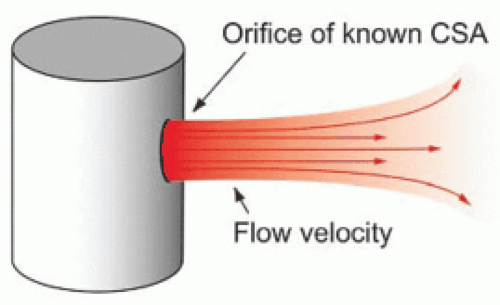
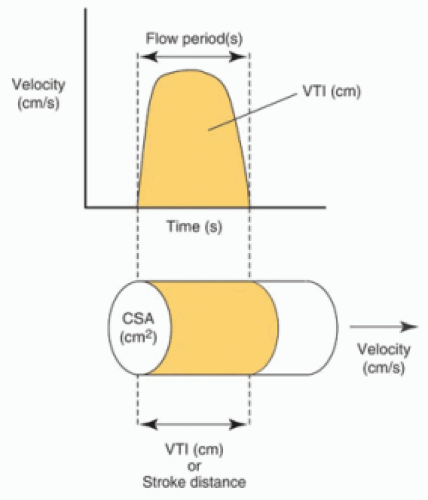
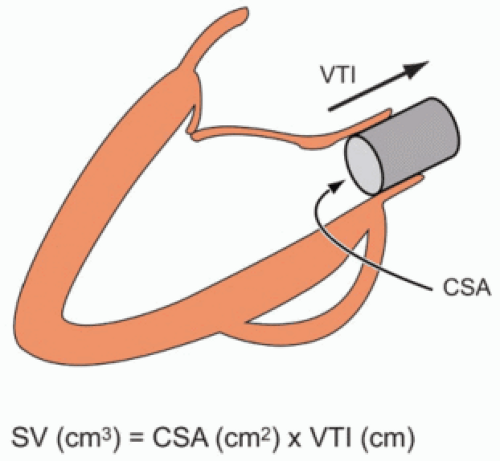
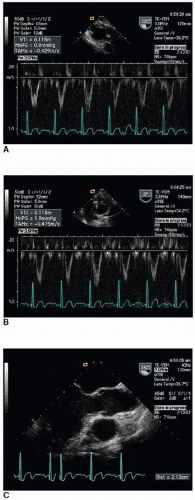
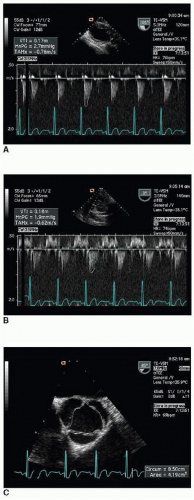
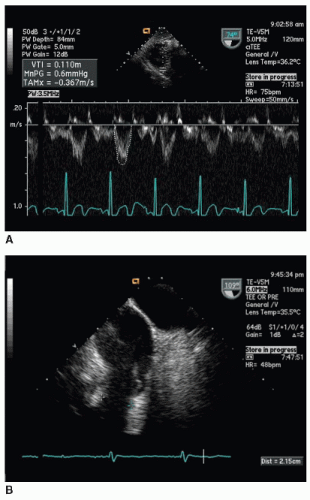
The Doppler velocity-time integral (VTI) can be used to calculate stroke volume (SV) at a specific location:
SV = CSA × VTI
Doppler-derived SVs can be used to determine cardiac output (CO), the pulmonary-to-systemic shunt ratio (Qp/Qs), and regurgitant volume (RV). However, propagation of errors may lead to a significant error in either the (Qp/Qs) or an RV calculated using Doppler SVs using transesophageal echocardiography (TEE).
The proximal flow convergence method can be used to determine regurgitant severity based on the maximal regurgitant orifice area:
EROA=6.28×r2×aliasing velocity)/VRJ
This method may overestimate the actual hemodynamic impact of the regurgitant lesion as the degree of regurgitation is not constant throughout systole in many patients. In spite of this and other limitations, the flow convergence method is useful in evaluating regurgitation as it is quantitative, relatively simple to perform, and applicable in a large number of patients with valvular regurgitation.
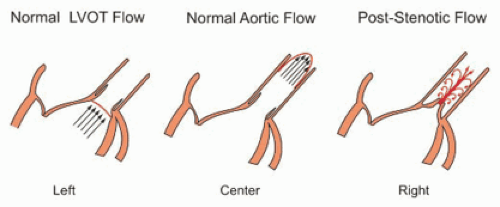
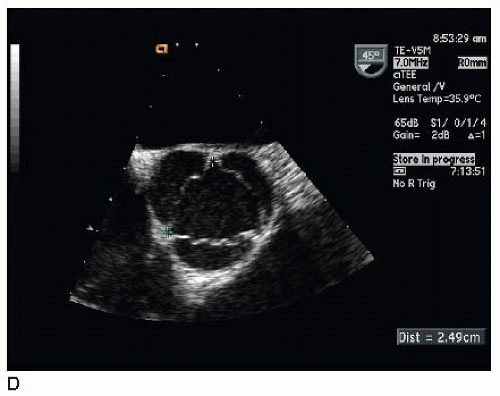
The continuity equation is another expression of the principle of conservation of mass (flow through the left ventricular outflow tract [LVOT] must equal flow through the aortic valve):
(AVA=CSALVOT × (VTILVOT / VTIAV)
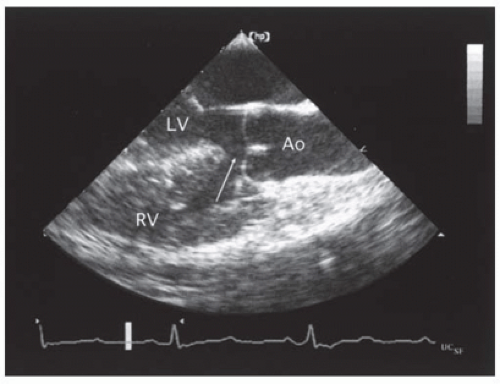
The primary concern in determining aortic valve area with the continuity equation using TEE is related to the possible underestimation of time-velocity integrals (TVIs) (or peak velocities) in the LVOT and/or aortic valve due to inadequate beam alignment.
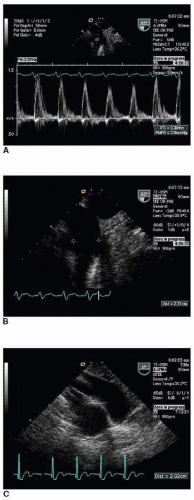
With valvular stenosis a longer pressure half-time (PHT) indicates more severe stenosis, whereas with valvular regurgitation a shorter PHT indicates more severe regurgitation. The PHT can be used to estimate the mitral valve area (MVA) of a stenotic native mitral valve using the following empirically derived formula:
MVA (cm2) = 220 / PHT (ms)
Estimation of an intracardiac or pulmonary pressure is possible by combining a pressure gradient calculated from a Doppler velocity using the simplified Bernoulli equation with a known or estimated pressure from a proximal or distal chamber. Example:
RVSP (mm Hg)=4 (vTR)2 + RAP (mm Hg)
TABLE 15.1 HEMODYNAMIC DATA OBTAINABLE WITH 2D DOPPLER ECHOCARDIOGRAPHY | ||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||
TABLE 15.2 ASSUMPTIONS FOR ACCURATE DOPPLER STROKE VOLUME CALCULATIONS | |||||
|---|---|---|---|---|---|
|
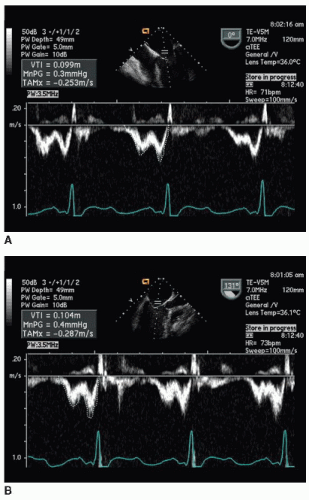
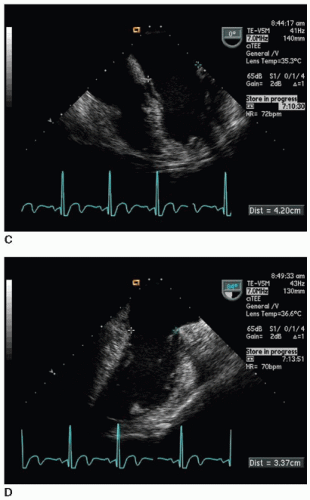
accurately when the ultrasound beam is perpendicular to the blood-tissue interface, while VTI is measured most accurately when the ultrasound beam is parallel to blood flow. Thus, diameter measurements and Doppler velocity profiles are usually not recorded from the same imaging plane. Efforts should be made to perform these measurements at the same anatomic location and in close sequence in order to minimize error in the calculated SV.
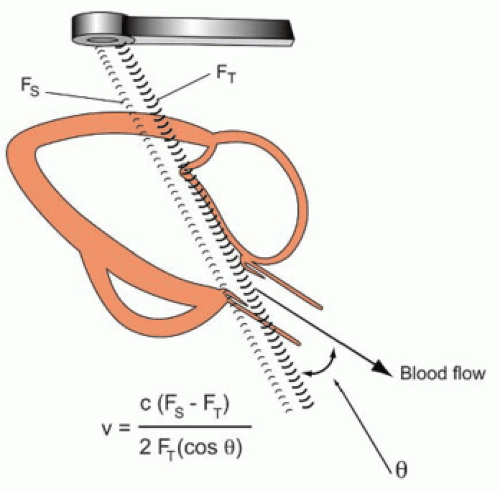
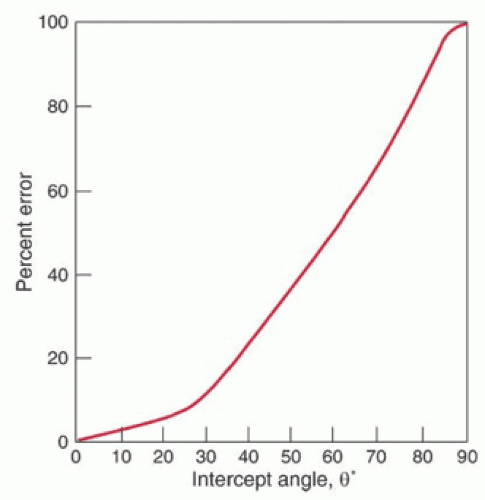
in the Doppler equation (Fig. 15-5). However, as θ increases from 20 to 60 degrees, the error in the calculated Doppler velocity increases from 6% to 50% (Fig. 15-6). The highest velocity signal obtained (the loudest audio signal) will correlate with the most parallel alignment of the Doppler beam with blood flow.
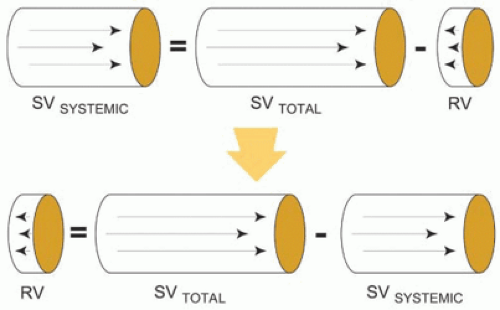
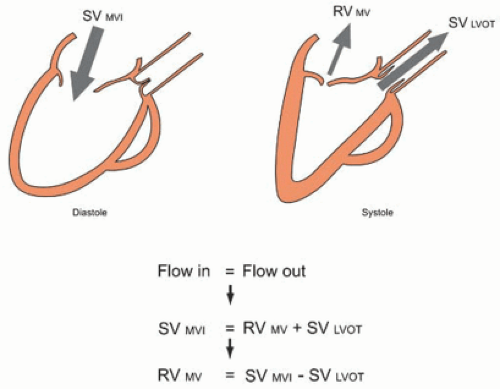
SV delivered to the systemic circulation (SVSYSTEMIC) must equal the total forward SV across a regurgitant valve (SVTOTAL) minus the RV (Fig. 15-12):
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree