Use of transcatheter endovascular stenting has been increasing in the treatment of coarctation of aorta (CoA). The present study was undertaken on adults with CoA who underwent stent placement from 2000 to 2011 to analyze the relation of hospital volumes to the outcomes of stenting in adults with CoA. It was a retrospective study based on Healthcare Cost and Utilization Project’s Nationwide Inpatient Sample (NIS) database from 2000 to 2011 and identified subjects using the International Classification of Diseases, Ninth Revision, Clinical Modification procedure code of 747.10 (CoA). Annual hospital volume was calculated using unique hospital identifiers. Weights provided by the Nationwide Inpatient Sample were used to generate national estimates. A total of 105 (weighted 521) subjects were identified with International Classification of Diseases, Ninth Revision , code of 39.90 (Endovascular stent). Hospital volumes were divided into tertiles. We compared the highest tertile (≥3 procedures annually) with other tertiles (<3 procedure annually). The composite outcomes of the analysis were procedure-related complications, length of stay (LOS), and cost in relation to the hospital volume. No inhospital death was reported in either group. Hospitals with ≥3 procedures annually had significantly lower incidence of complications (9.5% vs 23.0%) compared to the hospitals with <3 procedures annually (p-value 0.002). Similar results were obtained after multivariate regression analysis in relation to hospital volume. Shorter LOS and lower cost were observed with annual hospital volume of ≥3 procedures. In conclusion, stenting adults for CoA is remarkably safe, and the outcomes of the procedure have improved in centers with annual hospital volume of ≥3 procedures. There is also decreasing trend of procedure-related complications, shorter LOS, and lower costs compared to centers with annual volume <3 procedures.
Coarctation of Aorta (CoA) is congenital obstruction of blood flow through aorta and represents 4% to 7% of all congenital heart diseases (CHD). The treatment options for CoA have evolved from surgical resection followed by end-to-end anastomosis in 1940s to balloon angioplasty (BA) in 1970s and decades thereafter to use of endovascular stents from 1990s. The purpose of implementing wide scale use of the endovascular stents was to overcome some of the limitations encountered with the previous methods of treatment including recoarctation, residual hypertension, aortic wall injury causing dissection, and aneurysm formation. For over the past 15 years, the use of stenting is increased, particularly in adults for native and recoarctation and becoming a standard practice in such patients after results of favorable initial and intermediate outcomes reported in numerous studies. So, our retrospective study was undertaken on subjects who underwent endovascular stenting from the period of 2000 to 2011 to analyze the relation of hospital volumes to the outcomes of the procedure in adults with CoA.
Methods
The study cohorts were acquired from the Nationwide Inpatient Sample (NIS) database of 2000 to 2011, a subset of the Healthcare Cost and Utilization Project sponsored by the Agency for Healthcare Research and Quality. NIS is a deidentified database, so it was exempted from institutional review board approval. Weights provided by the NIS were used to generate national estimates. Details regarding the NIS data have been previously published for which the internal validity has been ensured by annual data quality assessments, and their results were compared with other hospitalization discharge database in the United States to strengthen the external validity. For that reason, the NIS data have also been used to study trends in other acute medical and surgical conditions. NIS sample is a stratified 20% sample of all discharges from US community hospitals that do not include rehabilitation and long-term acute care hospitals.
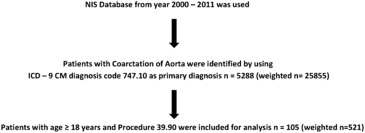
From the NIS database relevant patient population were queried using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) with primary diagnosis code of 747.10 (Coarctation of aorta [CoA]). Subjects who underwent transcatheter endovascular stenting were identified with ICD-9 code of 39.90 (Endovascular stent; Figure 1 ).
The main objectives of our study were 2-fold: (1) to analyze the post procedural complications as a primary outcome of the study and (2) to analyze the patterns of resource utilization in terms of length of stay (LOS) and cost of hospitalization in relation to the hospital volumes as a secondary outcome. During the analysis, preventable procedural complications were identified by patient safety indicators (PSIs). These indicators are based on ICD-9-CM codes and Medicare severity Diagnosis-Related Groups, and each PSI has specific inclusion and exclusion criteria. Other procedure-related complications which were not part of PSI were identified using ICD-9-CM codes (listed in Supplementary Table 1 ) in any secondary diagnosis field. “Any complications” was defined as occurrence of ≥1 postprocedure complications listed in Supplementary Table 1 . Similar method has been used before. The NIS database contains data on total charges the hospitals billed for services. These data were merged with the cost to-charge ratio files to get actual cost per hospital visit.
Demographic characteristics of the subjects including age, gender, and race were distinguished based on NIS variables ( Table 1 ). We defined severity of co-morbid conditions using Deyo modification of Charlson Comorbidity Index (CCI) as provided in Supplementary Table 2 . Facilities were considered to be teaching hospitals if they had an American Medical Association–approved residency program, were a member of the Council of Teaching Hospitals, or had a fulltime equivalent interns and residents to patient’s ratio of ≥0.25. Annual hospital volume was determined using the unique hospital identification number to calculate the total number of procedures performed by a particular institution in the study year. Hospital volume was divided into tertiles with the following cutoffs: first (≤1 procedure/year), second (2 procedures/year), and third (≥3 procedures/year). We decided to have cutoff at sixty-seventh percentile or 3 procedures annually. Thus, we compared the highest tertile (≥3 procedures annually) with other tertiles (<3 procedures annually). Of note, these volume cut offs are applicable to only NIS and are not representative of actual procedural numbers in clinical practice.
| Variable | Hospital Volume < 3 | Hospital Volume ≥ 3 | Overall | p-value |
|---|---|---|---|---|
| Number of Hospitals | 70 | 7 | 77 | |
| Total no. of observations (Unweighted) | 83 (79%) | 22 (21%) | 105 (100%) | |
| Total no. of observations (Weighted) | 417 (80%) | 105 (20%) | 521 (100%) | |
| Age (years) (Mean, Standard Error) | 38.1 ± 1.5 | 32.2 ± 3.1 | 36.9 ± 1.4 | 0.054 |
| Race | ||||
| White | 47.5 % | 45.3 % | 47.0 % | |
| Black | 2.7 % | 4.9 % | 3.1 % | 0.0004 |
| Hispanic | 16.0 % | 32.3 % | 19.3 % | |
| Other | 7.3 % | 4.1 % | 6.7 % | |
| Missing | 26.6 % | 13.4 % | 23.9 % | |
| Sex | ||||
| Male | 60.3 % | 72.0 % | 62.6 % | 0.026 |
| Female | 39.8 % | 30.0 % | 37.4 % | |
| Median Household Income Category for patient’s Zip code ∗ | ||||
| 1. 0-25th percentile | 21.1 % | 17.8 % | 20.4 % | |
| 2. 26-50th percentile | 19.7 % | 4.1 % | 16.6 % | |
| 3. 51-75th percentile | 17.9 % | 19.4 % | 18.2 % | 0.0002 |
| 4. 76-100th percentile | 23.8 % | 41.3 % | 27.3 % | |
| Missing | 17.5 % | 17.5 % | 17.5 % | |
| Primary Payer | ||||
| Medicare/Medicaid | 19.1 % | 30.4 % | 21.4 % | |
| Private | 71.6 % | 55.1 % | 68.3 % | 0.0051 |
| Other | 9.3 % | 14.5 % | 10.3 % | |
| Hospital Characteristics | ||||
| Bed size of Hospital depending on Location & Teaching Status | ||||
| Small | 9.0 % | 28.8 % | 13.0 % | |
| Medium | 18.6 % | 14.2 % | 17.7 % | <.0001 |
| Large | 72.4 % | 57.0 % | 69.3 % | |
| Hospital Location | ||||
| Rural | 2.6 % | 0.0 % | 2.0 % | 0.0991 |
| Urban | 97.5 % | 100.0 % | 98.0 % | |
| Hospital Location & Teaching Status | ||||
| Rural | 2.6 % | 0.0 % | 2.0 % | |
| Urban non-teaching | 12.6 % | 28.8 % | 15.9 % | 0.0001 |
| Urban teaching | 84.8 % | 71.3 % | 82.1 % | |
| Teaching status | ||||
| Non-teaching | 13.9 % | 28.8 % | 16.9 % | 0.0003 |
| Teaching | 86.1 % | 71.3 % | 83.1 % | |
| Hospital Region | ||||
| North-East | 12.7 % | 28.8 % | 15.9 % | |
| Mid-West | 18.6 % | 0.0 % | 14.9 % | |
| South | 20.5 % | 0.0 % | 16.4 % | <.0001 |
| West | 25.3 % | 58.1 % | 31.9 % | |
| Missing | 22.8 % | 13.1 % | 20.9 % | |
| Admission Type | ||||
| Non elective | 22.9 % | 27.7 % | 23.9 % | |
| Elective | 63.5 % | 58.9 % | 62.6 % | 0.58 |
| Missing | 13.6 % | 13.4 % | 13.5 % | |
| Admission Day | ||||
| Weekdays | 94.9 % | 100.0 % | 95.9 % | 0.019 |
| Weekends | 5.1 % | 0.0 % | 4.1 % | |
| Disposition | ||||
| Routine | 100.0 % | 95.9 % | 99.2 % | |
| Missing | 0.0 % | 4.1 % | 0.8 % | <.0001 |
| Mortality | 0.0 % | 0.0 % | 0.0 % | |
| Missing | 0.0 % | 4.1 % | 0.8 % | |
| Charlson Score † | ||||
| Score 0 | 72.6 % | 69.4 % | 71.9 % | 0.52 |
| Score ≥ 1 | 27.4 % | 30.6 % | 28.1 % | |
| Length of Stay (Median, Quartile1 – Quartile3) | 1 (1 -2) | 1 (1 -1) | 1 (1 – 2) | 0.23 |
| Cost (Median, Quartile1 – Quartile3) | 14363.9 (10277.2 – 18806.8) | 11541.1 (8806.8 – 18770.4) | 13829.7 (9822.5 – 18361.1) | 0.21 |
∗ This represents a quartile classification of the estimated median household income of residents in the patient’s ZIP Code. These values are derived from ZIP Code-demographic data obtained from Claritas. The quartiles are identified by values of 1 to 4, indicating the poorest to wealthiest populations. Because these estimates are updated annually, the value ranges vary by year. http://www.hcupus.ahrq.gov/db/vars/zipinc_qrtl/nisnote.jsp .
† Charlson/Deyo comorbidity index was calculated as per Deyo classification.
We had used Stata IC 11.0 (StataCorp, College Station, Texas) and SAS 9.4 (SAS Institute Inc, Cary, North Carolina) for data analyses. Weighted values of patient-level observations were generated to produce a nationally representative estimate of the entire US population of hospitalized patients. Differences between categorical variables were tested using the chi-square test, and differences between continuous variables were tested using the Mann-Whitney-Wilcoxson nonparametric test.
Multivariate logistic regression models were used for categorical-dependent variables such as any complications. For LOS and cost, multiple logistic regression was used after the values were dichotomized at the median value. In all multivariate models, we minimally adjusted the confounding variables related to hospitals such as hospital procedure volume and patient-level variables such as age, gender, and Charlson score/Deyo modification of CCI. The relation between institutional volume and outcomes was represented as a nonlinear polynomial function using restricted cubic spline transformations of the volume measure. The use of splines is an established method to determine whether nonlinearity exists between a continuous variable and a dependent outcome using all data points to estimate the shape of an association between an exposure (hospital volume) and an outcome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


