Date of birth
Explanation and
Consent
“Could we have a little chat about what’s brought you in today?”
2.2 History taking
2.2.1 Presenting complaint
Use open questions to start the consultation.
Obtain nature and duration of complaint.
2.2.2 History of presenting complaint
There are six cardinal symptoms in Cardiology.
1. | Chest pain “SOCRATES” | |
Site | “Where is the pain?” | |
Onset | “How did it come on?” | |
Character | “Can you describe the pain?” | |
Radiation | “Does the pain go anywhere else?” | |
Associated features | “Does it come on with other symptoms?” | |
Time course | “How long does each episode last for?” | |
Exacerbating/relieving factors | “Does anything make it better or worse?” | |
Severity score | “On a scale of 1–10, how bad is the pain?” | |
2. | Shortness of breath (SOB) | |
Dyspnoea | ||
Exercise tolerance, including stairs and hills | Use a local example “How far along Frederick Street can you walk without stopping?” | |
Rule out other causes for exercise intolerance | e.g. Osteoarthritis, chest pain, dizziness | |
Effect of activities of daily living | “Has the breathlessness affected your daily routine?” | |
Orthopnoea | ||
No. of pillows used and why | “How many pillows do you use? Is X number of pillows normal for you?” | |
Paroxysmal nocturnal dyspnoea | ||
Frequency | “Have you ever found yourself waking up in the middle of the night, coughing and trying to catch your breath?” | |
Effect on sleep, daytime activities | ||
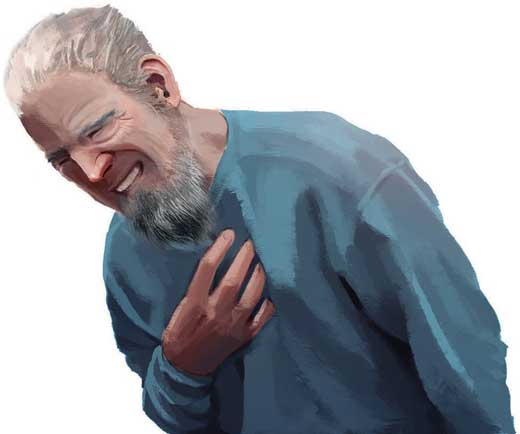
Figure 2.1 – Chest pain (Levine’s sign).
3. | Claudication | |
Location | “Where is the pain?” (Bilateral or unilateral; thigh, buttocks, calf) | |
Distance covered | “How far can you walk before needing to rest?” | |
Rule out other causes of stopping and effects on activities of daily living
4. | Syncope | |
Rule out epilepsy by asking (in addition to core questions)
| ||
If possible, obtain collateral history | ||
5. | Palpitations | |
Rhythm | Ask the patient to tap out the rhythm | |
Effect on activities | “Does it stop you from doing anything?” | |
Frequency and duration of episodes | “How often do you get this symptom and how long do they last for?” | |
Associated symptoms and triggers | ||
6. | Ankle (peripheral) oedema | |
Extent of swelling | “How far does the fluid spread along?” | |
Weight change | “Have you lost or gained weight recently?” | |
2.2.3 Past medical history
Acute hospital admissions (duration, reason).
Medical or surgical intervention received (CABG, PCI, AVR, pacemakers, etc.).
Don’t forget to check for thyroid disease (e.g. atrial fibrillation associated with hyperthyroidism).
Ask specifically about cardiovascular risk factors:
Non-modifiable | Modifiable |
Age | Hypertension (most common risk factor) |
Male gender | Diabetes mellitus (worst risk factor) |
Family history of cardiovascular disease | Smoking |
2.2.4 Drug history
- Ask about regular medications and allergies
- Specific drugs to be aware of
- digoxin – can cause digitalis toxicity
- amiodarone – can cause pulmonary fibrosis, thyroid disease, corneal deposits, skin discoloration
- adriamycin/doxorubicin – chemotherapeutic agents known to cause cardiotoxicity
- tricyclic antidepressants – can precipitate arrhythmias and prolong QT interval
- drugs that can prolong QT interval (refer to Chapter 4).
- digoxin – can cause digitalis toxicity
2.2.5 Family history
- For first-degree relatives, enquire about age, current health or cause of death (if deceased)
- Enquire about specific cardiac family history (e.g. hyperlipidaemia, myocardial infarction).
2.2.6 Social history
Alcohol intake | Units per week ([volume of alcohol/L × ABV/%] × 7), pattern (binge/regular) |
Smoking | Per day, for how many years (pack years), any intention to stop, smoking cessation efforts |
Illicit drug use | Cocaine is a cause of coronary vasospasm and arrhythmia |
Travel | |
Occupation | Effect of symptoms on work |
Living conditions | Housing (stairs present?), family, carer support |
Diet, exercise levels and stress | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


