I. INTRODUCTION
A. Epidemiology. More than 50 million people in the United States are diagnosed with systemic hypertension, many of whom are inadequately treated. Approximately 1% of those poorly treated progress to a crisis phase, accounting for more than 50% of all cases of hypertensive crisis. Although the incidence is decreasing due to improved awareness, treatments, and public health measures, patients with untreated hypertension or suboptimal blood pressure control remain more susceptible to acute rises in blood pressure. Patients with secondary causes of hypertension are also at higher risk for hypertensive crisis. Unless promptly recognized and treated, hypertensive crisis can lead to acute central nervous system, renal and cardiovascular dysfunction, and, possibly, death. Effective and prompt antihypertensive treatment improves prognosis.
B. Definitions. Hypertensive crisis is defined as having either a hypertensive emergency or hypertensive urgency. According to the Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure, normal blood pressure is defined as a systolic blood pressure < 120 mm Hg and a diastolic blood pressure < 80 mm Hg. Severe hypertension is defined as a systolic blood pressure > 180 mm Hg and/or diastolic blood pressure > 120 mm Hg.
1. Hypertensive emergency. Hypertensive emergency is defined as
severe hypertension with evidence of acute end-organ damage, which can be manifested by a variety of syndromes (
Table 35.1). Severe hypertension in the presence of chronic organ damage without associated acute manifestations does not constitute an emergency. Delineating hypertensive emergency from urgency is important because it implicates the need for immediate parenteral blood pressure lowering therapy in a monitored setting (typically intensive care unit [ICU]) to minimize tissue damage and long-term complications. Delay may cause irreversible organ dysfunction and death.
2. Hypertensive urgency. Hypertensive urgency, on the other hand, is generally defined as severe hypertension without acute end-organ damage. In the absence of symptoms or acute organ dysfunction, severe hypertension can be lowered over a period of days to weeks. Patients can be treated with oral medications and usually managed as outpatients.
3. Pseudoemergencies. Pseudoemergencies are acute rises in blood pressure attributed to a physiologic trigger, causing a massive sympathetic or catecholamine surge. These are typically seen as the result of pain, hypoxia, hypercarbia, hypoglycemia, anxiety, or a postictal state. These scenarios must be differentiated from true hypertensive crises because the management differs significantly. Treatment is directed at the underlying trigger and does not necessarily include antihypertensive medications.
II. PATHOPHYSIOLOGY
A. Autoregulation. Understanding autoregulation is the cornerstone of managing hypertensive crises safely while minimizing the risk of iatrogenic complications. The kidney, brain, fundi, and heart all possess
autoregulatory mechanisms that maintain blood flow at near-constant levels despite fluctuations in blood pressure. This protects these vital organs from the consequences of hypoperfusion with decrease in blood pressure and hyperperfusion with increase in blood pressure. The cardiovascular equivalent to Ohm’s law in physics (
I =
V/
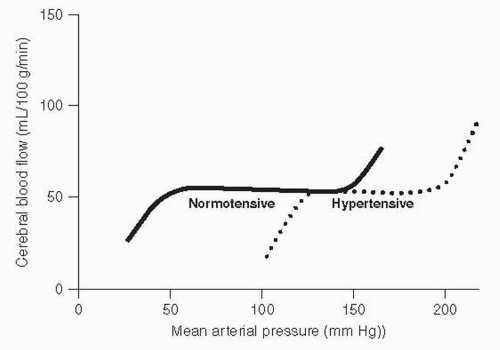
R) is that blood flow is equal to pressure divided by resistance. Constant blood flow is maintained by parallel changes in these two parameters: pressure and resistance. The endothelial layer in these vessels controls local autoregulatory vasoconstriction when the perfusion pressure increases and vasodilation when perfusion pressure decreases. There is a range of pressures for which the autoregulatory mechanism functions normally. In
normotensive patients or in those with adequate hypertension management, this range of mean arterial pressures (MAPs) is approximately between 60 and 120 mm Hg. Loss of autoregulatory control at an MAP of 120 mm Hg in patients without preexisting chronic hypertension explains why a seemingly trivial elevation in blood pressure (160/100 mm Hg) can have severe end-organ damage. Classic examples of this phenomenon occur with acute illnesses such as acute glomerulonephritis, preeclampsia, and cocaine abuse. However, in
chronically hypertensive patients, either undiagnosed or inadequately controlled, the autoregulatory range is shifted to the right from arteriolar smooth muscle hypertrophy. This hypertrophy minimizes the transmission of pressure to the capillary bed, allowing tissue tolerance of higher blood pressures, but at the same time places the patient at risk for hypoperfusion if treated to normotensive pressures (
Fig. 35.1).
This is the reason that blood pressure should not be reduced too quickly in chronically hypertensive patients since this will result in relative hypotension causing tissue hypoperfusion. Gradual reduction in blood pressure allows the rightward-shifted autoregulatory curve to normalize as the arteriolar hypertrophy slowly regresses. Treatment must be tempered by the fact that
abrupt overzealous blood pressure reduction may lead to hypoperfusion and ischemia, with potential for irreversible neurologic damage. Cerebrovascular accidents, blindness, paralysis, coma, myocardial
infarction (MI), and death have been reported as consequences of overaggressive blood pressure reduction.
B. Endothelial damage. Hypertensive emergencies are triggered by an abrupt increase in systemic vascular resistance (SVR) caused by elevated levels of circulating vasoconstrictors (e.g., norepinephrine and angiotensin II). The resultant increase in blood pressure leads to arteriolar fibrinoid necrosis and endothelial damage. This endothelial damage is the etiology of the loss of autoregulatory function. In addition, the necrotic fibrinoid debris causes narrowing and obliteration of the vascular lumen. Target organ dysfunction ensuing from these two processes causes further release of vasoactive substances, producing a cycle of increasing SVR, elevated systemic blood pressure, vascular injury, and tissue damage. This is the vicious cycle that propagates the hypertensive emergency.
C. Manifestations. The endothelial damage and escape from autoregulatory control during a hypertensive crisis leads to the classic acute end-organ complications. Because the brain is encased in a finite space in the skull, the excess blood flow results in cerebral edema and elevated intracranial pressure (ICP), leading to encephalopathy and seizures. In the kidney, the fibrinoid necrosis as well as the excess blood flow destroy glomeruli, resulting in proteinuria, hematuria, and acute renal failure. The acute injury to the fundi is manifested by exudates, hemorrhage, papilledema, and potentially blindness. The cardiovascular system can suffer from myocardial ischemia and pulmonary edema from the increased afterload state as well as aortic dissection and hemolysis from the shear stress.
III. ETIOLOGY.
It is estimated that 30% to 40% of patients with a hypertensive crisis have an identifiable underlying cause compared with < 5% of those with hypertension who have not had a crisis. Evaluation for such secondary causes and precipitants is indicated in all patients with a hypertensive crisis.
A. A common scenario is that of a patient inadequately treated for chronic hypertension or one that is medically nonadherent.
B. Risk factors for progression to hypertensive crisis include male gender, black race, low socioeconomic status, cigarette smoking or other tobacco abuse, and oral contraceptive use. Unlike primary hypertension, the incidence of which increases with age, the peak incidence of hypertensive crisis occurs among people aged 40 to 50 years.
C. Underlying pathologic states that can precipitate hypertensive crises include renal parenchymal disease, renovascular hypertension, collagen vascular disease and scleroderma, pheochromocytoma, vasculitis, preeclampsia, and neurologic disorders (
Table 35.2).
D. A number of medications and illicit drugs can cause marked elevations in systemic blood pressure. The most common offenders are cocaine, oral contraceptives, sympathomimetic agents (e.g., diet pills and amphetamines), cold remedies (especially pseudoephedrine), nonsteroidal anti-inflammatory drugs (NSAIDs), tricyclic antidepressants, and monoamine oxidase inhibitors. Withdrawal from medications and illicit drugs can also precipitate severe hypertension. Examples include alcohol, benzodiazepine, and clonidine withdrawal.
IV. CLINICAL PRESENTATION
A. History
1. Symptoms. The history should focus on the organs that are known to suffer from end-organ damage: cardiovascular, neurologic, renal, and ocular. Cardiopulmonary symptoms include shortness of breath and chest pain. Neurologic symptoms include headache, confusion, lethargy, altered mental status, nausea, and vomiting. Oliguria and change in urine color to suggest hematuria may be the symptoms volunteered by the patient if there is renal damage. Blurred vision or change in vision suggests ocular involvement.
2. Symptom chronology. Among patients with severe hypertension, symptom chronology and the duration of uncontrolled blood pressure should be elicited, as this will guide the aggressiveness of blood pressure control.
3. History of hypertension. Most patients with hypertensive crises have an underlying history of chronic primary hypertension; however, a significant proportion have secondary forms of hypertension. Age of onset of hypertension as well as other potential clues to a secondary form of hypertension should be assessed.
4. Contributory medication history may include NSAIDs, oral contraceptives, erythropoietin, psychotropic agents, monoamine oxidase inhibitors, ephedrine, cyclosporine, tacrolimus, over-the-counter cold remedies, and many other medications. Withdrawal from clonidine is always a risk factor for a crisis in hypertensive patients to whom this medication has been previously prescribed. For those on antihypertensive medications it is crucial to elicit administration history, as a frequent, and potentially catastrophic, complication occurs when severe hypotension is induced by initiation of all outpatient medications in a patient with nonadherence.
5. History of use of recreational drugs such as cocaine and amphetamines, nonprescription stimulants including sympathomimetic weight loss pills, and performance-enhancing substances for athletes is important to elicit.
6. Smoking history. Smokers are at increased risk for progression to severe hypertension, perhaps due to endothelial dysfunction and dysfunctional autoregulation.
B. Physical findings
1. Vital signs. Blood pressure is measured in both upper and lower extremities to evaluate for stenosis or dissection of the aorta or great vessels. Severe hypertension is confirmed by taking two blood pressure measurements separated by 15 to 30 minutes. No absolute level of blood pressure differentiates an emergency from an urgency. The distinction is based upon the assessment of acute end-organ damage.
2. Optic fundi are examined for signs of retinopathy, including exudates, hemorrhages, or papilledema.
3. Neurologic assessment is performed to assess mental status and neurologic motor deficits. Patients with hypertensive encephalopathy may manifest neurologic signs of confusion or seizure activity.
4. Cardiovascular and pulmonary systems are examined for the presence of an S3, S4, new murmur, and/or pulmonary edema. Total volume status should be assessed, as certain treatments can cause severe hypotension in the setting of volume depletion and other medications are less effective in the setting of fluid overload.
5. Vascular system is examined by palpation of pulses and auscultation for bruits, especially renal bruits.