Iliofemoral Reconstruction: Ipsilateral and Crossover
Richard F. Neville
Bao Nguyen
Peripheral arterial occlusive disease often occurs in a multilevel distribution. This multilevel distribution carries significant therapeutic implications, as the first principle guiding the planning of a successful revascularization remains treating inflow disease prior to further distal procedures, if needed. Inflow procedures address occlusive disease in the aorta and iliac arteries of symptomatic limbs. Symptomatic aortoiliac disease is usually manifested as claudication in the calf with extension to the thigh and buttock area. Rest pain and tissue loss are unusual with isolated aortoiliac disease because significant collaterals often develop to maintain distal perfusion. Limb-threatening ischemia, rest pain, and tissue loss frequently occur when multilevel occlusive disease involves a combined distribution of aortoiliac and infrainguinal disease. Claudication and rest pain may be relieved by treatment of the inflow problem; however, tissue loss may require the addition of a distal revascularization. The Leriche syndrome is a classic symptom complex of aortoiliac disease involving hip and thigh claudication, impotence, and absent femoral pulses. Impotence occurs as flow to the internal pudendal artery is decreased, causing insufficient flow for erectile function. Indications for treatment of inflow disease include disabling claudication, rest pain, or tissue loss.
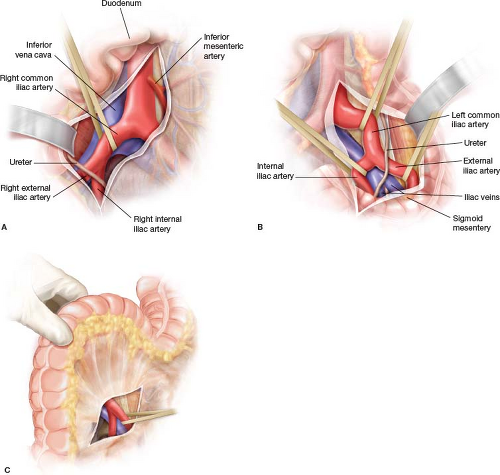
Advances in endovascular therapy have established angioplasty and stenting as the most common intervention for aortoiliac lesions, especially for Trans-Atlantic Inter-Society Consensus (TASC) A/B lesions. Although the results of endovascular interventions are less durable for TASC C lesions, these options are still acceptable for patients with medical comorbidities. Nevertheless, when endovascular interventions are unsuccessful for these lesions or inadvisable (as for TASC D lesions), operative treatment may be indicated. Surgical procedures performed for aortic and unilateral iliac occlusive disease include endarterectomy, anatomical bypasses such as aorto- or iliofemoral bypasses, or extra-anatomical configurations such as axillofemoral, femorofemoral, or crossover iliofemoral bypasses. In this chapter, we will focus on the surgical techniques and relevant details of ipsilateral and crossover iliofemoral bypasses.
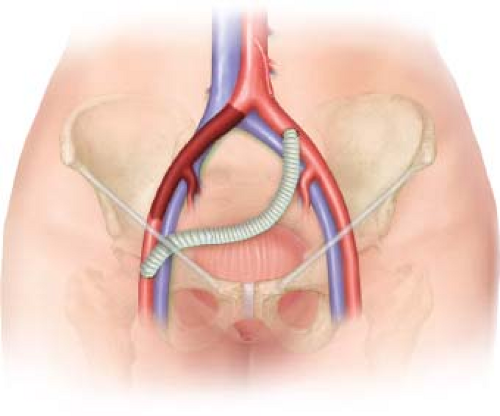
Ipsilateral iliofemoral bypass (Fig. 21.1) may be considered when the aorta and proximal common iliac artery are free of hemodynamically significant disease. When the ipsilateral common iliac artery is occluded but the contralateral iliac circulation is
well preserved, iliofemoral crossover bypass (Fig. 21.2) is a good alternative, especially in high-risk patients because this procedure can avoid cavitary exposure and may be done under regional anesthesia. Crossover iliofemoral bypass is certainly favored when there is heavy scarring or infection in the contralateral femoral region. Careful preoperative evaluation and medical optimization are essential to obtain good outcomes, with an individualized approach considered for each patient.
well preserved, iliofemoral crossover bypass (Fig. 21.2) is a good alternative, especially in high-risk patients because this procedure can avoid cavitary exposure and may be done under regional anesthesia. Crossover iliofemoral bypass is certainly favored when there is heavy scarring or infection in the contralateral femoral region. Careful preoperative evaluation and medical optimization are essential to obtain good outcomes, with an individualized approach considered for each patient.
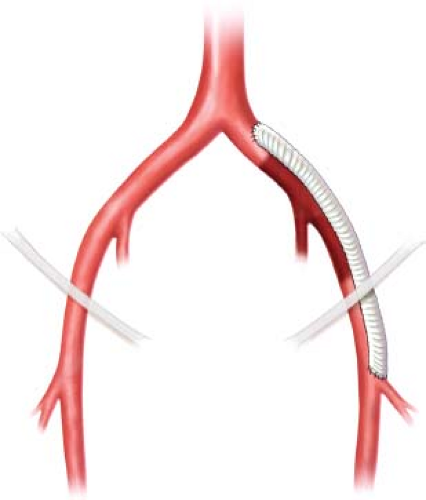 Figure 21.1 A schematic of an ipsilateral iliofemoral bypass. Graft patency is best when the femoral anastomosis is directed toward the profunda femoral artery. |
In the patient with unilateral inflow occlusive disease an iliofemoral bypass is an excellent option, especially for patients who are at increased risk for an abdominal aortic procedure. The operation is performed through a flank approach and a retroperitoneal dissection. The bypass extends from the common iliac artery to the femoral artery typically using an 8-mm Dacron or ePTFE graft. The graft is tunneled in an anatomic position in the retroperitoneum and brought under the inguinal ligament into the groin for anastomosis to the femoral artery. Results are excellent with 5-year patency reported between 75% and 90%.
Extra-anatomic bypasses do not follow the normal anatomic course of the arterial tree. These operations are performed when the risk of an anatomical procedure is excessive due to the patient’s medical condition or infected tissue planes. Crossover iliofemoral
bypass is appropriate for unilateral aortoiliac disease in a patient considered a poor operative risk for an intra-abdominal procedure. The bypass requires a contralateral iliac artery without significant disease to serve as inflow. Blood is routed from the contralateral iliac artery to enhance flow to the femoral artery on the symptomatic side typically with an 8-mm Dacron or externally reinforced ePTFE graft. Progression of disease in the donor iliac artery can occur; however, it is relatively uncommon.
bypass is appropriate for unilateral aortoiliac disease in a patient considered a poor operative risk for an intra-abdominal procedure. The bypass requires a contralateral iliac artery without significant disease to serve as inflow. Blood is routed from the contralateral iliac artery to enhance flow to the femoral artery on the symptomatic side typically with an 8-mm Dacron or externally reinforced ePTFE graft. Progression of disease in the donor iliac artery can occur; however, it is relatively uncommon.
Preoperative preparation should identify and medically optimize the comorbid conditions that could result in serious postoperative complications such as myocardial or cerebrovascular ischemia. In patients who are at high risk for coronary artery occlusive disease, noninvasive testing such as ischemic stress test by dipyridamole thallium scintigraphy or stress echocardiography should be obtained, if indicated. Arterial noninvasive testing such as segmental pressures and waveforms with ankle brachial indices (ABIs) should be obtained to assess the severity of the disease at baseline. Although CT and MR angiography can deliver excellent images of the aortoiliac circulation, multiplanar angiography of the bilateral iliac and femoral arterial system should be considered to evaluate the adequacy of the inflow and distal targets in planning for a successful operation. If there is any doubt about subtle disease of the donor iliac artery, pressure gradients should be measured and endovascular intervention executed as indicated to optimize to donor iliac system before the planned surgical revascularization. For male patients who are sexually active, the possibility of sexual dysfunction should be discussed.
Positioning
The procedure is best performed in an operating room with endovascular capabilities. Patients are positioned supine with the abdomen prepped widely from the xiphoid to the bilateral knees. Consideration should be given to full circumferential sterile preparation of the symptomatic leg in case additional procedures are required. General anesthesia is used under most circumstances, but if the patients are deemed high-risk for general anesthesia, spinal or epidural anesthesia is an alternative, and local anesthesia alone is possible for femoral–femoral bypass. Prophylactic antibiotics should be administered.
Technique
Iliofemoral Bypass
The femoral artery of the symptomatic side is exposed first. If the common femoral, superficial femoral, and profunda femoral arteries are patent without significant disease based on preoperative imaging, a longitudinal incision or transverse groin incision may be used for exposure. The common femoral artery is exposed and dissected distally to its bifurcation where the proximal superficial femoral and profunda femoral arteries are isolated and controlled. Circumflex branches should be preserved if possible. On the other hand, if the profunda femoral is the only patent target on the preoperative angiogram, the incision should be made more distally in the upper thigh to directly expose the profunda artery to avoid crossing the groin crease unnecessarily in order to lower the risk of postoperative wound complications. It is very important that the profunda femoral artery is adequately exposed, which involves dividing of major crossing profunda venous branches, for a profundaplasty if there is disease at the orifice because the long-term patency of the bypass depends heavily on the optimization of the profunda outflow.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree