Hypertension
Michael A. Weber
Hypertension is the most common chronic condition dealt with by physicians in the United States. Even so, there is no agreement on a straightforward and accurate way to describe it. Most directly, hypertension could simply be described as the clinical finding of high blood pressure, but most experts now recognize that hypertension often is part of a complex set of cardiovascular, renal, and metabolic abnormalities. There is a great deal of variability in the phenotypic characteristics of hypertension, suggesting that high blood pressure may be a reflection of differing underlying abnormalities. On the positive side, the creation of effective pharmacologic and lifestyle strategies for reducing blood pressure has at least provided dependable tools for clinicians to manage hypertension and improve patient outcomes in their practices.
History
Over 4,000 years ago observers noted that the finding of a hard pulse, particularly in older people, was indicative of a poor prognosis (1). Perhaps the real origin of hypertension as a contemporary condition was the report by Bright in 1836 that patients with renal disease tended to suffer from major cardiovascular events and often died from strokes (2). To this day, the powerful connection between the kidney and the circulation, presumably mediated by high blood pressure and the activation of mechanisms such as the renin-angiotensin system, remains a fundamental part of our understanding of hypertension. The work by Korotkoff in the early part of the 20th century showing how vascular sounds are indicative of blood pressure values helped lead to practical methods for clinicians to measure blood pressure routinely (3).
In what is now becoming a familiar paradigm for medical progress, the next two major developments came from industry. The first came from the life insurance industry when the Actuarial Society of America reported the close relationship between blood pressure measurements and life expectancy (4). In some ways, these data, published over 80 years ago, provide the rationale for our current aggressive approach to managing hypertension. This approach, though, could not have been possible without the second contribution from industry, in particular the discovery of pharmacologic agents that could effectively reduce blood pressure in the clinical setting.
Among the earliest antihypertensive drugs were the diuretics, which first became available in the 1950s and are still indispensable. Much of our progress in treating hypertension during the past 50 years has depended on the progressive development of newer, more selective drugs that have expanded efficacy as well as becoming progressively more tolerable to patients. A brief but delightful summary of this fascinating process has been published recently (5). It is noteworthy that the writer of that review (Dr. Edward Freis) contributed in a meaningful fashion to the history of hypertension by reporting in 1967 on the first clinical trial in which drug treatment of hypertension, as compared with placebo, significantly reduced the incidence of major cardiovascular events and death (6).
Definitions
Hypertension can be defined in different fashions. First of all, it can be described almost entirely in terms of blood pressure; then, it can be defined as part of a syndrome of cardiovascular risk factors, including high blood pressure, and by evidence for underlying vascular abnormalities; and finally, it can be regarded empirically as a high-risk condition in which cardiovascular prognosis can be improved by the application of appropriate therapies.
The Blood Pressure Approach
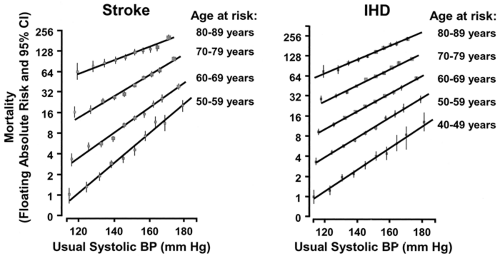
Since the early actuarial data that showed the connection between blood pressure and cardiovascular events, prospective clinical observations have continued to support the importance of this relationship. For instance, long-term follow-up of a large cohort of young and middle-age men recruited for a study
known as the Multiple Risk Factor Intervention Trial has shown that both systolic and diastolic blood pressures were highly predictive of subsequent strokes and cardiovascular outcomes (7). A particularly powerful observation, based on a meta-analysis of a million people, has defined the link between blood pressure and major outcomes in a precise fashion (8). As shown in Figure 25-1, regardless of age, blood pressure is clearly a major determinant of coronary and stroke mortality. For every 20 mm Hg increment in systolic blood pressure there is approximately a doubling of the risk of events. When considered on a population basis, blood pressure differences of only 1 mm Hg multiply out into meaningful effects on clinical outcomes. Using these same data (8), it has been stressed that age is also a major determinant of outcomes (9).
known as the Multiple Risk Factor Intervention Trial has shown that both systolic and diastolic blood pressures were highly predictive of subsequent strokes and cardiovascular outcomes (7). A particularly powerful observation, based on a meta-analysis of a million people, has defined the link between blood pressure and major outcomes in a precise fashion (8). As shown in Figure 25-1, regardless of age, blood pressure is clearly a major determinant of coronary and stroke mortality. For every 20 mm Hg increment in systolic blood pressure there is approximately a doubling of the risk of events. When considered on a population basis, blood pressure differences of only 1 mm Hg multiply out into meaningful effects on clinical outcomes. Using these same data (8), it has been stressed that age is also a major determinant of outcomes (9).
Clinical trials that have studied the importance of reducing blood pressure in high-risk hypertension have arrived at similar conclusions. For instance, in the Hypertension Optimal Treatment (HOT) trial (10), hypertensive patients treated with more-aggressive as compared with less-aggressive blood pressure-lowering therapy—particularly if they were also diabetic—had significantly fewer clinical events. Likewise, in the United Kingdom Prospective Diabetes Study (11), tighter as compared with less-tight control of blood pressure was significantly more effective at preventing cardiovascular and diabetic clinical endpoints. Indeed, meta-analysis of hypertension clinical trials in general could lead to the conclusion that the clinical effects of antihypertensive therapy could be explained mainly by the effects on blood pressure (12).
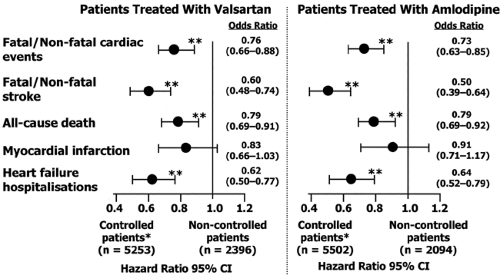
Most recently, the clinical effects of achieving a systolic blood pressure goal of less than 140 mm Hg were examined in the Valsartan (VALUE) trial (13). For treatments based on either valsartan or amlodipine, as shown in Figure 25-2, achieving this treatment goal—regardless of the drug regimen used—sharply reduced the incidence of cardiac events, stroke, and mortality.
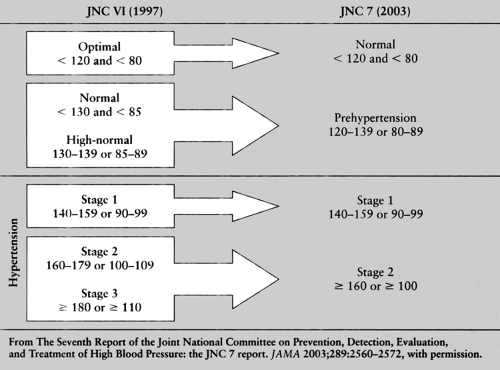
Largely for these reasons, the most recent report of the Joint National Committee on the Prevention, Detection and Treatment of High Blood Pressure (JNC 7) has taken very much a blood pressure-focused approach toward defining and caring for hypertension (14). The criteria recommended by this committee are summarized in Table 25-1 and should be considered carefully.
Staging of Hypertension
The JNC has recommended that a diagnosis of hypertension should be made when blood pressure is 140/90 mm Hg or higher. As long as either the systolic or diastolic criterion is met, the diagnosis is established. Hypertensive patients whose blood pressures are below 160/100 mm Hg are classified as Stage 1, whereas those at or above this level are classified as Stage 2. As discussed later, this has implications for how treatment should be started. It is noteworthy that the diagnosis and decision to treat are in general not affected by the age, other demographic features, or comorbidities of patients. Blood pressure, by and large, is the predominant criterion. The main exception to the 140/90 mm Hg threshold is for patients with diabetes or chronic kidney disease, in whom the diagnosis should be made and treatment begun if blood pressure is 130/80 mm Hg or higher.
This apparently simplistic approach does not mean that the JNC failed to recognize the important effects on global cardiovascular risk of the multiple cardiovascular findings that often accompany high blood pressure. Rather, it indicates the belief by the JNC that because hypertension generally is not well managed, and that a disturbingly large number of hypertensive patients are either not being treated or are being treated inadequately, straightforward recommendations based on blood pressures alone are most likely to be understood and lead to action by the clinical community. It should also be noted that the goal of treatment for most patients is to reduce their blood
pressures to below 140/90 mm Hg, and in the case of those with diabetes or chronic kidney disease, below 130/80 mm Hg.
pressures to below 140/90 mm Hg, and in the case of those with diabetes or chronic kidney disease, below 130/80 mm Hg.
Why did the JNC choose these particular blood pressure criteria? After all, as shown in Figure 25-1, it is evident that prognosis is progressively better at levels of systolic blood pressure down to 115 mm Hg, or possibly even lower. Why, then, choose 140 mm Hg as a diagnostic criterion? Briefly, the JNC was guided by published evidence of clinical trials in which antihypertensive therapy reduced clinical events. However, most of this evidence so far has come from trials that used treatment criteria of around 140/90 mm Hg as their therapeutic blood pressure targets. Certainly, as shown in Figure 25-2, achieving a systolic goal of less than 140 mm Hg is associated with dramatic reductions in clinical events (13). Tempting as it may be to aim even lower, we still await clinical trial evidence that doing so will actually improve outcomes in hypertensive patients.
As an interim concept, the JNC (as shown in Table 25-1) has suggested the use of a category called prehypertension encompassing those patients with blood pressures between 120/80 and 139/89 mm Hg. And although not recommending treatment for such individuals (unless they are diabetic patients with renal disease) with therapeutic agents, they suggest the use of lifestyle modifications that could at least slow down the usual age-related increases in blood pressure and delay the onset of clinical hypertension.
The Risk Factor Approach and the Metabolic Syndrome
Hypertension commonly clusters with other cardiovascular risk factors, including lipid abnormalities, glucose intolerance, and obesity. This is sometimes referred to in terms such as the metabolic syndrome, syndrome X, and the hypertension syndrome (15). None of these descriptions is entirely satisfactory, for there is variability in the clinical picture. Moreover, because evidence for cardiovascular and renal changes are often part of this constellation of findings, limited terms such as “metabolic” do not really suffice.
It is interesting to note that evidence for this constellation of findings can appear early in life. It has been shown, for instance, that normotensive offspring of parents with hypertension can already exhibit evidence for early changes in metabolic findings and in such characteristics as microalbuminuria, early changes in the structure and function of the left ventricle, and stiffening of the arteries (15). It is not entirely certain whether these familial findings reflect a genetic tendency or simply the effects of a commonly shared environment. It should also be pointed out that because the definition of the metabolic syndrome is arbitrary (15), it may not truly represent a syndrome with a single underlying etiology (16).
Despite these controversies, there is no doubt that a number of metabolic, cardiovascular, and renal changes are commonly associated with hypertension and almost certainly affect total cardiovascular risk in such individuals. The official guidelines of the European Society of Hypertension (ESH) (17) differ quite sharply from the JNC guidelines in taking these comorbidities into account. Put simply, the European guidelines advocate earlier and more aggressive therapy in hypertensive patients who have concomitant risk factors, even if blood pressure is only modestly elevated and, at the same time, would allow a more deliberative and protracted period of observation before starting treatment in hypertensive patients who do not exhibit other risk factors.
One thing is clear. All the guidelines committees agree that every patient should be evaluated for all known cardiovascular risk factors, and when found, these risk factors should be dealt with in an effective fashion. One important example of this approach: there is compelling evidence that the use of statin therapy in hypertensive patients, even when their low-density lipoproteins (LDL) cholesterol levels do not reach the traditional criteria for such therapy, still contributes meaningful additional reductions in cardiovascular outcomes (18).
A More Fundamental Definition
A working group of the American Society of Hypertension has published a position paper on the definition of hypertension (19). The approach suggested in this report, as summarized in Table 25-2, is less empirical than those encompassed by the
JNC (14) or the ESH (17) and goes beyond the blood pressure and other clinical findings that characterize those definitions. Instead, this more fundamental paradigm sees hypertension as a disease affecting the structure and function of arteries and myocardium, together with other underlying abnormalities of renal and neuroendocrine mechanisms. In this construct of hypertension, clearly there is a heterogeneity of causes leading to the high blood pressure and an assumption that high blood pressure—although important—should also be interpreted as a diagnostic sign of underlying abnormalities.
JNC (14) or the ESH (17) and goes beyond the blood pressure and other clinical findings that characterize those definitions. Instead, this more fundamental paradigm sees hypertension as a disease affecting the structure and function of arteries and myocardium, together with other underlying abnormalities of renal and neuroendocrine mechanisms. In this construct of hypertension, clearly there is a heterogeneity of causes leading to the high blood pressure and an assumption that high blood pressure—although important—should also be interpreted as a diagnostic sign of underlying abnormalities.
Table 25-2. The Proposed Classification of Hypertension by a Working Group of the American Society of Hypertension that, in Addition to Blood Pressure Levels, Takes into Account Concomitant Risk Factors as Well as Evidence for Cardiovascular Structural or Functional Changes in Determining the Status of Hypertensive Patients | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||
There is good clinical evidence to support this protean view. Hypertensive patients can be differentiated on the basis of such phenotypes as their renin measurements, their age, and their body mass, and also by variations in the structure and function of such organs as the cardiac left ventricle, the degree of stiffness of small and large arteries, and characteristics of renal function (20). From a practical point of view, this definition does not provide the simplicity of the previous guidelines. On the other hand, this preliminary work sets the stage for anticipating that hypertension ultimately will be regarded as a set of varying conditions that, once carefully described, might respond optimally to different therapeutic strategies.
Evaluation of the Hypertensive Patient
Evaluating and diagnosing a person who might have hypertension, though relatively straightforward, has lifelong implications for the patient. In general, an elevated blood pressure is all that is required to make a diagnosis, but the impact is considerable: quite apart from the costs and inconveniences of regular visits to clinicians, making lifestyle changes, and taking medications, there is also the issue of labeling a person with a lifelong diagnosis. In explaining to patients that they have hypertension, clinicians must describe cardiovascular events, strokes, and other serious outcomes that can result if the hypertension is not well treated. For many patients, this will be the first time that such serious events have been raised in the context of their own lives. So it is also critical to provide encouragement that this diagnosis should not affect their long-term outlook provided they make a sensible commitment to their own care. Because the published guidelines provide excellent detailed information on the comprehensive evaluation of hypertensive patients, only some brief comments are made here.
Measuring the Blood Pressure
In making a diagnosis of hypertension, the blood pressure readings should be confirmed on two or three occasions, preferably some days apart. Details of appropriate techniques are described in the guidelines (14). Some experts advocate the use of ambulatory blood pressure monitoring for patients in whom white coat hypertension—blood pressure that is high in the clinical setting but is normal at most other times—is suspected. This can be a useful test, though if other clinical findings provide an incentive to hypertensive therapy, particularly other risk factors or evidence for cardiovascular or renal changes, then it is probably not necessary to perform ambulatory monitoring to confirm the diagnosis. Home blood pressure readings by patients are interesting, but it should be remembered that typically blood pressures at home are lower than in the office because they are often taken at times of day when blood pressures are expected to be relatively low. It should also be remembered that our knowledge of the prognosis of hypertension is based on readings obtained in the clinical setting.
Laboratory and Other Tests
Because high blood pressure is often associated with other risk factors, laboratory studies should be carried out to evaluate findings such as lipids, glucose, electrolytes, renal function, and liver function. Fasting values should be used because they help in the diagnosis of diabetes and in calculating the lipid profile. Because it is an important predictive factor, microalbuminuria should be looked for; and likewise an electrocardiogram (or echocardiogram if feasible) should be performed to check for left ventricular hypertrophy or other evidence of cardiac involvement. All these tests are relevant because they can dictate the selection of antihypertensive drugs. Fuller recommendations can be found in published guidelines (14,17).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree