(1)
Anatomy Department, University of Medicine and Pharmacy Carol Davila, Bucharest, Romania
Abstract
When regarding the hearts vascularization, broken rules are often the case. Here there are exceptions to almost every rule.
8.1 Arteries of the Heart
8.1.1 General Considerations
When regarding the hearts vascularization, broken rules are often the case. Here there are exceptions to almost every rule.
Perhaps more than in any other organ, individual variations of the heart’s vascular supply can be the deciding factor between life and death.
We shall briefly consider some of the characteristics of the heart’s vascularization, keeping in mind that these rules often have exceptions.
At first glance, the heart seems to have an independent vascular supply, isolated from the other organs. In fact, there are small anastomoses in the subepicardial plexus, connecting it to small branches originating in the pericardiophrenic, esophageal, bronchial, internal thoracic and mediastinal arteries.
Not only that, but the subepicardial space has angiogenetic properties. For instance, the greater omentum, if sutured to this plane, will develop arteriolar anastomoses with the subepicardial plexus. It is possible that other parts of the heart may have the same angiogenetic properties.
The hearts vascularization is terminal. This means that there are no anastomoses between the branches of an artery supplying a certain myocardial segment and those of another artery supplying the same segment. Therefore, the obstruction of an artery must lead to the infarction of its myocardial territory. This is the rule. However, if the arterial obstruction occurs slowly, gradually, there usually is enough time for anastomoses and collateral vessels to develop (“on demand-anastomoses”).
More than that, up to the age of one, there are numerous intercoronary anastomoses. In some cases, these persist up to adulthood. These intercoronary anastomoses are most often to be found:
at the apex, between branches of the anterior interventricular, posterior interventricular, and circumflex branch;
around the conus, between branches from the right and left coronary arteries.
on the pulmonary surface, between branches of the anterior interventricular and circumflex branches
on the sternocostal surface of the right ventricle, between branches of the anterior interventricular branch and the right coronary artery
in the subendocardial plexus, especially at the base of the papillary muscles
in the interventricular septum
in the vasa vasorum of the great vessels.
Another rule states that arteries are continued by an arteriolar–capillary network. However, there are arteriocavitary anastomoses (with the atrial or ventricular lumina) and even arterio-venous anastomoses, shunting the capillary bed.
In the myocardium there are structures called intertrabecular sinusoid spaces, especially in the wall of the left ventricle, with a diameter of about 250 μm. Some of the arterio-cavitary anastomoses are arterio–sinusoid anastomoses. Specific to these vessels is that they lack the tunica media, (thus being unresponsive to vasodilatatory signals [1]).
As a rule, when an artery descends into the muscular layer, it does not reemerge to the surface. This is not the case in cardiac anatomy, where myocardial bridges can cover arterial segments of various lengths. These occur most frequently over the anterior interventricular branch (Figs. 8.23 and 8.24), the obtuse marginal branch and the artery to the sinoatrial node (Fig. 7.17). Proximal, and sometimes distal to the myocardial bridge, the artery is slightly dilated.
It is noteworthy that the coronary arteries usually have a subepicardial course. In extreme cases, the arteries may have an intracavitary course through the aortic vestibule or the pulmonary infundibulum, or, as shown in our studies, through the atrial lumen (Figs. 8.53 and 8.54). Coronary arteries with a free intrapericardial course have been described.
As a rule, the sympathetic and parasympathetic autonomous systems have opposite effects on arterial muscle. In the heart, both acetylcholine and noradrenalin are coronarodilators.
In an organ consuming that much energy, one would expect a very long coronary perfusion time. This is not the case. Coronary blood flow is mostly diastolic, the coronary perfusion time is very short (8 s) and gets even shorter during exercise. All this is compensated by an immense capillary territory and a 1:1 ratio between capillaries and myocytes. In cardiac hypertrophy, this ratio remains unchanged and an imbalance between the cardiac fibers great volume and the limited capacities of the capillary occurs.
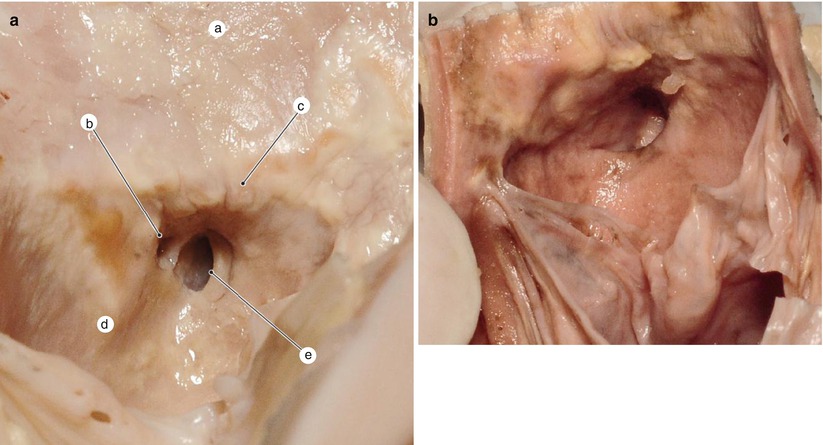
Fig. 8.1
(a) Left coronary sinus – detail. a aorta, b accessory coronary ostium, c supravalvular crest with atherosclerotic changes, d left coronary sinus, e the aortic-coronary margin at the level of the left coronary ostium. (b) Left coronary sinus with periostial atheromatosis – detail
As there are two coronary arteries, for a long time it was thought that there is a predefined, constant and predictable border between their vascularization–territories. Individual variation is the rule when concerning the heart’s vascularization. Coronary dominance spans from moderate to extreme. It is not wrong to state that every individual has his own “coronary map”.
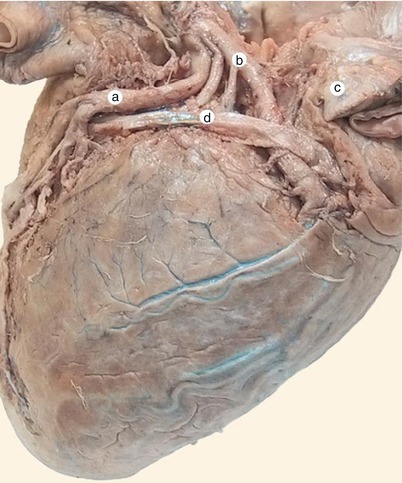
Fig. 8.2
Highlighting of the arteriovenous triangle (Brocq and Mouchet). a anterior interventricular artery, b circumflex artery, c left auricle, d great cardiac vein
In classical anatomy textbooks (Gray’s Anatomy, ed. 39, p. 1014) the dominant coronary artery is defined as the one supplying the posterior interventricular branch. This is true only if this branch has the proper length and diameter, because there are cases where this branch is short and slender, and even though it is situated in the posterior interventricular sulcus, it is by far not dominant.
We think that it is important to mention that there can be a left, a right, or a balanced dominance (a so–called co–dominance, when branches originating in both arteries descend through the posterior interventricular sulcus).
8.1.2 The Left Coronary Artery
The left coronary artery emerges from an ostium usually situated in the center of the left aortic sinus (Fig. 8.1). Usually, the greater part of this ostium is situated above the superior edge of the semilunar valve, but its position can vary: it can also be below this margin or completely above it (a so-called “tubular origin”). Seldom the left coronary artery can have its origin in the pulmonary trunk. Sometimes there can be two to three ostia in the left aortic sinus, the additional ones usually belonging to small branches.
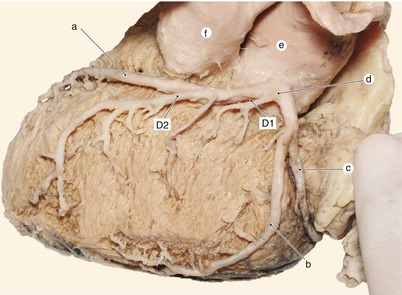
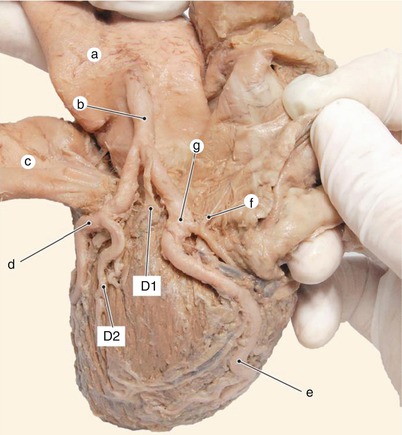
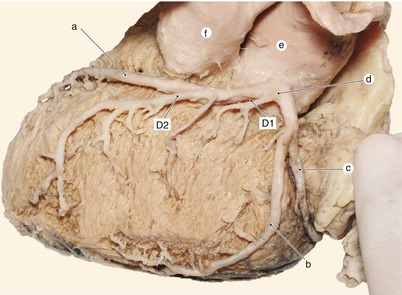
Fig. 8.3
The left coronary artery – view from the left side. a anterior interventriculary artery, b obtuse marginal artery, c circumflex artery, d left coronary artery with a short course, e aorta, f pulmonary trunk
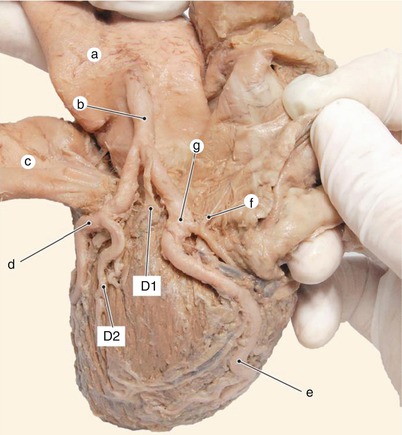
Fig. 8.4
Left coronary artery with a long course. a aorta, b left coronary artery with a long course, c pulmonary trunk, d anterior interventricular artery, e obtuse marginal artery, f an anterior atrial artery (from the circumflex artery), g bifurcation of the circumflex artery
The left coronary artery usually has a greater diameter than the right, of about 3–4 mm.
The left coronary artery can create anteriorly an “aorto-coronary edge”, rendering its catheterization for angiography more difficult.
The left coronary artery courses towards the left half of the coronary sulcus, being surrounded by the fatty tissue between the pulmonary trunk and the left atrial appendage (which also covers it). In this area, its bifurcation becomes a part of the arteriovenous triangle (Brocq and Mouchet): the base of the triangle is the greater cardiac vein, the two other sides are the anterior interventricular and the circumflex branches (Fig. 8.2).
The left coronary artery is considered to be short when its course is shorter than 0.5 cm (Figs. 8.3 and 8.6), or long, when over 0.5 cm; it can reach up to 2–3 cm (Fig. 8.4).
After this short course, the left coronary artery divides into two branches: the anterior interventricular branch, also called left anterior descending (LAD) by surgeons, and the circumflex branch (the angle between the two branches is about 90*).
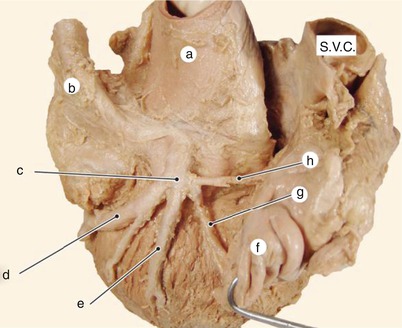
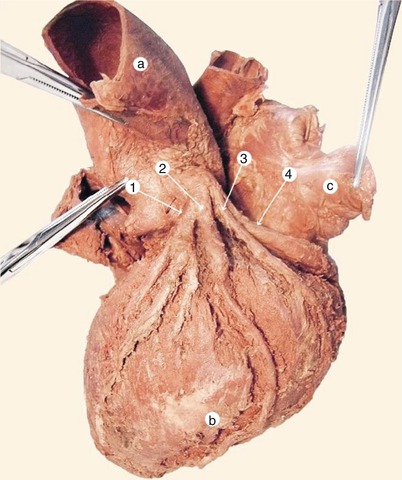
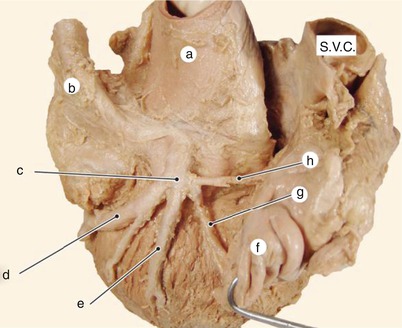
Fig. 8.5
Trifurcation of the left coronary artery. a aorta, b pulmonary trunk, c trifurcation of the left coronary artery, d anterior interventricular artery, e left ventricular diagonal artery, f left auricle, g circumflex artery, h artery to the sinoatrial node
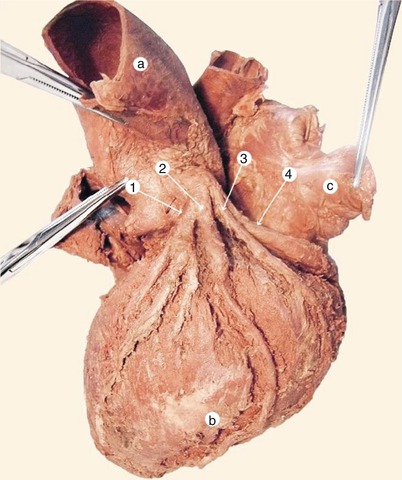
Fig. 8.6
Quadrifurcation of the left coronary artery. 1 anterior interventricular artery, 2 left ventricular diagonal artery, 3 obtuse marginal artery, 4 circumflex artery, a aorta, b obtuse margin, c left auricle
The left coronary artery can also divide into three or four branches.
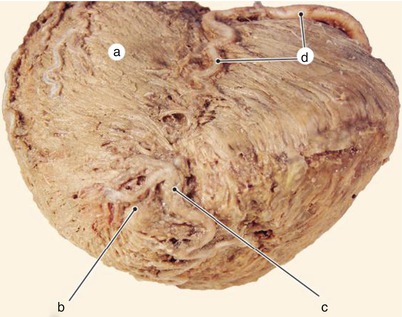
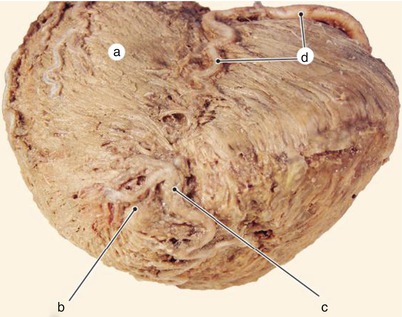
Fig. 8.7
Recurrent an posterior interventricular arteries. a diaphragmatic surface of the left ventricle, b vortex, c recurrent artery, d right coronary artery and posterior interventricular artery
When there are three branches, the middle can be called the “animus intermediate” artery, median artery, left diagonal etc (Fig. 8.5).
In the case of four branches, these are labeled, from anterior to posterior: anterior interventricular branch, left ventricular diagonal artery, obtuse marginal artery and circumflex branch (Fig. 8.6).
8.1.2.1 The Anterior Interventricular Branch
The anterior interventricular branch (left anterior descending) descends through the eponymous sulcus together with the greater cardiac vein. Its relation to the vein is very variable (Figs. 4.8 and 4.9). It reaches the notch at the heart’s apex and then continues on the diaphragmatic surface as the recurrent artery (Figs. 8.7 and 8.8). It ascends 1–2 cm through the posterior interventricular sulcus and then ends by dividing into two or more branches. It can anastomose at the apex with the posterior interventricular or circumflex branch (Fig. 8.9) (the recurrent artery rarely occupies the whole posterior interventricular sulcus).
A special variation is the bifurcation of the anterior interventricular branch. We can describe a true bifurcation when both branches are situated in the anterior interventricular sulcus, with the shorter one also ending there (Fig. 8.11). A pseudobifurcation is the case when the shorter branch does not end its course in the sulcus (Fig. 8.12). These details are important in cardiac surgery.
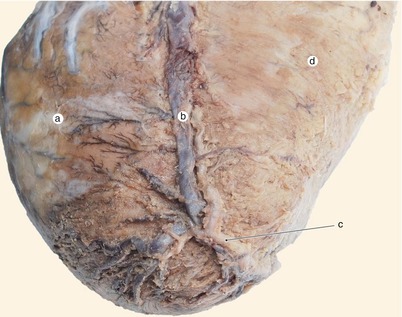
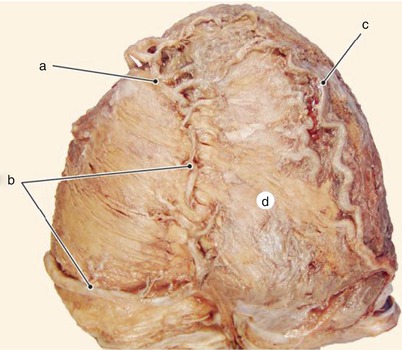
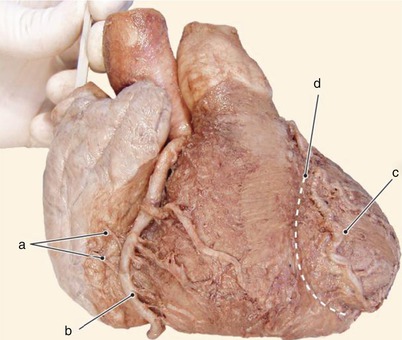
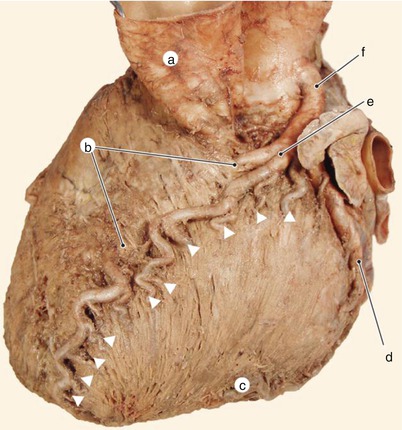
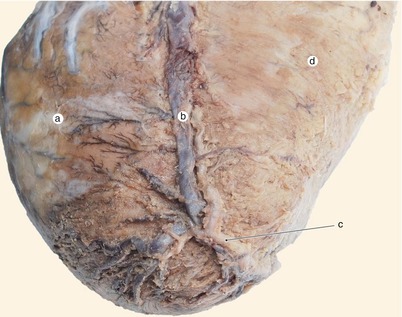
Fig. 8.8
Recurrent artery high ascending in the posterior interventricular sulcus. a diaphragmatic surface of the left ventricle, b middle cardiac vein, c recurrent artery, d diaphragmatic surface of the right ventricle
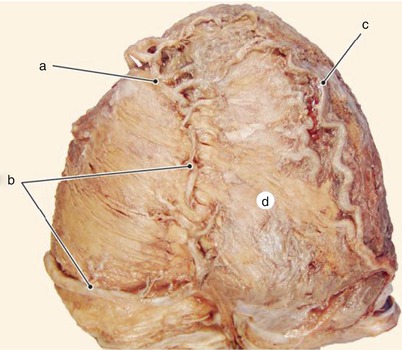
Fig. 8.9
The cardiac apex is an area where all three main coronary arteries can anastomose. a recurrent artery (from the anterior interventricular artery), b right coronary artery and posterior interventricular artery, c obtuse marginal artery (from the circumflex artery), d diaphragmatic aspect of the left ventricle
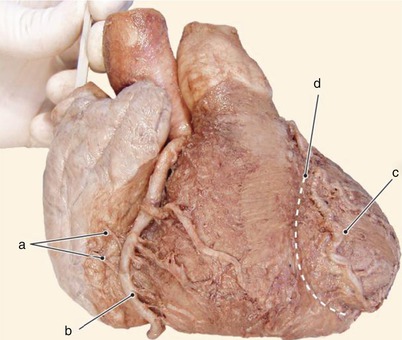
Fig. 8.10
The anterior interventricular artery actually runs left to the homonymous sulcus. a anterior atrial arteries, b right coronary artery, c anterior interventricular artery, d anterior interventricular sulcus
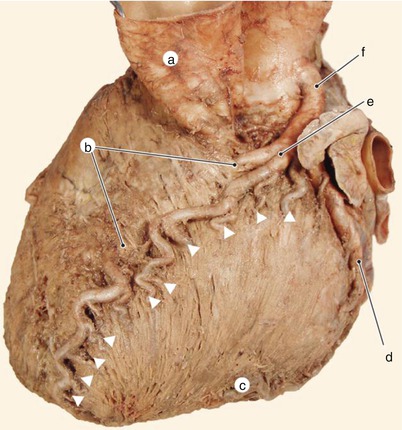
Fig. 8.11
“True” bifurcation of the anterior interventricular artery. The arrowheads indicate the origins of the septal arteries. a pulmonary trunk, b myocardial bridge over the anterior interventricular artery, c obtuse margin, d circumflex artery, e true bifurcation, f left coronary artery (long course)
In case of clinical signs of myocardial infarction around the bifurcation, it is possible that only one of the two branches is obstructed.
The angiographic visualization of the permeable branch can lead to misdiagnosing and missing the chance of performing a coronary intervention.
Clinically the anterior interventricular branch is topographically divided into three segments (based on angiographic criteria): the proximal segment (from the origin to the emergence of the main septal branch), the middle segment (to the origin of the second diagonal branch) and the distal segment (to the end of the artery) (Fig. 8.13).
The branches of the anterior interventricular branch also show variability regarding their origin, length, diameter and vascularization territory.
Most frequently, the anterior interventricular branch has the following branches:
vasa vasorum for the origins of the great vessels (Fig. 8.14);
anterior right ventricular branches;
anterior left ventricular branches, also called diagonal branches (some of these can also be double);
anterior septal branches, also called perforating branches;
posterior septal branches, emerging from the recurrent artery.
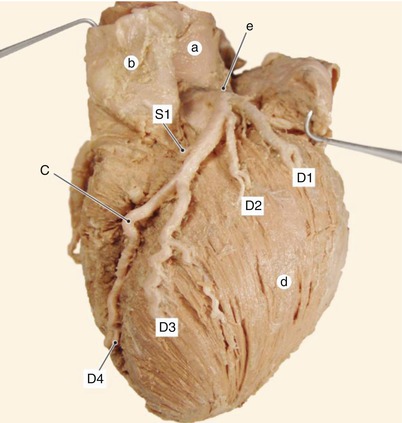
Fig. 8.12
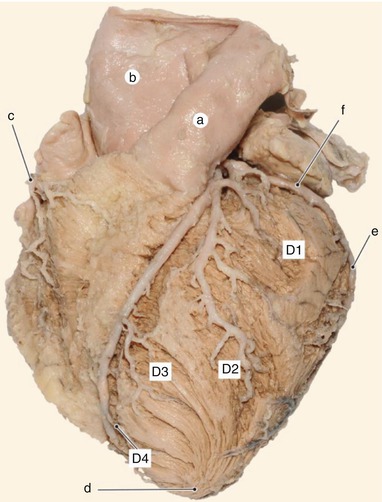
Pseudobifurcation of the anterior descending artery – actually the emergence of D3. a aorta, b pulmonary trunk, c anterior interventricular artery, d obtuse margin, e left coronary artery. S1 first septal artery, D1–D4 diagonal arteries
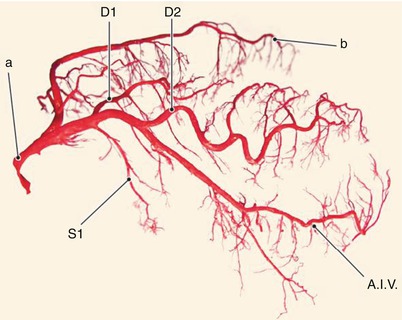
Fig. 8.13
The segments of the anterior interventricular artery (methylmetacrylate coronary mold): the proximal segment – from the emergence to S1, middle segment –between S1 and D2, distal segment – beyond D2. a left coronary artery, b circumflex artery. A.I.V anterior interventricular artery
We would like to mention that the anterior ventricular branches usually have a short subepicardial course and then penetrate the myocardial layer. The various groups of anterior branches will now be individually described:
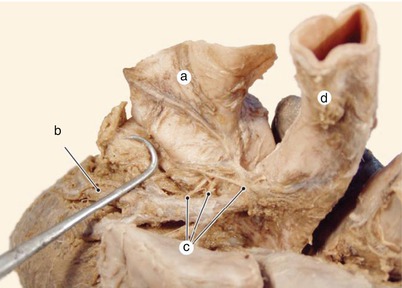
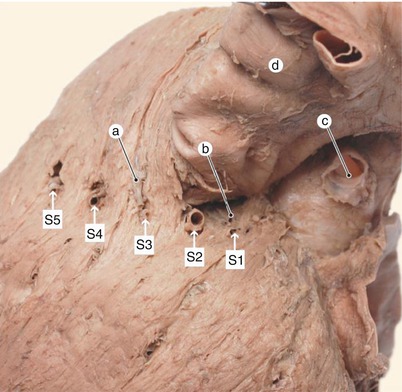
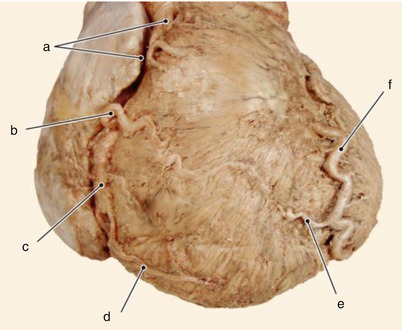
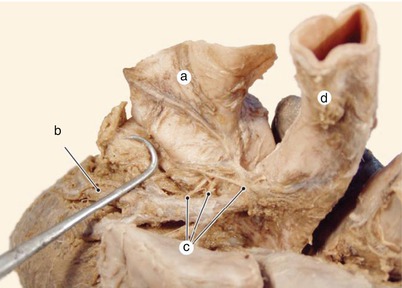
Fig. 8.14
Vasa vasorum of the aorta highlighted. a pulmonary trunk, b anterior interventricular artery, c vasa vasorum, d aorta
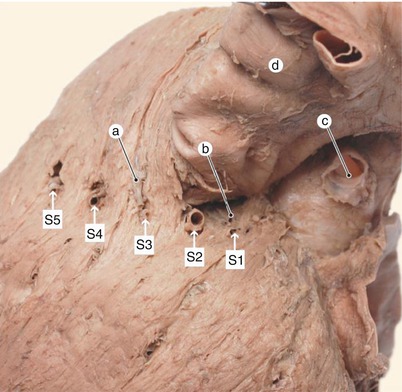
Fig. 8.15
Highlighting the septal arteries and infundibular branches. a preinfundibular artery, b retroinfundibular artery, c left coronary artery, d pulmonary trunk
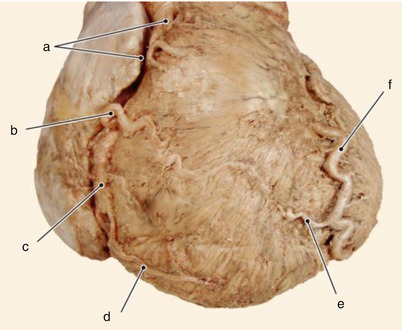
Fig. 8.16
Intercoronary anastomosis on the sternocostal aspect of the heart. a conal arteries, b right ventricular diagonal artery, c right coronary artery, d right marginal artery, e anterior right ventricular artery, f anterior interventricular artery
The anterior right ventricular branches are few and usually short. Sometimes there is a left conal (or left periinfindibular) artery (Figs. 8.15 and 8.19), which, together with a homonymous branch from the right coronary artery, creates “the arterial periinfundibular ring” (Vieussens). Sometimes there are one to two right branches (Fig. 4.30). One of these long subepicardial branches can anastomose with a diagonal branch of the right ventricle (Fig. 8.16).
The right-sided branches are:
the right conal branch (called the “third coronary artery” when it has its own aortic ostium). It runs anteriorly to the conus (Fig. 4.35).
The left-sided branches are: the left conal branch (left preinfundibular) (Fig. 8.15) and a left retroinfundibular branch (which can emerge directly from the anterior interventricular branch or, frequently, from the first septal branch) (Figs. 8.17, 8.18, 8.19, 8.32 and 6.98).
The anterior left ventricular branches (lateral branches in N.A.I.) are more numerous (2–10) and also variable when considering their number or position. Some of these branches have a more constant course and are easier to identify, even if their origin is variable (from the left coronary artery or from the circumflex branch): the first left ventricular diagonal branch and the obtuse marginal branch (Fig. 8.3). Their names are very suggestive for their course. When describing individual branches of this type it is always important to mention their origin (e.g. the first diagonal branch of the left ventricle, a branch of the anterior interventricular branch). These arteries vascularize, completely or together with other branches, the anterior mitral papillary group.
All of the anterior left ventricular branches are called diagonal when there are more than two, when these are parallel to each other and when they course towards the acute margin and the apex (They are labeled D1, D2, etc.) (Figs. 8.12, 8.20, 8.21, 8.22, 8.23, 8.24 and 8.25).
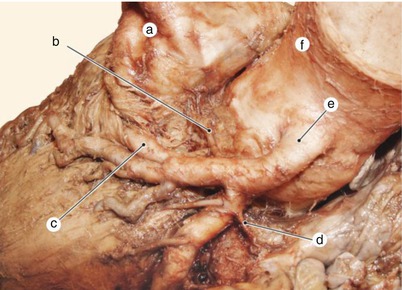
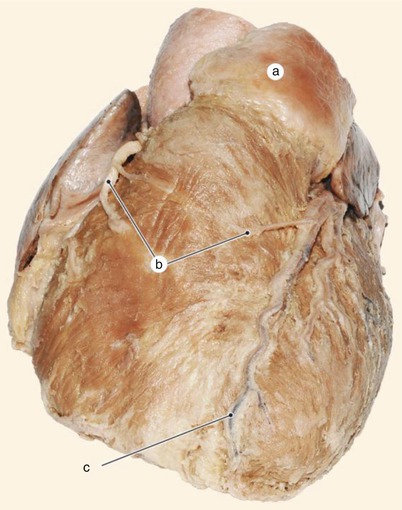
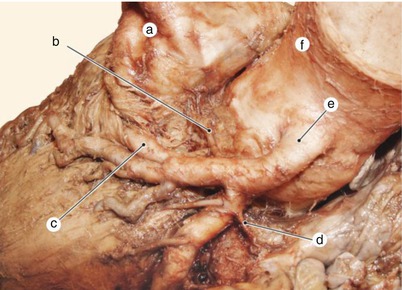
Fig. 8.17
Proximal part of the retroinfundibular artery (from the left coronary artery). a pulmonary trunk, b retroinfundibular artery, c anterior interventricular artery, covered by myocardial bridge, d anterior atrial artery, e left coronary artery, f aorta
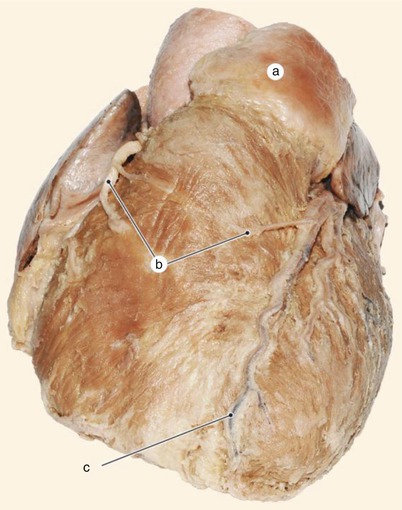
Fig. 8.18
Conal arteries. a pulmonary trunk (with bulbous proximal segment), b anterior conal arteries, c anterior interventricular artery
As a general rule, when the first branches are of greater size, the others are smaller.
The anterior interventricular septal (perforating) branches emerge in a parallel pattern from the anterior interventricular branch and vascularize roughly the anterior 2/3 of the interventricular septum.
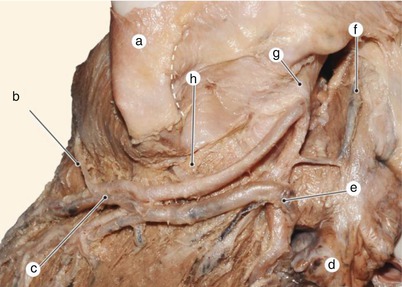
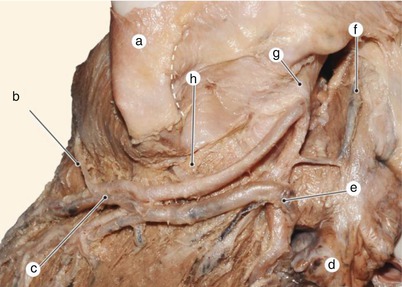
Fig. 8.19
Infundibular branches emerging from the anterior interventricular artery. a pulmonary trunk, b preinfundibular artery, c anterior intreventricular artery, d left auricle, e greater cardiac vein, f greater anastomotic artery, g left coronary artery, h retroinfundibular artery
Figures 8.13, 8.28 and 8.29 show methylmetacrylate molds of the left coronary artery and its major branches.
The first septal branch of greater caliber, frequently the second septal branch – S2, is called the main septal branch. It originates left of the infundibuloventricular junction, near the emergence of the first diagonal branch (Figs. 8.26 and 8.27). Angiographically, its course at a right angle to the anterior interventricular branch helps identify the latter.
It very often vascularizes the postperforating segment of the His bundle, thence its great clinical importance. This artery also supplies a great part of the crista of the interventricular septum, the medial tricuspid papillary muscle, and, together with a branch from the right coronary artery, the anterior tricuspid papillary muscle.
Sometimes a big S1 has its own ostium in the left aortic sinus, and is labeled the main septal branch. This is Vieussens’ internal coronary artery (Fig. 8.30).
!Regardless which is the main septal branch, a smaller branch may emerge adjacent to its ostium (Fig. 8.31).
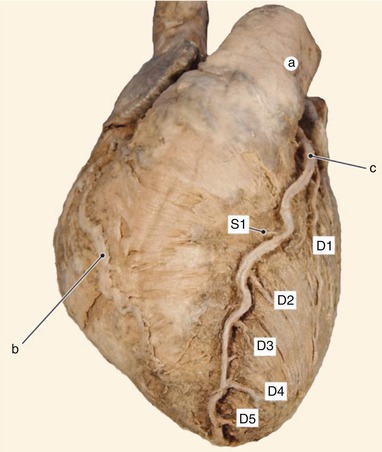
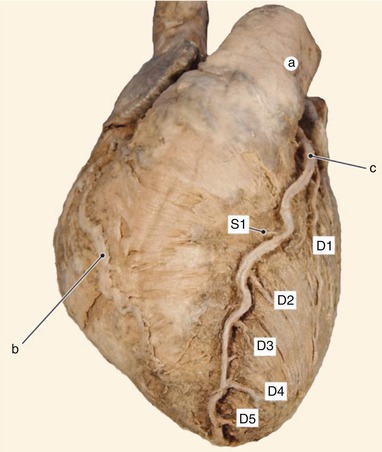
Fig. 8.20
Diagonal branches (D1–D5), first septal artery (S1), from the anterior interventricular artery. a pulmonary trunk, b right ventricular diagonal artery, c anterior intreventricular artery
Posterior septal branches emerge from the recurrent artery and supply the posterior third of the apical part of the interventricular septum (Fig. 8.29).
In some cases, especially concerning the first septal branches, two arteries may have a common emergence from the anterior interventricular branch. This can render coronary stenting very difficult or even impossible (Fig. 8.31).
Septal branches can communicate with the left ventricle, establishing arterioluminal anastomoses (Fig. 8.32).
The Romanian anatomist A. Crainicianu named the diagonal arteries and the myocardial bridges at the beginning of the last century [2].
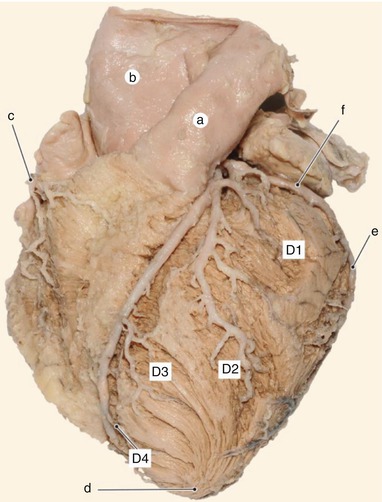
Fig. 8.21
The anterior interventricular artery and its diagonal branches (D1–D4). a pulmonary trunk, b aorta, c conal arteries, d vortex, e obtuse marginal artery, f circumflex artery
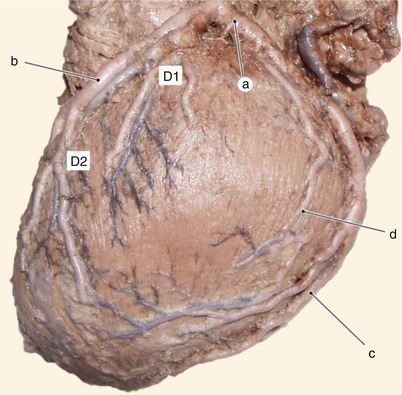
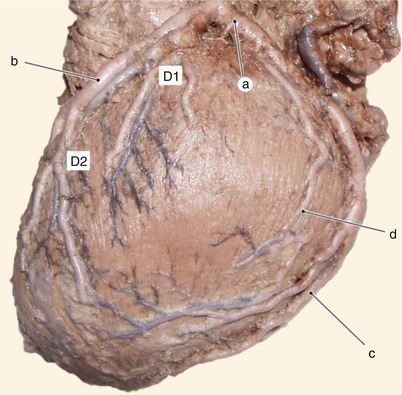
Fig. 8.22




Diagonal arteries (D1 and D2). Arterial branches for the pulmonary surface of the heart. a circumflex artery, b anterior interventricular artery, c obtuse marginal artery, d left ventricular diagonal artery, originating from the circumflex artery
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


