Limited studies with relatively small sample sizes have reported that elevated d -dimer levels on admission were associated with increased risk of short-term mortality in patients with type A acute aortic dissection (AAD). However, there were unavailable data regarding the impact of admission d -dimer levels on long-term outcomes. Our present study aimed to evaluate the association of admission d -dimer levels with both inhospital and long-term all-cause mortality in patients with type A AAD. A total of 212 consecutive patients with type A AAD were enrolled. d -Dimer levels were measured on admission, and patients were followed up prospectively. The primary end points were inhospital and long-term all-cause mortality. The median length of follow-up was 18.8 months (interquartile range 6.7 to 24.4 months). The inhospital and long-term all-cause mortality rates were 12.7% and 12.4%, respectively. Compared with the survivors, the nonsurvivors had significantly higher d -dimer levels (p <0.001). When divided into 4 groups according to admission d -dimer quartiles, patients in Q4 (>6.10 μg/ml) had the highest inhospital and long-term mortality among groups. After multivariate adjustment, the d -dimer level in Q4 (>6.10 μg/ml) was an independent risk factor for inhospital mortality (hazard ratio [HR] 6.12, 95% confidence interval 1.35 to 27.89, p = 0.019) in addition to surgical treatment; however, this was not an independent predictor for long-term mortality. In conclusion, our study with a relatively large sample size suggested that elevated admission d -dimer levels (>6.10 μg/ml) might be a predictor for increased risk of inhospital mortality, and urgent-emergent surgery might be needed in patients with elevated d -dimer levels on admission. However, d -dimer levels at admission failed to predict long-term mortality.
Highlights
- •
Admission d -dimer independently predicts inhospital mortality.
- •
Admission d -dimer had no impact on long-term mortality.
- •
Elevated admission d -dimer level may be a marker of urgent-emergent surgery.
d -Dimer, which is a degradation product of cross-linked fibrin, is elevated in patients with acute aortic dissection (AAD). In recent years, several studies evaluated the prognostic value of d -dimer levels on admission in patients with AAD and reported that elevated d -dimer levels were associated with poor short-term outcome. However, the sample size in these studies was relatively small, which may be insufficient to reach a reliable conclusion. Moreover, these studies only investigated the association between d -dimer levels and short-term (inhospital) outcome, and studies with long-term follow-up are lacking. Therefore, we conducted an observational study to evaluate the predictive value of admission d -dimer levels for both inhospital and long-term outcomes with a relatively large sample of patients with type A AAD.
Methods
From March 2010 to June 2011, consecutive patients with suspected AAD presented to Fuwai hospital were enrolled. The diagnosis of type A AAD was confirmed by multidetector computed tomographic scanning. This study was approved by the ethical committees of Fuwai hospital, and written informed consent was obtained from each patient.
Baseline characteristic data were collected on admission. Admission plasma d -dimer levels were measured by Stago Evolution automatic blood coagulation analyzer (France) with Bi-directional Lateral Flow Immunoassay test (Relia Biotechnologies, Shenzhen) according to the standard protocol of the supplier. Hospital management including medical and surgical treatment was well recorded. The rationale and strategy of surgical intervention were determined by surgeons according to the American Association for Thoracic Surgery 2010 Guidelines for the Diagnosis and Management of Patients with Thoracic Aortic Disease.
Inhospital outcome data were collected using medical records. After discharge, follow-up was performed by telephone. The study end points were inhospital and long-term all-cause mortality.
Continuous variables are presented as the mean ± SD or median and interquartile range according to whether they follow Gaussian distributions. Categorical data are presented as numbers and proportion. Baseline characteristics were compared between survivors and nonsurvivors using unpaired Student’s t tests, Wilcoxon Mann-Whitney tests for continuous data, and the chi-square tests for categorical data. Inhospital and long-term mortality among the d -dimer quartiles was compared using the chi-square tests. Univariate and multivariate Cox proportional hazard analyses were used to analyze the factors related to inhospital and long-term mortality with hazard ratios (HRs) and the 95% confidence interval (CI). Kaplan-Meier survival curves among groups stratified by admission d -dimer quartiles were constructed and compared using the log-rank test. A p value <0.05 was considered to be statistically significant. All the statistical analyses were performed using SPSS statistical software, version 19.0 (SPSS Inc., Chicago, Illinois).
Results
A total of 375 patients were diagnosed with AAD from March 2010 to June 2011, of which 225 were Stanford type A AAD and 150 were Stanford type B AAD. After excluding 13 patients for whom there was incomplete data or who were lost to follow-up, 212 patients with type A AAD were analyzed. The median length of follow-up was 18.8 months (interquartile range 6.7 to 24.4 months). Inhospital mortality was 12.7% (27 of 212). For the 185 hospital survivors, 23 patients died during long-term follow-up, with 12.4% long-term mortality.
Table 1 summarizes clinical features of survivors and nonsurvivors. Compared with the survivors, the nonsurvivors had significantly higher d -dimer levels, white blood cell (WBC) counts, and creatinine levels (all p <0.001). The proportion of surviving patients who received surgical treatment was significantly higher than of nonsurvivors (74.7% vs 14.0%, p <0.001).
| Variable | All patients (n=212) | Survivor (n=162) | Non-survivor (n=50) | p value |
|---|---|---|---|---|
| Age (years) | 48.5±11.5 | 47.7±11.6 | 51.2±10.7 | 0.060 |
| Men | 161 (75.9%) | 121 (74.7%) | 40 (80.0%) | 0.571 |
| Hypertension | 141 (66.5%) | 105 (64.8%) | 36 (72.0%) | 0.394 |
| Coronary artery disease | 7 (3.3%) | 7 (4.3%) | 0 (0.0%) | 0.203 |
| Smoker | 82 (38.7%) | 58 (35.8%) | 24 (48.0%) | 0.137 |
| Alcohol use | 44 (20.8%) | 35 (21.6%) | 9 (18.0%) | 0.692 |
| Onset-to-admission intervals (hours) | 18.0 (8.0-24.0) | 19.0 (10.0-24.0) | 14.0 (6.0-30.0) | 0.195 |
| On admission: | ||||
| Systolic blood pressure (mmHg) | 144.1±17.2 | 144.4±17.3 | 143.6±17.4 | 0.882 |
| Heart rate (bpm) | 83.0 (75.0-96.0) | 83.0 (75.0-93.0) | 86.0 (75.0-102.0) | 0.510 |
| White blood cell count (×10 9 /L) | 10.4 (7.4-13.5) | 9.9 (7.1-12.5) | 12.1 (10.1-17.9) | <0.001 |
| Platelet count (×10 9 /L) | 177.0 (137.0-237.0) | 179.0 (141.0-244.0) | 157.0 (111.5-220.0) | 0.100 |
| C-reactive protein (mg/L) | 42.2 (7.0-105.5) | 30.9 (6.5-85.1) | 74.2 (8.6-132.0) | 0.188 |
| D-dimer (μg/mL) | 2.8 (1.1-6.1) | 2.5 (0.8-4.9) | 6.8 (1.5-16.0) | <0.001 |
| Creatinine (μmol/L) | 88.4 (73.6-110.7) | 87.3 (71.6-102.0) | 102.5 (75.9-168.2) | <0.001 |
| Aorta ascenden diameter (mm) | 47.3±11.4 | 47.4±12.1 | 47.4±8.8 | 0.999 |
| Pericardial effusion | 38 (17.9%) | 22 (13.6%) | 16 (32.0%) | 0.005 |
| Surgical treatment | 128 (60.4%) | 121 (74.7%) | 7 (14.0%) | <0.001 |
Inhospital and long-term mortality were compared according to the admission d -dimer quartiles. As demonstrated in Figure 1 , inhospital mortality was significantly higher in Q4 (30.2%), followed by Q3 (11.3%) and Q2 (5.7%), and it was the lowest in Q1 (3.8%; p <0.001). Similarly, the long-term mortality in Q4 (24.3%) was significantly higher than in the other 3 groups (p = 0.046).
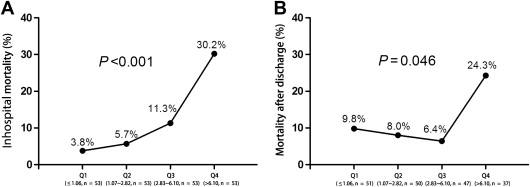
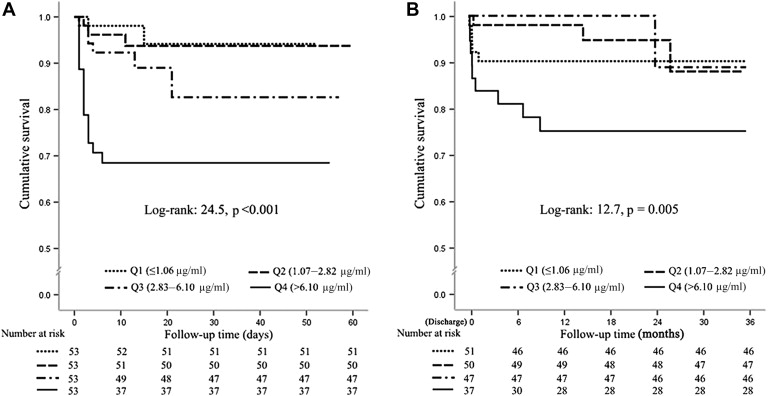
Figure 2 demonstrates the survival curves as stratified by admission d -dimer quartiles. The Q4 group displayed a steep decrease in cumulative inhospital survival, which made it significantly different from the other groups (log-rank p <0.001). Similar trends were observed during long-term follow-up after discharge (log-rank p = 0.005).
The association of d -dimer levels on admission with inhospital and long-term mortality was analyzed using univariate Cox proportional hazard analysis ( Table 2 ). As a continuous variable, d -dimer levels were positively associated with inhospital death (HR 1.12, 95% CI 1.07 to 1.18, p <0.001). As a categorical variable and compared with Q1, d -dimer levels in Q4 (>6.10 μg/ml) were associated with a 10-fold increased risk of inhospital mortality (HR to 10.23, 95% CI 2.34 to 44.63, p = 0.002). The other factors associated with inhospital mortality included admission WBC counts, creatinine levels, and surgical treatment. Similar results were observed between admission d -dimer levels and long-term mortality ( Table 2 ).
| Variable | In-hospital mortality | Long-term mortality | ||||
|---|---|---|---|---|---|---|
| HRs | 95%CI | p value | HRs | 95%CI | p value | |
| Sex (female vs. male) | 0.84 | 0.34-2.09 | 0.711 | 0.30 | 0.07-1.28 | 0.103 |
| Age (years) | 1.01 | 0.98-1.05 | 0.464 | 1.03 | 0.99-1.07 | 0.142 |
| D-dimer (continuous) | 1.12 | 1.07-1.18 | <0.001 | 1.09 | 1.02-1.17 | <0.001 |
| Q2 vs. Q1 | 1.53 | 0.26-9.17 | 0.641 | 0.55 | 0.13-2.32 | 0.419 |
| Q3 vs. Q1 | 3.15 | 0.63-15.65 | 0.166 | 0.65 | 0.16-2.73 | 0.555 |
| Q4 vs. Q1 | 10.23 | 2.34-44.63 | 0.002 | 3.15 | 1.03-9.62 | 0.044 |
| C-reactive protein (continuous) | 1.00 | 0.99-1.01 | 0.763 | 1.00 | 1.00-1.01 | 0.156 |
| White blood cell count (continuous) | 1.16 | 1.07-1.24 | <0.001 | 1.15 | 1.06-1.26 | 0.001 |
| Platelet count (continuous) | 0.99 | 0.99-1.000 | 0.061 | 1.00 | 0.99-1.00 | 0.353 |
| Creatinine (continuous) | 1.01 | 1.003-1.011 | 0.001 | 1.01 | 1.004-1.02 | 0.001 |
| Pericardial effusion | 2.29 | 1.00-5.28 | 0.051 | 2.97 | 1.16-7.56 | 0.023 |
| Aorta ascenden diameter (continuous) | 1.02 | 0.99-1.06 | 0.198 | 0.99 | 0.95-1.04 | 0.741 |
| Surgical intervention | 0.02 | 0.003-0.15 | <0.001 | 0.15 | 0.05-0.40 | <0.001 |
Table 3 demonstrates predictors of inhospital and long-term mortality by multivariate Cox proportional hazard analysis. After adjustment for age, gender, admission WBC counts, d -dimer and creatinine levels and surgical treatment, d -dimer levels in Q4 (>6.10 μg/ml) independently predicted a sixfold increased risk of inhospital death (HR 6.12, 95% CI 1.35 to 27.89, p = 0.019). Surgical treatment was the only protector of inhospital mortality (HR 0.02, 95% CI 0.003 to 0.15, p <0.001). In contrast, after multivariate adjustment, admission d -dimer levels were not independent predictors for long-term mortality, and the factors associated with long-term mortality were admission WBC counts, pericardial effusion, and surgical treatment, and surgical treatment was the only protector (HR 0.15, 95% CI 0.05 to 0.41, p <0.001).
| In-hospital mortality | Long-term mortality | ||||||
|---|---|---|---|---|---|---|---|
| Variable | HRs | 95%CI | p value | Variable | HRs | 95%CI | p value |
| D-dimer | White blood cell count | 1.15 | 1.05-1.27 | 0.004 | |||
| Q2 vs. Q1 | 1.23 | 0.20-7.61 | 0.825 | Pericardial effusion | 3.29 | 1.24-8.73 | 0.017 |
| Q3 vs. Q1 | 1.78 | 0.36-8.91 | 0.483 | Surgical intervention | 0.15 | 0.05-0.41 | <0.001 |
| Q4 vs. Q1 | 6.12 | 1.35-27.89 | 0.019 | ||||
| Surgical intervention | 0.02 | 0.003-0.15 | <0.001 | ||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


