78% | 52.18 | <0.001 |
| Angioplasty | 99.59% | 99.6% | 99.72% | 99.74% | 99.66 | <0.001 |
| Angioplasty and stents | 51.81% | 54.95% | 57.51% | 50.16% | 53.63 | <0.001 |
| Angioplasty and artherectomy and stent | 0.26% | 0.23% | 0.16% | 0.32% | 0.24 | <0.001 |
| Acute limb ischemia | 45.73% | 42.64% | 37.77% | 35.16% | 40.34 | <0.001 |
| Chronic limb ischemia | 50.86% | 53.77% | 59.27% | 62.39% | 56.56 | <0.001 |
| Iliac PVD | 3.91% | 3.25% | 3.23% | 1.97% | 3.09 | <0.001 |
| CTO (ICD9 code-440.4) | 12.92% | 12.17% | 12.77% | 11.93% | 12.45 | <0.001 |
| Thrombolysis (ICD9 code-99.10) | 10.78% | 9.45% | 6.85% | 6.88% | 8.49 | <0.001 |
| Bypass graft intervention | 4.51% | 4.93% | 4.06% | 3.53% | 4.26 | <0.001 |
| Outcomes | ||||||
| Disposition | <0.001 | |||||
| Home | 75.93% | 80.02% | 84.73% | 87.82% | 82.11 | |
| Facility/others | 21.96% | 18.27% | 13.95% | 11.07% | 16.32 | |
| Amputation | 13.21% | 11.08% | 8.34% | 6.08% | 9.69 | <0.001 |
| BKA | 2.87% | 2.22% | 1.88% | 1.31% | 2.07 | <0.001 |
| AKA | 1.69% | 1.58% | 1.11% | 0.89% | 1.32 | <0.001 |
| Minor amputation | 9.46% | 8.05% | 5.89% | 4.32% | 6.94 | <0.001 |
| Mortality | 1.67% | 1.33% | 1.11% | 0.88% | 1.25 | <0.001 |
| Total charges ($) | 23495±132 | 21583±120 | 19519±113 | 18123±106 | 20673±59 | <0.001 |
∗ Obesity defined as https://www.hcup-us.ahrq.gov/db/vars/cm_obese/nisnote.jsp#top .
The HCUP NIS contains data on total charges for each hospital in the databases, which represent the amount that hospitals billed for services. To calculate estimated cost of hospitalizations, the NIS data were merged with cost-to-charge ratios (CCR) available from HCUP. Using the merged data elements from the CCR files and the total charges reported in the NIS database, we converted the hospital total charge data to cost estimates by simply multiplying total charges with the appropriate CCR. These costs are in essence standardized, can be measured across hospitals, and are used in remainder of this report. Adjusted cost for each year was calculated in terms of the 2011 cost, after adjusting for inflation according to the latest consumer price index data released by the US government on January 16, 2013.
Stata IC 11.0 (StataCorp, College Station, Texas) and SAS 9.4 (SAS Institute Inc, Cary, North Carolina) were used for analyses. Weighted values of patient-level observations were generated to produce a nationally representative estimate of the entire US population of hospitalized patients. Differences between categorical variables were tested using the chi-square test, and differences between continuous variables were tested using the Student t test. p Value <0.05 was considered significant.
Hierarchical models or multilevel models are designed to analyze data with nested observations. The NIS data set is inherently hierarchical, viz., the data have group-specific (i.e., hospital) attributes, and within each group (i.e., hospital), there are patients, which contribute patient-specific attributes to the data. Hierarchical models take into consideration the effect of nesting (e.g., patient-level effects nested within hospital-level effects). Hence, it is superior to simple regression modeling for the available data set. Hierarchical mixed-effects logistic regression models were used for categorical-dependent variables such as primary and secondary outcomes, and hierarchical mixed-effects linear regression models were used for continuous-dependent variable such as cost of care. Two-level hierarchical models (with patient-level factors nested within hospital-level factors) were created with the unique hospital identification number incorporated as random effects within the model. In all multivariate models, we included hospital-level variables such as hospital region (Northeast, South, Midwest with West as referent), teaching versus nonteaching hospital, hospital procedure volume, and patient-level variables such as age, gender, Deyo modification of CCI, admission over the weekend, primary payer (with Medicare or Medicaid considered as referent), and admission type (elective admission as referent). All interactions were thoroughly tested. Multicollinearity, defined as a perfect linear relation or very high correlation between 2 or more predictor (independent) variables was assessed using variance inflation factor >20 suggestive of multicollinearity.
The relation between institutional volume and outcomes was represented as a nonlinear polynomial function using restricted cubic spline transformations of the volume measure. The use of splines is an established method to determine whether nonlinearity exists between a continuous variable and a dependent outcome using all data points to estimate the shape of an association between an exposure (hospital volume) and an outcome.
Results
Table 1 displays the baseline characteristics of the study population across hospital volume quartiles. Overall, 54.82% were men, 59.49% were whites. Of the patients, 41.07% had a CCI score ≥2 with hypertension (74.41%) and diabetes (42.37%) being the most common co-morbidities. Medicare or Medicaid was the primary payer (76.48%) with 19.59% of the subjects having private insurance. Of the procedures done, 67.64% were done in large hospitals, 92.3% in urban hospitals, and 51.4% in teaching hospitals. Of those procedures, 54.42% were elective, whereas 94.31% were done on weekdays.
The overall rate of periprocedural complications ( Table 2 ) was 14.46% with highest volume hospitals having the lowest rate of complications (13.36%) compared to lowest volume hospitals (15.66%; p <0.001). Likewise, the composite of inhospital mortality and complications was lower in highest volume hospitals (13.61%) compared to lower volume hospitals (16.31%; p <0.001). The overall rate of vascular complications was 11.32% with 2.7% of the patients having postprocedural hemorrhage requiring transfusion. The rate of amputation was 9.69% with lowest rate in highest volume hospitals (6.08%) compared to lowest volume hospitals (13.21%; p <0.001).
| 1st quartile | 2nd quartile | 3rd quartile | 4th quartile | Overall | P-value | |
|---|---|---|---|---|---|---|
| Hospital volume (range) | <=36 | 37 to 68 | 69 to 126 | >126 | overall | |
| Overall (unweighted) | 22978(24.78} | 23330(25.16) | 23178(25.00) | 23228(25.05) | 92714 | |
| Overall (weighted) | 113300(24.95) | 114373(25.19) | 114284(25.17) | 112155(24.70) | 454112 | |
| Mortality | 1.67% | 1.33% | 1.11% | 0.88% | 1.25 | <0.001 |
| Any complication or death | 16.31% | 15.74% | 13.94% | 13.61% | 14.90 | <0.001 |
| Any complication | 15.66% | 15.29% | 13.53% | 13.36% | 14.46 | <0.001 |
| Vascular complications | 11.66% | 11.78% | 10.88% | 10.96% | 11.32 | <0.001 |
| Compartment syndrome | 0.38% | 0.38% | 0.32% | 0.23% | 0.33 | <0.001 |
| Arteriovenous fistula | 0.13% | 0.15% | 0.18% | 0.14% | 0.15 | 0.022 |
| Rupture of artery | 0.04% | 0.05% | 0.06% | 0.05% | 0.05 | 0.525 |
| Atheroembolism of lower extremity | 0.26% | 0.29% | 0.28% | 0.13% | 0.24 | <0.001 |
| Injury to blood vessels of lower extremity | 0.03% | 0.07% | 0.05% | 0.05% | 0.05 | 0.001 |
| Vascular complications requiring surgery | 3.49% | 3.33% | 2.51% | 2.1% | 2.86 | <0.001 |
| Post-op hemorrhage requiring transfusion | 3.2% | 2.7% | 2.7% | 2.2% | 2.7 | <0.001 |
| Accidental puncture | 0.85% | 1.12% | 1.29% | 1.6% | 1.21 | <0.001 |
| Vascular device, implant, and graft complications | 4% | 4.47% | 4.07% | 4.72% | 4.31 | <0.001 |
| Other nonspecific peripheral vascular complications | 1.39% | 1.45% | 1.32% | 1.51% | 1.42 | 0.006 |
| Iatrogenic cardiac complications | 0.88% | 0.88% | 0.78% | 0.72% | 0.81 | <0.001 |
| Respiratory complications (Post-op resp failure) | 0.99% | 1.05% | 0.82% | 0.67% | 0.88 | <0.001 |
| Postoperative-Stroke/TIA | 0.11% | 0.10% | 0.09% | 0.12% | 0.10 | 0.082 |
| Renal and metabolic complications | 0.58% | 0.46% | 0.35% | 0.31% | 0.43 | <0.001 |
| Postoperative DVT/PE | 1.34% | 1.19% | 0.91% | 0.92% | 1.09 | <0.001 |
| Postop infectious complications | 2.42% | 1.8% | 1.43% | 1.39% | 1.76 | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


