Fontan failure can occur even with normal systolic ventricular function and often in the context of significant liver disease. We hypothesized that Fontan failure is hemodynamically distinct from traditional heart failure and characterized by low systemic vascular resistance (SVR) index and preserved cardiac index. Twenty-seven symptomatic adult Fontan (SAF) patients who underwent catheterization from 2001 to 2011 constituted our study group. Fifty-four predominantly asymptomatic pediatric Fontan (PF) patients who underwent catheterization during the same period were randomly selected to perform a control:case cohort analysis. Clinical comparisons were made between the 2 groups. The adults were more symptomatic than the PF cohort (New York Heart Association classes I and II or III and IV: 48% or 52% [SAF] vs 94% or 6% [PF], respectively, p <0.01). SAF versus PF mean catheterization findings were central venous pressure 18 ± 6 versus 14 ± 3 mm Hg (p <0.01), SVR index 1,680 ± 368 versus 1,960 ± 550 dyn s/cm 5 /m 2 (p = 0.02), and cardiac index 2.7 ± 0.8 versus 2.8 ± 0.7 L/min/m 2 (p = 0.25). By imaging, the SAF cohort demonstrated a greater incidence of abnormal liver texture changes (96% vs 75%, p = 0.04) and nodularity (77% vs 42%, p = 0.02). In conclusion, adult patients with failing Fontan circulation had a lower SVR index and similar cardiac index compared with the pediatric cohort. Liver disease in the adults was more advanced. Our data suggest that Fontan failure is a distinct circulatory derangement with hemodynamic features similar to portal hypertension, albeit with limited ability to augment cardiac output.
Single ventricle palliation, culminating in the Fontan operation, has been described as a failed strategy in terms of long-term survival and quality of life. Among survivors, only 70% actuarial freedom from death or cardiac transplantation 25 years after Fontan palliation has been reported. “Fontan failure” is a term used to characterize much of the associated morbidity; however, it is itself variably defined. Descriptions include low cardiac output in the absence of ventricular failure, “myocardial failure”, and “death, (Fontan) takedown, transplantation, or New York Heart Association (NYHA) classes III and IV”. Depiction of the hemodynamic profile of Fontan failure has been similar to traditional heart failure: elevated central venous pressure, pulmonary capillary wedge pressure, and systemic vascular resistance (SVR), with a low cardiac index. However, clinical deterioration can occur in the absence of ventricular dysfunction, suggesting that distinct mechanisms are contributive. Based on the growing evidence of liver pathology in Fontan patients over time, we hypothesized that portal hypertension might play a significant role in failing Fontan pathophysiology. We sought to define the hemodynamic phenotype of patients with Fontan failure using catheterization data from symptomatic adult Fontan (SAF) patients and then compared our data with a pediatric Fontan (PF) cohort.
Methods
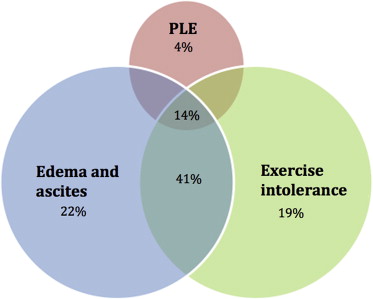
We performed a retrospective review of the Emory Adult Congenital Heart Center database for patients with the single ventricle physiology status after Fontan palliation who underwent a heart catheterization from January 2001 to December 2011. Surveillance catheterizations are not performed on all patients with Fontan palliation at our adult center and instead are done because of clinical deterioration. We defined clinical deterioration (Fontan failure) as development of significant symptoms such as refractory edema, ascites, protein-losing enteropathy, or considerable exercise intolerance, regardless of ventricular function. A total of 27 patients (NYHA functional classes III and IV: 52%) met the inclusion criteria. We also identified predominantly asymptomatic Fontan patients (NYHA functional classes I and II = 94%), aged 10 to 19 years, who had a catheterization performed during the study period. At our institution, catheterizations are routinely performed in PF patients at 10 and 15 years after the Fontan palliation. A total of 54 patients were randomly selected to perform a 2:1 control:case cohort analysis.
Clinical data, echocardiograms, catheterization findings, and liver imaging were compared between the SAF and PF cohorts. Echocardiogram interpretations are those of the attending cardiologist, with the evaluation of ventricular function accomplished by subjective assessment, modified Simpson’s method, and triplane 3-dimensional reconstruction. Cardiac catheterizations were performed using local anesthesia and conscious sedation. Measurements were made using an end-hole catheter and a transducer using the standard technique. Systemic blood flow was calculated using the Fick method, and SVR and cardiac output were indexed to account for discrepant body surface area between the 2 patient populations. Pulmonary vascular resistance was not calculated because of known difficulties in measuring pulmonary blood flow in the failing Fontan circulation ; however, transpulmonary gradients were normal in each cohort. Hepatic vein wedge pressures were not routinely obtained and are likely not useful in Fontan patients with postsinusoidal portal hypertension. Finally, although pertinent medications are listed for each cohort, all such medications were held on the day of catheterization in each group.
At our institution, PF patients routinely undergo hepatic magnetic resonance imaging (MRI) or ultrasound at the age of 13 years, whereas adult Fontan patients receive liver imaging as part of their intake assessment. Computed tomography and ultrasound are used only when MRI is contraindicated. Imaging findings consistent with liver disease include changes in echogenicity by ultrasound or heterogenous enhancement of the parenchyma on delayed phase postcontrast imaging by MRI. Liver nodularity is a well-described imaging finding in patients with cirrhosis, indicative of the underlying distortion of hepatic architecture by formation of regenerative nodules. Varices were documented by imaging and not endoscopy. Liver imaging interpretations are those of the attending radiologist.
Analysis of the comparisons was completed using paired t test for continuous variables and Fisher’s exact test for categorical variables. We used SAS, version 9.2 (SAS Institute Inc., Cary, North Carolina). Data are expressed as mean values ± SDs. Statistical significance was defined as p value ≤0.05.
Results
A total of 27 SAF patients (aged 21 to 55 years) underwent a catheterization during the study period. All the patients had Fontan circulatory failure, reflected by clinical deterioration, as the indication for catheterization. Symptoms at the time of catheterization are depicted in Figure 1 . Pertinent mean catheterization findings of the cohort include central venous pressure of 18 ± 6 mm Hg, pulmonary capillary wedge pressure of 13 ± 5 mm Hg, systemic arteriovenous oxygen saturation difference of 24 ± 6%, SVR index of 1,680 ± 368 dyn s/cm 5 /m 2 , and cardiac index of 2.7 ± 0.8 L/min/m 2 .
Clinical features of the SAF and PF cohorts are listed in Table 1 . Compared with the PF cohort, the adult patients were statistically older at the time of Fontan palliation and farther removed from the Fontan at the time of catheterization. The SAF cohort was more symptomatic than the PF cohort by NYHA classification. Furthermore, of the 13 SAF patients (48%) who were in NYHA classes I and II, only 2 were in NYHA class I. Both these patients had severe fluid overload despite diuretics. NYHA class itself did not predict hemodynamic profile among the SAF cohort; there was no significant difference between patients in NYHA classes I and II and those in classes III and IV within this group. The SAF cohort contained a greater percentage of atriopulmonary Fontan palliations, whereas the PF group contained almost exclusively lateral tunnel and extracardiac Fontan patients. Finally, although angiotensin-converting enzyme inhibitors were more likely to be used in the PF cohort, β blockers were used with greater frequency in the SAF patients.
| Variable (Mean ± SD) | Adults, n = 27 (%) | Pediatric, n = 54 (%) | p |
|---|---|---|---|
| Age at catheterization (yrs) | 31.3 ± 9.3 | 13.7 ± 2.9 | <0.01 |
| Age at Fontan (yrs) | 10.6 ± 8 | 2.9 ± 2 | <0.01 |
| Time from Fontan to catheterization (yrs) | 20.7 ± 5.9 | 10.7 ± 3.8 | <0.01 |
| Male (%) | 52 | 46 | 0.71 |
| Height (cm) | 165.9 ± 33.5 | 150.8 ± 14.6 | 0.03 |
| Weight (kg) | 81.2 ± 18.8 | 45.7 ± 18.6 | <0.01 |
| Body surface area (m 2 ) | 2 ± 0.3 | 1.4 ± 0.3 | <0.01 |
| NYHA functional class ∗ | |||
| I and II | 48 | 94 | <0.01 |
| III and IV | 52 | 6 | |
| Atriopulmonary Fontan | 67 | 2 | <0.01 |
| Lateral tunnel Fontan | 33 | 69 | <0.01 |
| Extracardiac Fontan | 0 | 29 | <0.01 |
| Fontan fenestration | 11 | 87 | <0.01 |
| Systemic left ventricle | 81 | 44 | <0.01 |
| Systemic right ventricle | 19 | 56 | <0.01 |
| ACE inhibitor † | 41 | 74 | <0.01 |
| β Blocker † | 67 | 26 | <0.01 |
| Furosemide | 63 | 41 | 0.10 |
| Aldactone | 48 | 37 | 0.12 |
| Digoxin | 30 | 39 | 0.2 |
| Hemoglobin (g/dl) | 14.9 ± 2 | 14.6 ± 1.7 | 0.42 |
∗ Among the adult Fontan cohort, 13 (48%) of the 27 patients were NYHA class I and II; however, only 2 of these were NYHA class I. Both patients had significant fluid overload despite diuretics.
† ACE inhibitor and β-blocker use was not mutually exclusive. In the adult cohort, 8 patients (30%) were prescribed both medication classes, whereas 8 pediatric patients (15%) were prescribed both medicine types.
Tables 2 and 3 highlight differences in catheterization and echocardiographic findings between the SAF and PF cohorts. The hemodynamic profiles of the adult atriopulmonary versus lateral tunnel Fontans did not significantly differ and therefore were combined for analysis. The pediatric cohort had statistically lower values for central venous pressure and pulmonary capillary wedge pressure but greater SVR index. There was no significant difference in the cardiac index between the 2 groups. Indications for catheterization among the PF cohort are shown in Figure 2 .
| Parameters (Mean ± SD) | Adults (n = 27) | Pediatric (n = 54) | p |
|---|---|---|---|
| Central venous pressure (mm Hg) | 18 ± 6 | 14 ± 3 | <0.01 |
| Pulmonary capillary wedge pressure (mm Hg) | 13 ± 5 | 10 ± 3 | <0.01 |
| Aortic pressure (mm Hg) | 76 ± 12 | 79 ± 12 | 0.34 |
| Systemic arteriovenous pressure difference (mm Hg) | 57 ± 12 | 65 ± 12 | <0.01 |
| Mixed venous saturation (%) | 66 ± 8 | 68 ± 6 | 0.45 |
| Aortic saturation (%) | 91 ± 5 | 92 ± 4 | 0.46 |
| Systemic arteriovenous saturation difference (%) | 24 ± 6 | 24 ± 5 | 0.75 |
| Cardiac index (L/min/m 2 ) | 2.7 ± 0.8 | 2.8 ± 0.7 | 0.57 |
| SVR index (dyn s/cm 5 /m 2 ) | 1,680 ± 368 | 1,960 ± 550 | 0.02 |
| Parameters | Adults (%) | Pediatric (%) ∗ | p |
|---|---|---|---|
| At least moderate RV systolic dysfunction † | 80 | 12 | <0.01 |
| At least moderate TR † | 20 | 8 | 0.42 |
| Moderate or greater RV dysfunction or TR † | 80 | 15 | <0.01 |
| At least moderate LV systolic dysfunction ‡ | 18 | 5 | 0.21 |
| At least moderate MR ‡ | 23 | 19 | 0.78 |
| Moderate or greater LV dysfunction or MR ‡ | 27 | 24 | 0.93 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


