Fig. 40.1
Adult patient with a proximal LPA stenosis (a, b) undergoing hybrid stent therapy using an endoscopic approach with direct visualization, as well as surgical pulmonary valve replacement. Image (c) documents the ridge/kink (arrow) at the proximal LPA while image (d) documents the same lesion after placement of an intraoperative stent
Using previous imaging data, stent and balloon choices should be made in advance to intraoperative stent placement, and the chosen diameter is additionally evaluated intraoperatively using a variety of Hagar dilators. Endoscopic guidance is extremely helpful in aiding stent delivery (Fig. 40.2). Once the vessel is exposed, the endoscope is advanced until the first side branch is visualized, thereby obtaining a good estimate of the maximum length to avoid jailing of those side branches. In addition, the endoscope can facilitate advancing a wire into the correct vessel, rather than mistakenly entering a smaller side branch distally. Soft wires are preferable and stiff wires as well as long sheaths are not required. Prepping the stent on the balloon should be performed in standard technique, even though elimination of all air or the use of contrast in the balloon is not quite as important as during percutaneous stent delivery. In small patients, if a stent that can be expanded to adult size is too long, it can be shortened during the procedure using standard sterilized wire cutters or strong scissors. Importantly though, this should only be performed for closed-cell design stents, as cutting or shortening open-cell design stents can be associated with a loss of stent integrity and radial strength. Once a wire has been placed in appropriate position, the balloon/stent is advanced over the wire and positioned by visualizing the proximal end of the stenotic lesion. If there are any concerns about wire or balloon positioning, it can be helpful to use a C-arm during stent expansion as this will show if a stent expands unequally or if the balloon/stent may be trapped in a smaller distal vessel. Once the stent is fully expanded, the endoscope is utilized to evaluate the entire stent position and stent lumen (Fig. 40.1). Any struts that expand beyond the proximal end of the vascular lesion can be folded over by the surgeon using some stronger pickups, thereby creating a smooth adherence of the struts to the vessel wall (Fig. 40.3). In addition to visual and endoscopic inspection, it is desirable to perform an exit angiography at the end of the procedure to evaluate the results of stent placement angiographically.
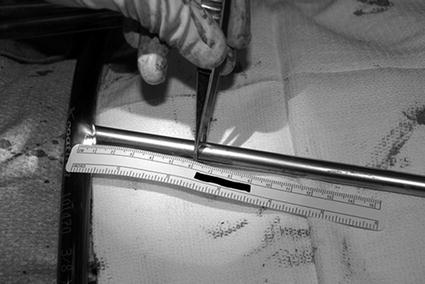
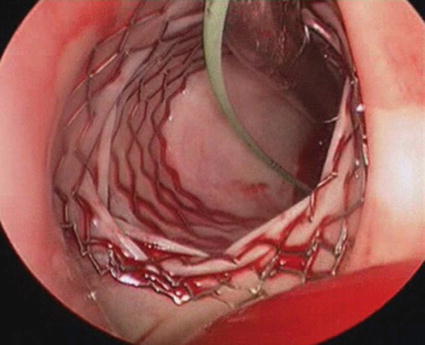
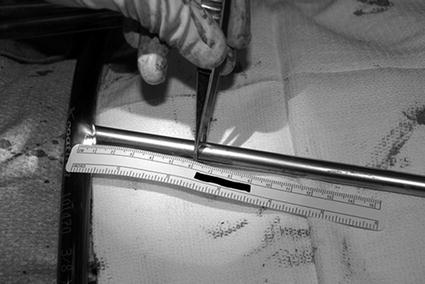
Fig. 40.2
Endoscope used during intraoperative stent placement via direct visualization. The endoscope facilitates imaging of the side branches distal to the stenotic lesion and allows estimate of the distance to those branches
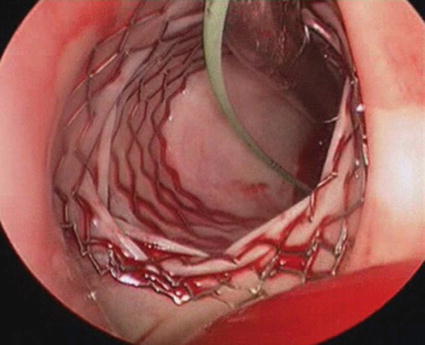
Fig. 40.3
Stent positioned in proximal LPA using direct visualization with endoscopy. Note the folded meshwork of the stent that is bent over the proximal LPA ridge to create a smooth entry site into the LPA
40.3 Hybrid Stent Delivery Using Angiographic Guidance
Hybrid stent therapy using angiographic guidance is less commonly performed than direct visualization with endoscopic guidance. This technique is usually reserved for patients where a percutaneous transcatheter approach has not been successful in treating a specific vascular lesion or where there is very little opportunity for direct visualization, such as residual arch obstructions identified during exit angiography after a comprehensive arch repair (Fig. 40.4). In addition, angiographic guidance is advantageous in patients where there is very little preexisting imaging data or in smaller vascular structures, where the use of endoscopy would not be feasible in evaluating the distal vessel. Furthermore, this approach is beneficial in critically ill postoperative patients where a longer percutaneous procedure may not be well tolerated, especially if stents are desired that can be expanded to adult size, which would require larger delivery sheaths and stiffer wires. A direct approach in these patients avoids the use of stiff wires and long sheaths and is hemodynamically often a lot better tolerated. In addition, if there are concerns of creating vascular injury in a freshly dissected vessel in a postoperative patient, performing this procedure with an open chest and cardiopulmonary bypass on standby provides an additional safety net.
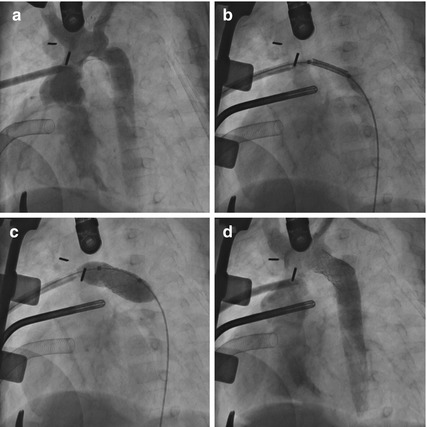




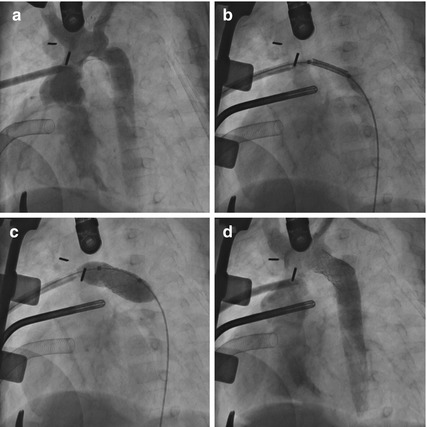
Fig. 40.4
Six-months-old infant with hypoplastic left heart syndrome undergoing a bidirectional Glenn procedure. There was a preexisting concern about an arch obstruction. Intraoperative angiography (a) documented a narrowing distal to the left subclavian artery. An intraoperative stent was placed through a sheath that was advanced over a wire through a purse string in the ascending aorta. (b) Stent positioning, (c) stent expansion, and (d) final angiogram
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


