Chapter 35 Hemodynamic Monitoring in Critical Illness
Monitoring Devices
Arterial Pressure Monitoring
Noninvasive Arterial Blood Pressure Monitoring
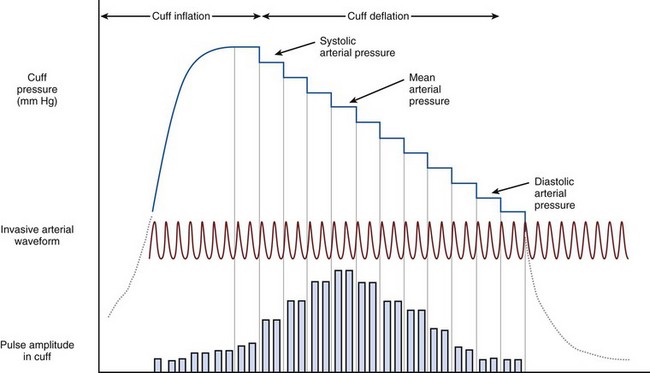
Noninvasive arterial blood pressure (NIBP) measurements in critical care most commonly are taken using an automated oscillometric device. This consists of a circumferential pneumatic cuff applied to the arm or leg. The cuff is inflated to a pressure above systolic arterial pressure, followed by controlled slow deflation of the cuff. As the cuff pressure falls below systolic arterial pressure, turbulent flow occurs in the artery beneath the cuff, causing oscillations in cuff pressure, which become maximal at MAP (Figure 35-1). Processing software allows determination of systolic, mean, and diastolic pressures in accordance with the amplitude of these oscillations.
Central Venous Catheterization
The complications of central venous cannulation are listed in Box 35-2. Despite advances in catheter technology such as antimicrobial coating, risk for microbial contamination is significant. The corresponding risk of catheter-related sepsis may be mitigated by minimizing the time during which the catheter remains in situ. The benefits of changing the catheter must be weighed against the risks associated with catheter reinsertion (Box 35-3).
Pulmonary Artery Catheterization
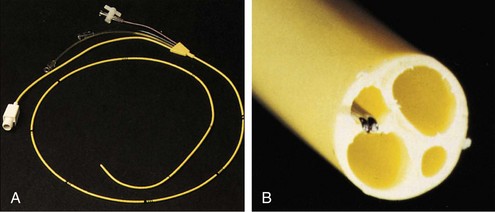
The pulmonary artery flotation catheter (PAFC) is a multilumen central venous catheter that is guided by flow to rest in the pulmonary artery (Figure 35-2). It allows measurement and derivation of a wide variety of hemodynamic variables, which are listed in Box 35-4. Indications for its use include the following:
• Determination of the cause of hemodynamic insufficiency
• Discrimination between cardiogenic and noncardiogenic pulmonary edema
• Measurement of cardiac output and pulmonary artery pressures (for example, in pulmonary hypertension or hepatopulmonary syndrome)
• Guidance in use of inotrope, vasopressor, or vasodilator therapy in critical illness or after major surgery
 is whole-body oxygen delivery, CO is cardiac output, and Ca
is whole-body oxygen delivery, CO is cardiac output, and Ca