Mobility and function are important predictors of survival. However, their combined impact on mortality in adults ≥65 years with heart failure (HF) is not well understood. This study examined the role of gait speed and instrumental activities of daily living (IADL) in all-cause mortality in a cohort of 1,119 community-dwelling Cardiovascular Health Study participants ≥65 years with incident HF. Data on HF and mortality were collected through annual examinations or contact during the 10-year follow-up period. Slower gait speed (<0.8 m/s vs ≥0.8 m/s) and IADL impairment (≥1 vs 0 areas of dependence) were determined from baseline and follow-up assessments. A total of 740 (66%) of the 1,119 participants died during the follow-up period. Multivariate Cox proportional hazards models showed that impairments in either gait speed (hazard ratio 1.37, 95% confidence interval 1.10 to 1.70; p = 0.004) or IADL (hazard ratio 1.56, 95% confidence interval 1.29-1.89; p <0.001), measured within 1 year before the diagnosis of incident HF, were independently associated with mortality, adjusting for sociodemographic and clinical characteristics. The combined presence of slower gait speed and IADL impairment was associated with a greater risk of mortality and suggested an additive relation between gait speed and IADL. In conclusion, gait speed and IADL are important risk factors for mortality in adults ≥65 years with HF, but the combined impairments of both gait speed and IADL can have an especially important impact on mortality.
Gait speed is an important predictor of mortality, hospitalization, and nursing home placement in adults ≥65 years, as well as disability and mortality in those with cardiovascular disease in particular. A related measure, the 6-minute walk distance, is a prognostic marker of mortality in heart failure (HF). Impairment in gait speed often occurs in the setting of impairments in other geriatric measures, for example, in conjunction with deficits in lower extremity strength and balance as measured by the Short Physical Performance Battery or as a component of frailty in HF. Instrumental activities of daily living (IADL) is another important geriatric measure in HF given its association with HF incidence and mortality in adults ≥65 years. Of the available measures of mobility or function, gait speed and IADL are quick and reliable and may serve as screening tools in the clinical setting to identify adults with HF at increased risk for adverse outcomes. We, therefore, investigated the impact of gait speed and IADL, separately and combined, on all-cause mortality in adults with incident HF who are ≥65 years.
Methods
The Cardiovascular Health Study (CHS) is a prospective, population-based observational cohort study of cardiovascular disease and cardiovascular risk factors in community-dwelling US adults ≥65 years. An initial cohort of 5,201 participants was recruited in 1989 to 1990, and a second cohort of 687 African-Americans was recruited in 1992 to 1993. All participants underwent health evaluations per standardized protocols, and details of the CHS study methodology including variables collected have been published elsewhere. There were 1,139 CHS participants ≥65 years without prevalent HF at enrollment and who were diagnosed with incident HF during the study. Of these, 1,119 had complete gait speed and IADL data and were included in the present study.
Variables analyzed in this study included sociodemographic characteristics (age, gender, race, marital status, education, and income) and medical history (general health, smoking history, myocardial infarction, coronary artery disease, hypertension, diabetes mellitus, stroke, chronic obstructive pulmonary disease, cancer, kidney disease, depression as measured with the Center for Epidemiologic Studies Depression Scale, and cognitive status as measured by the Mini-Mental State Examination score) collected at baseline. Time to walk 15 feet and IADL were collected at baseline and at annual follow-up assessments. We converted the time to walk 15 feet into gait speed in meters per second and dichotomized into slower (or impaired) (<0.8 m/s) or normal (≥0.8 m/s) based on previous studies. We defined IADL impairment as dependence in ≥1 categories among the 8 activity categories. Gait speed measurements were collected from year 3 (which was the first year of follow-up) through year 11 but not in year 10. IADL was measured from year 3 through year 11. Of the 1,119 participants meeting inclusion criteria for this study, we identified 815 (73%) participants whose diagnosis of incident HF was at year 12 or earlier. This subset represented those participants who had either a gait speed or IADL assessment scheduled within 1 year of their incident HF diagnosis because neither gait speed nor IADL was assessed beyond year 11. Among these 815, a total of 606 (74%) had a completed gait speed measurement and 690 (85%) had a completed IADL assessment within 1 year before incident HF diagnosis.
Incident HF was diagnosed by central adjudication by the CHS Events Committee. The primary outcome of interest was all-cause mortality, which was adjudicated by reviewing death certificates, autopsy reports, hospital records, and interviews with attending physicians, next-of-kin, and witnesses.
We analyzed cross-sectional associations between sociodemographic and clinical characteristics and gait speed and IADL, respectively, using the chi-square and t tests. We examined the associations between (1) gait speed impairment and (2) IADL impairment and all-cause mortality using Cox proportional hazard survival models. Separate models were created for both gait speed and IADL using measurements at baseline and within 1 year of incident HF diagnosis. We further stratified subjects into those with and without preserved ejection fraction (EF) for separate survival analyses. Only 89% of the 1,119 participants had an EF recorded at baseline: 862 (86%) had EF ≥55%, 77 (8%) had EF of 45% to 54%, and 60 (6%) had EF <45%. All African-American CHS participants were recruited after the baseline echocardiogram. A second echocardiogram at year 7 was recorded for 687 (61%) of the 1,119, excluding those who died or were lost to follow-up. Among these, 526 (77%) had EF ≥55%, 94 (14%) had EF of 45% to 54%, and 68 (10%) had EF <45%. Only 618 participants had EF measurements at baseline and year 7. As the CHS EF categories (≥55% “normal,” 45% to 54% “mildly reduced,” and <45% “moderately or severely reduced”) are not concordant with the 2013 American Heart Association guideline EF classifications (≥50% “preserved,” 41% to 49% “borderline,” ≤40% “reduced,” and >40% with previous reduced EF “improved”), we incorporated both classifications for this study and defined preserved EF to include any of following criteria: (a) EF ≥55% at year 7, (b) EF ≥45% at year 7 and EF ≥45% at baseline (to exclude subjects with AHA-classified “improved EF”), or (c) EF ≥45% at baseline and died or lost to follow-up before year 7. Those with EF <45% were defined as “reduced EF,” but their numbers were too small to obtain a meaningful estimate in the Cox model, and so those with no recorded EF were included in this reference group.
We also performed a sensitivity analysis on the subset of participants who did not have impairment with regard to either gait speed or IADL at baseline to examine the impact of acute impairment of gait speed, IADL, and both factors combined in the follow-up period.
Hazard ratios (HRs) and 95% confidence intervals (CIs) were used to describe the statistical associations. All statistical tests were 2 tailed, with a p value <0.05 considered significant. Data analyses were conducted using SPSS statistics software, version 21 (IBM Corporation, Somers, New York) and Stata, v.12.1 (Stata, Inc., College Station, Texas).
Results
The mean age at enrollment for eligible participants in this study was 74 years (SD ± 6), 51% were women and 14% were nonwhite. The median gait speed at baseline was 0.76 m/s with an interquartile range of 0.65 to 0.91 m/s, and 566 (51%) had a gait speed <0.8 m/s. Men had a significantly faster mean gait speed (0.87 m/s) than women (0.78 m/s; p <0.001). Among the 1,119 participants, 780 (68%) reported no IADL impairments, 270 (24%) reported 1, and 89 (8%) reported ≥2 impairments. Slower gait speed was positively correlated with age, female gender, nonwhite race, fewer years of education, and lower income, whereas IADL impairment was more likely to be positively correlated with a number of medical conditions ( Table 1 ).
| Number (%) or mean (±SD) | IADL | P-value † | Gait Speed ∗ | P-value † | ||
|---|---|---|---|---|---|---|
| IADL=0 (n=780) | IADL ≥1 (n=359) | ≥ 0.8 m/s (n=553) | < 0.8 m/s (n=566) | |||
| Age at study entry (years) | 74 (±6) | 76 (±6) | <0.001 | 73 (±5) | 76 (±6) | <0.001 |
| Age at the time of incident HF | 81 (±6) | 82 (±4) | 0.04 | 80 (±6) | 82 (±6) | <0.001 |
| Female | 361 (46%) | 224 (62%) | <0.001 | 224 (41%) | 345 (61%) | <0.001 |
| Non-white race | 99 (13%) | 64 (18%) | 0.02 | 56 (10%) | 101 (18%) | <0.001 |
| Married | 513 (66%) | 221 (62%) | 0.18 | 396 (72%) | 328 (58%) | <0.001 |
| Education (college or higher) | 325 (42%) | 133 (37%) | 0.15 | 264 (48%) | 186 (33%) | <0.001 |
| Income > $25,000 | 254 (33%) | 99 (28%) | 0.09 | 206 (37%) | 141 (25%) | <0.001 |
| General health fair to poor | 185 (24%) | 176 (49%) | <0.001 | 125 (23%) | 235 (41%) | <0.001 |
| Smoking (pack years) | 20 (±28) | 18 (±28) | 0.31 | 17 (±27) | 22 (±28) | 0.002 |
| Myocardial Infarction | 109 (149%) | 69 (19%) | 0.02 | 94 (17%) | 82 (14%) | 0.25 |
| Coronary artery disease | 198 (25%) | 126 (35%) | 0.001 | 170 (31%) | 149 (26%) | 0.10 |
| Hypertension | 421 (54%) | 214 (60%) | 0.08 | 301 (54%) | 324 (57%) | 0.34 |
| Diabetes mellitus | 187 (24%) | 85 (24%) | 0.90 | 125 (23%) | 142 (25%) | 0.33 |
| Stroke | 35 (5%) | 27 (8%) | 0.05 | 27 (5%) | 45 (8%) | 0.11 |
| Chronic obstructive pulmonary disease | 90 (11%) | 74 (21%) | <0.001 | 76 (14%) | 86 (15%) | 0.49 |
| Cancer | 108 (14%) | 62 (17%) | 0.13 | 90 (16%) | 77 (14%) | 0.21 |
| Kidney disease | 192 (25%) | 114 (32%) | 0.01 | 138 (25%) | 165 (29%) | 0.11 |
| Depression score | 4.1 (±4.1) | 6.4 (±5.1) | <0.001 | 3.9 (±3.9) | 5.7 (±5.0) | <0.001 |
| Mini Mental State Examination score | 28 (±2) | 27 (±3) | 0.001 | 28 (±2) | 27 (±3) | <0.001 |
∗ Twenty participants had missing gait speed data.
† P-values are calculated using Pearson Chi-Square tests of association for categorical variables and F tests of equal means for continuous variables.
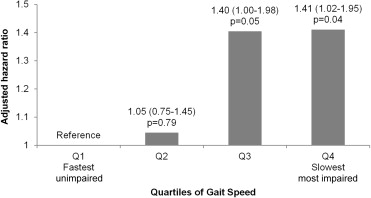
Overall, 740 (66%) of the 1,119 participants died. The median time from enrollment to incident HF was 6.4 years, and the median time from incident HF to death was 1.7 years. Slower gait speed and IADL impairment, whether assessed at baseline or within 1 year of incident HF, was each independently associated with all-cause mortality ( Table 2 ). The adjusted hazard ratio for IADL was substantially greater, whereas that for gait speed did not differ meaningfully, for models using assessments within 1e year of incident HF ( Table 2 ). There was no meaningful difference observed in our stratified analysis of the impact of gait speed in women (HR 1.38, 95% CI 1.09 to 1.75; p = 0.009) and men (HR 1.22, 95% CI 0.99 to 1.51; p = 0.08). Analysis using quartiles of gait speed did not demonstrate a dose-response effect of gait speed on all-cause mortality ( Figure 1 ).
| Model | Variables Measured at Baseline (N=1,119) | Variables Measured within One Year of Incident HF (N=606) | ||
|---|---|---|---|---|
| Hazard Ratio (95% CI) | P-Value | Hazard Ratio (95% CI) | P-Value | |
| Gait Speed Impairment (<0.8 m/s vs ≥0.8 m/s) | ||||
| Unadjusted Model | 1.45 (1.25-1.68) | <0.001 | 1.57 (1.29-1.91) | <0.001 |
| Adjusted (all with incident HF) | 1.28 (1.10-1.50) | 0.002 | 1.37 (1.10-1.70) | 0.004 |
| Adjusted (those with preserved ejection fraction † ) | 1.36 (1.12-1.65) | 0.002 | 1.45 (1.12-1.86) | 0.004 |
| Adjusted (those with reduced ejection fraction ‡ ) | 1.14 (0.87-1.50) | 0.4 | 1.51 (0.98-2.32) | 0.06 |
| IADL Impairment (≥1 Impairments vs. None) | ||||
| Unadjusted Model | 1.23 (1.06-1.43) | 0.006 | 1.69 (1.41-2.02) | <0.001 |
| Adjusted (all with incident HF) | 1.18 (1.01-1.39) | 0.04 | 1.56 (1.29-1.89) | <0.001 |
| Adjusted (those with preserved ejection fraction † ) | 1.14 (0.93-1.39) | 0.2 | 1.55 (1.23-1.95) | <0.001 |
| Adjusted (those with reduced ejection fraction ‡ ) | 1.28 (0.96-1.69) | 0.09 | 1.53 (1.07-2.20) | 0.02 |
∗ Potential confounding factors included: Age at incident HF, gender (female vs. male), race (non-white vs. white), marital status (married vs. not), education (any college or higher), and income (>$25,000 vs. not), depression score, Mini Mental State Examination Score, hypertension, coronary artery disease, and chronic kidney disease, as determined at study entry.
† Sample size for individuals with preserved ejection fraction were 756 (68%) for baseline model and 427 (70%) for the one year prior to HF model.
‡ Sample size for individuals with reduced/unknown ejection fraction were 363 (32%) for baseline model and 179 (30%) for the one year prior to HF model.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


