The relation between underlying ventricular morphology and regional function in patients with Fontan circulation remains unclear. The aim of this study was to compare regional function and its heterogeneity in patients with tricuspid atresia (TA), biventricular apex-forming morphology (BiV), and controls. Nineteen patients (median age 12 years) with Fontan circulation who presented consecutively were prospectively enrolled and compared with age- and heart rate–matched controls. Most patients were in New York Heart Association class I (63%). Longitudinal systolic strain (S), systolic strain rate (SR sys ), and early diastolic strain rate (SR dia ) peaks were obtained from 6 ventricular segments, and a coefficient of variation by segment was calculated as a measure of regional heterogeneity. Systolic S, SR sys and SR dia peaks were decreased at the right and left lateral walls in both patient groups compared with controls (p ≤0.001 for all). Patients with TA had higher systolic S and SR sys in the middle of the right lateral wall than those with BiV morphology (p = 0.009 and p = 0.001, respectively). The mean coefficients of variation assessed by S and SR sys were similar in controls and patients with TA but lower in those with BiV than in controls and patients with TA (p <0.001 and p = 0.01, respectively). The mean coefficient of variation assessed by SR dia was greater only in patients with BiV than in controls (p = 0.001). In conclusion, patients with Fontan circulation have more heterogenous systolic and early diastolic regional function than healthy control subjects, and patients with TA have better systolic regional function in the middle of the right lateral wall and less systolic heterogeneity than patients with BiV morphology.
Late morbidity and long-term survival remain problematic because of medical complications. Systolic and diastolic cardiac dysfunction might contribute to these unfavorable outcomes. Given the variety of ventricular anatomic arrangements in patients with functional univentricular hearts, follow-up monitoring would be facilitated by an effective, noninvasive approach for evaluating systolic and diastolic ventricular function. Conventional noninvasive imaging modalities are limited to the assessment of global univentricular function (e.g., the ejection fraction) in patients with Fontan circulation. The univentricular ejection fraction may decrease only at the end stage of heart failure. In contrast to the conventional echocardiographic assessment of the global univentricular function, novel echocardiographic strain and strain rate imaging modalities allow the quantitative evaluation of regional systolic and diastolic ventricular function of variable, complex anatomies, such as in patients with Fontan circulation. The heterogeneity of regional heart function has been assessed in other conditions. However, the heterogeneity of regional systolic and diastolic heart function in patients with Fontan circulation and its relation to ventricular morphology have remained unclear. Therefore, the goal of this prospectively designed study was to test the hypothesis that both patient groups have decreased regional ventricular function and greater functional heterogeneity than controls. Secondarily, we compared regional ventricular function between the two groups of Fontan patients to test the hypothesis that regional ventricular function and its heterogeneity would not differ between these patient groups.
Methods
We prospectively screened for study eligibility patients with Fontan circulation who routinely presented to the Berlin German Heart Institute from October 2003 through October 2005. We consecutively enrolled all eligible and consenting patients with normal ventricular D-loop and either tricuspid atresia (TA) or ventricular masses composed of 2 chambers that contribute to the apex (biventricular apex-forming morphology [BiV]; Supplementary Figure S1 ). We recruited healthy subjects matched by age and heart rate among healthy subjects who underwent examination in our outpatient clinic for heart murmurs or syncope and in whom structural cardiac lesions were ruled out using echocardiography. All patients and parents or guardians provided written informed consent. The study protocol was approved by the institutional ethics committee.
Using a commercially available echocardiography system (Vivid 7; GE Vingmed Ultrasound AS, Horten, Norway) equipped with a 2.5-MHz transducer, specifically trained cardiologists recorded standard views as described previously. We assessed the ratio of length of the rudimentary right ventricle to the total length of the right lateral free wall in the apical 4-chamber view in patients with TA at the end of diastole (the maximum ventricular chamber length); ( Supplementary Figure S2 ). For all routine clinical echocardiographic studies, ventricular function assessment included 2-dimensional imaging, color-flow Doppler, pulse-waved (PW) flow, and tissue Doppler imaging (TDI). The left ventricular ejection fraction was assessed using the 5/6 area-length method. The ejection fraction was calculated as (end-diastolic volume − end-systolic volume)/end-diastolic volume. The ejection fraction was considered normal for all study subjects ≥55%. The severity of mitral valve regurgitation was estimated by measurement of the vena contracta. Pulse-waved flow Doppler was recorded at the tip of the mitral leaflets to measure peak early filling (E-wave) velocity and peak atrial filling (A-wave) velocity and was used to extract the ratio of early to late diastolic flow velocity (E/A). Longitudinal systolic (S′), early (E′), and late diastolic (A′) velocity peaks were extracted using PW-TDI at the bases of the right and left lateral ventricular walls, and the E/E′ ratio was calculated using the mitral valve inflow E-wave and left lateral wall (E′). To assess global ventricular function, the Tei index was obtained ([isovolumic contraction + isovolumic relaxation time]/ejection time).
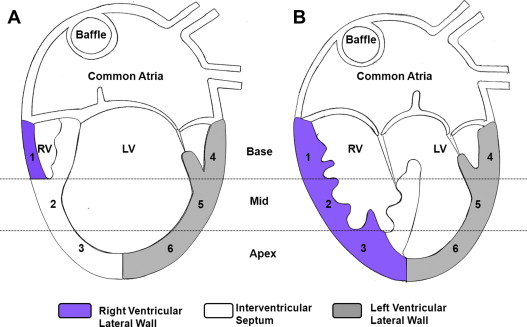
Real-time color TDI data were recorded from the right and left lateral walls using a standard apical 4-chamber view and digitally stored for off-line analysis to evaluate regional longitudinal function using strain and strain rate peaks. Because this method is angle dependent, care was taken to align the investigated myocardium and the ultrasound beam to nearly 0°. Longitudinal strain and strain rate peaks were extracted using dedicated software (EchoPAC; GE-Vingmed Ultrasound AS). Longitudinal systolic strain (S), systolic strain rate (SR sys ), and early diastolic strain rate (SR dia ) peaks were extracted for the basal, mid, and apical right and left lateral wall, as demonstrated in Figure 1 . We continuously positioned the region of interest within the interrogated segment using a semiautomated tracking algorithm and analyzed it as described previously. To minimize the effect of beat-to-beat variability on measured velocity and strain and strain rate peaks, 3 consecutive heart cycles were analyzed, and their mean was used in all analyses. The lead investigator processed data sets off-line and evaluated them in random order to avoid bias. To evaluate the heterogeneity of regional ventricular function, mean systolic S, SR sys , and SR dia peaks and their SDs for all 6 segments in the apical 4-chamber view were used.
The primary end points were S, SR sys , and SR dia in 6 segments. The secondary end points were PW-TDI derived velocities. Patient characteristics are summarized as median (range), number (percentage), or mean ± SD. All measurements are expressed as mean ± SD. Primary and secondary end points were compared with values in controls using the 1-sample unpaired Student’s t test. Bonferroni’s method was used to account for multiple comparisons. The p values for categorical data, such as New York Heart Association class, were calculated using Fisher’s exact test.
To summarize the heterogeneity of regional systolic and early diastolic function assessed by systolic S, SR sys , and SR dia in 6 segments, the coefficient of variation (CoV) was calculated for each segment as the ratio of SD to average in healthy controls and in patients. Then the mean CoV of all 6 segments was calculated for the primary end points. The mean CoV as a percentage was compared between study groups using the 1-sample unpaired Student’s t test. Bonferroni’s method was used to account for multiple comparisons, with a p value <0.017 for a significant difference for each comparison.
Pearson’s correlation coefficient was used to evaluate the association between systolic and diastolic mean CoV and Tei index and also systolic mean S, SR sys , and SR dia in all study subjects. Interobserver variability was quantified for the primary end point measure, systolic strain, using images from 13 randomly selected study patients and performed blinded by 2 investigators using Bland-Altman analysis for mean systolic strain values in the right and left lateral walls. Statistical analysis was performed using SPSS version 19 (SPSS, Inc., Chicago, Illinois). All statistical tests were 2 sided.
Results
Of 43 Fontan patients screened, 19 were eligible (median age, 12 years, range, 4 to 36), consented to be included in the study, and were enrolled. Ten of the 19 patients had TA and 9 had BiV ( Table 1 ). The surgical techniques for Fontan procedure were total cavopulmonary connection with extracardiac conduits in 9 patients with intra-atrial baffles in 8 patients and direct right atrial–to–pulmonary artery connection in 2 patients. The median duration from the Fontan procedure to study enrollment was 8 years (range, 2 to 15). Patients’ demographic and clinical characteristics variables are listed in Supplementary Table S1 . None of the demographic or clinical characteristics variables differed significantly between patient groups. The control population consisted of 19 subjects matched for age (median, 15 years, range, 5 to 36) and heart rate (mean, 75 ± 12 beats/min).
| Patient No. | Diagnosis | Great Arteries Relation | Segmental Approach | Pre-Fontan Procedures | PA Banding | Fontan Procedure Type | Age at Fontan (yrs) |
|---|---|---|---|---|---|---|---|
| 1 | TA and VSD (type I-C) | Normal | {S,D,S} | Modified BT shunt | No | TCPC intra | 14 |
| 2 | TA and PA (type I-A) | Normal | {S,D,S} | Modified BT shunt | No | TCPC intra | 3 |
| 3 | TA, VSD + PS (type I-B) | Normal | {S,D,S} | Waterston | No | TCPC intra | 18 |
| 4 | TA, VSD + PA (type III) | MGA | {S,D,L} | Modified BT shunt | No | RA–pulmonary artery | 19 |
| 5 | TA, VSD + PS (type I-B) | Normal | {S,D,S} | Glenn | No | TCPC extra | 2 |
| 6 | TA, PA (type I-A) | Normal | {S,D,S} | Modified BT shunt | No | TCPC extra | 1 |
| 7 | TA, VSD + PS (type I-B) | Normal | {S,D,S} | Modified BT shunt | No | TCPC extra | 5 |
| 8 | TA, PA (type I-A) | Normal | {S,D,S} | Modified BT shunt | No | TCPC intra | 5 |
| 9 | TA, PA (type I-A) | Normal | {S,D,S} | Modified BT shunt | No | RA–pulmonary artery | 16 |
| 10 | TA, VSD, (type III) | MGA | {S,D,L} | No | Yes | TCPC intra | 2 |
| 11 | CAVC, RVOTO | MGA | {S,D,L} | Modified BT shunt | No | TCPC extra | 2 |
| 12 | DORV, CAVC | d-TGA | {S,D,D} | No | No | TCPC extra | 28 |
| 13 | DORV | d-TGA | {S,D,D} | Modified BT shunt | No | TCPC extra | 4 |
| 14 | d-TGA, VSD, LVOTO | d-TGA | {S,D,D} | Modified BT shunt | No | TCPC intra | 12 |
| 15 | d-TGA, VSD, LVOTO | d-TGA | {S,D,D} | Modified BT shunt | No | TCPC extra | 2.5 |
| 16 | DILV | l-TGA | {S,D,L} | No | No | TCPC intra | 9 |
| 17 | DILV | d-TGA | {S,D,D} | Glenn | Yes | TCPC intra | 4 |
| 18 | DILV | d-TGA | {S,D,D} | Glenn | No | TCPC extra | 3 |
| 19 | DILV | d-TGA | {S,D,D} | No | No | TCPC extra | 4.5 |
In patients with TA with dominant left ventricles, the ratio of the length of the rudimentary right ventricle to the length of the entire right-sided lateral wall was 0.35 ± 0.02 (median, 0.35, range, 0.31 to 0.40), indicating that the rudimentary right ventricle represented approximately 1/3 of the total right lateral free wall. None of the patients had more than mild tricuspid or mitral valve regurgitation. The left ventricular ejection fraction was significantly lower in the Fontan circulation group compared with controls (51 ± 8% vs 62 ± 4%, p <0.001). In most patients (74% [14 of 19]), ventricular systolic function assessed by the ejection fraction was normal or mildly depressed. The ejection fraction was lower in the 2 groups of patients compared with controls and did not differ between TA and BiV patients ( Supplementary Table S2 ). Mitral valve inflow E wave and E/A ratio were significantly lower and E/E′ ratio was significantly elevated in both groups of patients compared with controls, and these measures also did not differ between TA and BiV patients ( Supplementary Table S2 ). Longitudinal S′ and E′ velocities at the right and left lateral walls were decreased and right lateral free wall A′ velocity was decreased in both patient groups in comparison with controls (p <0.001 for all) and again did not differ between TA and BiV patients. The Tei index was elevated in both patient groups compared with controls and did not differ between TA and BiV patients ( Supplementary Table S2 ).
Systolic S, SR sys , and SR dia were decreased at the right and left lateral walls in most ventricular segments in both patient groups in comparison with controls ( Supplementary Figure S3, Supplementary Table S3 ). Comparison analysis of all these measures between the patient groups showed significantly higher systolic S and SR sys in the right ventricular mid segment in patients with TA compared with those with BiV (−18 ± 4.3% vs −11 ± 4.4%, p = 0.009, and −1.5 ± 0.5 vs −0.7 ± 0.3 s −1 , p = 0.001, respectively). The TA and BiV patient groups had similarly decreased systolic mean S, SR sys , and SR dia measures in comparison with controls, but there was no difference between the two Fontan groups ( Supplementary Figure S4 ).
Segmental heterogeneity of systolic (S and SR sys ) and early diastolic (SR dia ) function assessed using the CoV in each segment varied more in both patient groups than in controls ( Figure 2 ). The heterogeneity of systolic function evaluated by the mean CoV of systolic S and SR sys was similar in patients with TA and controls but was greater in patients with BiV than in controls and in patients with TA (p <0.001 and p = 0.01, respectively; Figure 2 ). The mean CoV of SR dia was greater in patients with BiV morphology than in controls (p = 0.001; Figure 2 ), and both patient groups had significantly increased early diastolic heterogeneity compared with the control group.




