46 Hypertension
Hypertension is a major risk factor for atherosclerotic cardiovascular disease (Box 46-1). Despite advances in the understanding of the pathophysiology, epidemiology, and natural history of hypertension, as well as improvements in therapy, many patients with hypertension are undiagnosed or inadequately treated. Hypertension, or high blood pressure (BP), remains an important contributor to coronary events, heart failure, stroke, and end-stage kidney disease.
Box 46-1 Hypertension as a Risk Factor for Cardiovascular Disease
BP is a continuous variable, and any BP level chosen to define hypertension is arbitrary. Nevertheless, an operational definition of hypertension has been advocated as a treatment guideline. The Seventh Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) recommended the classification of BP for adults shown in Table 46-1.
Table 46-1 Classification of Blood Pressure for Adults Aged 18 Years and Older
| Category | Systolic (mm Hg) | Diastolic (mm Hg) |
|---|---|---|
| Normal | <120 | <80 |
| Pre-hypertension | 120–139 | 80–89 |
| Hypertension | ||
| Stage 1 | 140–159 | 90–99 |
| Stage 2 | ≥160 | ≥100 |
With permission from Chobanian VA, Bakris GL, Black AR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report. JAMA. 2003;289:2560–2572.
Etiology and Pathogenesis
Hypertension is a disorder of BP regulation that results from an increase in cardiac output or, most often, an increase in total peripheral vascular resistance. Cardiac output is usually normal in essential hypertension, although increased cardiac output plays an etiologic role. The phenomenon of autoregulation explains that an increase in cardiac output causes persistently elevated peripheral vascular resistance, with a resulting return of cardiac output to normal. Figure 46-1 shows mechanisms that can cause hypertension. Inappropriate activation of the renin-angiotensin system, decreased renal sodium excretion, and increased sympathetic nervous system activity, individually or in combination, are probably involved in the pathogenesis of all types of hypertension. Hypertension also has genetic and environmental causes, the latter including excess sodium intake, obesity, and stress. The inability of the kidney to optimally excrete sodium, and thus regulate plasma volume, leads to a persistent increase in BP whatever the etiology.
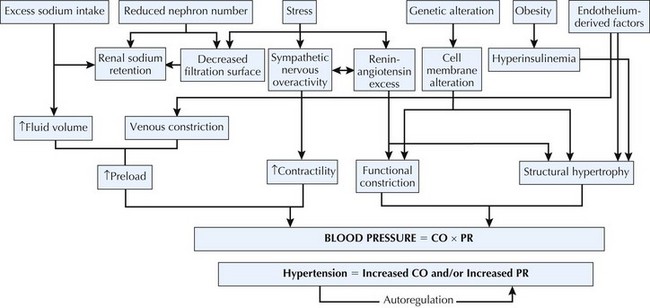
Figure 46-1 Factors involved in the control of blood pressure.
CO, cardiac output; PR, peripheral resistance.
With permission from Kaplan NM. Kaplan’s Clinical Hypertension. 8th ed. Philadelphia: Lippincott Williams & Wilkins; 2002.
Clinical Presentation
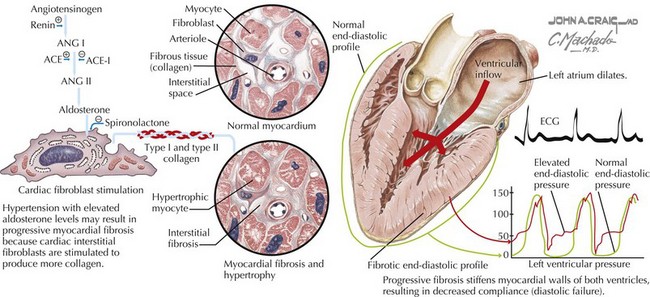
Increased ventricular afterload resulting from elevated peripheral vascular resistance and arterial stiffness is considered the principal determinant of myocardial hypertrophy in patients with hypertension. Hemodynamic overload stimulates increases in myocyte size and the synthesis of contractile elements. Fibroblast proliferation and deposition of extracellular collagen accompany these cellular changes and contribute to ventricular stiffness and myocardial ischemia. A growing body of evidence suggests that angiotensin II and aldosterone, independent of pressure overload, stimulate this interstitial fibrosis (Fig. 46-2).
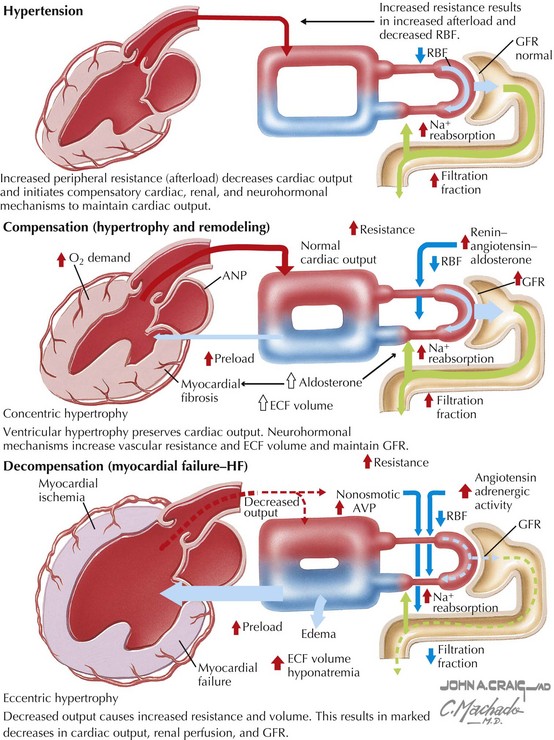
Clinical consequences of hypertensive heart disease include heart failure and coronary heart disease (CHD). More than 90% of patients with heart failure have hypertension, and data from the Framingham Heart Study suggest that high BP accounts for almost half of the population burden of this disorder. Treating hypertension reduces the risk of heart failure by nearly 50%. Heart failure develops because of the myocyte hypertrophy and ventricular fibrosis that characterize hypertensive LVH. As illustrated in Figure 46-3, the early functional manifestations of LVH include impaired LV relaxation and decreased LV compliance. Although the ejection fraction is preserved initially, diastolic dysfunction often results in increased filling pressures, leading to pulmonary congestion. This mechanism accounts for the symptoms observed in approximately 40% of hypertensive patients with heart failure. If excessive BP levels persist, myocyte loss and fibrosis contribute to ventricular remodeling and contractile dysfunction. Compensatory mechanisms, including remodeling of the peripheral vasculature and activation of the sympathetic nervous and renin-angiotensin systems, accelerate the deterioration in myocardial contractility. Ultimately, decompensated cardiomyopathy and heart failure from systolic dysfunction develop (Fig. 46-4).
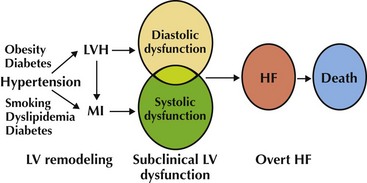
Figure 46-4 The development of heart failure (HF) in patients with hypertension.
LV, left ventricular; LVH, left ventricular hypertrophy; MI, myocardial infarction.
Adapted from Vasan RS, Levy D. The role of hypertension in the pathogenesis of heart failure. A clinical mechanistic overview. Arch Intern Med, 1996:156:1789–1796.
Differential Diagnosis
Approximately 95% of patients with elevated arterial pressure have hypertension of unknown etiology, known as essential hypertension. The remaining 5% have an identifiable cause of secondary hypertension (Box 46-2). Although relatively few patients have secondary hypertension, identification of these patients is important, because the hypertension can often be cured or significantly ameliorated by an interventional procedure, a specific drug therapy, or stopping a culprit drug.
Identifiable causes of hypertension should be sought in the initial history, physical examination, and laboratory studies. Further diagnostic evaluation for secondary hypertension causes is pursued when the presentation is atypical for essential hypertension or when the initial evaluation suggests an identifiable cause (Box 46-3).