Heart Sound Dynamics
1. How do heart sounds originate?
2. Name the two basic heart sounds and the valves associated with each.
3. How many characteristics are used to describe heart sounds?
4. How does the electrocardiogram (ECG) correlate with the heart’s electrical activity?
5. How can you accurately document the heart sounds heard during auscultation?
HEART SOUND ORIGINS
The heart sounds heard through a stethoscope during auscultation are generated by vibrations from the heart’s walls and valves and from turbulent blood flow. Normally, the heart’s walls and valves are compliant as they move in response to pressure and volume changes during the cardiac cycle.
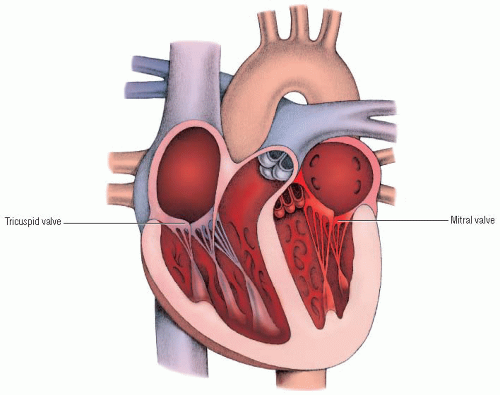
Blood flow
At the beginning of ventricular diastole, the ventricles are relaxed, and the aortic valve closes slightly before the pulmonic valve. For a brief time, both the atrioventricular (AV) and semilunar valves are closed. During this period, called isovolumic relaxation, intraventricular pressures continue to fall. However, the opening of the tricuspid and mitral valves follows quickly, and blood begins to flow passively from the atria into the ventricles. As the ventricles become distended, the rate of ventricular filling decreases. Then, as the atria contract (from stimulation of the atrial myocardium by an electrical impulse from the sinoatrial [SA] node), the ventricular volume is slightly boosted. The resulting increase in ventricular pressures causes the mitral and tricuspid valves to begin closing.
During atrial systole, the electrical impulse moves more slowly through the AV node and into the bundle of His. The impulse proceeds rapidly through the bundle branches and the Purkinje fibers, activating ventricular systole. Early in ventricular systole, intraventricular pressures increase above intra-atrial pressures, and the mitral and tricuspid valves close suddenly. Normally, the mitral valve closes slightly before the tricuspid valve.
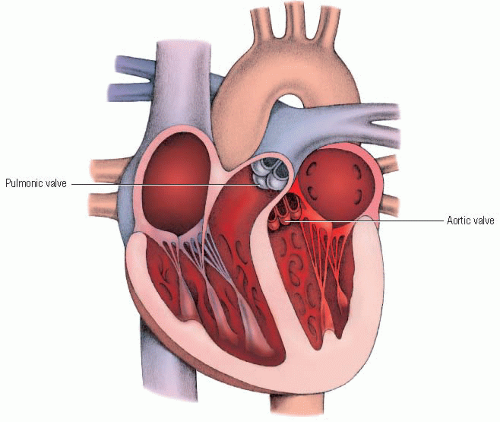
For another brief period, both the AV and semilunar valves are closed. During this period, known as isovolumic contraction,
ventricular pressures increase, becoming higher than the pressures in the pulmonary artery and aorta. The aortic and pulmonic valves open, and blood is ejected through them. Normally, the aortic valve opens slightly before the pulmonic valve.
ventricular pressures increase, becoming higher than the pressures in the pulmonary artery and aorta. The aortic and pulmonic valves open, and blood is ejected through them. Normally, the aortic valve opens slightly before the pulmonic valve.
After a period of maximum ejection of blood from the ventricles, the ventricles begin to relax. As intraventricular pressures fall rapidly, a brief backflow of blood from the pulmonary artery and aorta toward the ventricles occurs. Reduced intraventricular pressures and the temporary backflow of blood are associated with the closure of the aortic and pulmonic valves at the end of systole.
BASIC HEART SOUNDS
A normally functioning heart produces two basic heart sounds: S1 and S2. (♦ Sound 1) S1, the first heart sound, is heard at the beginning of systole. It’s associated with the closure of the mitral and tricuspid valves and the increasing pressures within the ventricles that cause the moving valve leaflets and cord structures to decelerate. S1 is generated by the closing of AV valves and the vibrations associated with tensing of the chordae tendineae and the ventricular walls.
At the end of ventricular systole, ventricular pressures fall rapidly, causing a slight backflow of blood from the aorta and pulmonary artery. The decrease in ventricular pressures to a level below that of aortic and pulmonic systolic pressures and the temporary backflow of blood and recoil events are associated with the closure of the aortic and pulmonic valves. (See Valves producing second heart sound [S2].) The vibrations associated with these events produce the second heart sound, S2, which marks the end of ventricular systole. (♦ Sound 2)
Characteristics
Every heart sound has six different characteristics that need to be assessed during auscultation. These are location, intensity, duration, pitch, quality, and timing. If you keep these characteristics in mind each time you perform auscultation, you’ll ensure a complete assessment of heart sounds, and you’ll be able to provide the information necessary for an accurate and complete documentation. Also, because these terms are used universally, all health care professionals will be able to understand your auscultatory findings.
Location
A sound’s location is the anatomic area on the patient’s chest wall where the sound is heard best. Bony structures and landmarks, such as the right and left midclavicular lines, are used to describe the precise location. For example, you might document that S1 was heard best over the mitral area.
Intensity
Intensity refers to the sound’s loudness during auscultation. Usually, a sound’s intensity is determined somewhat subjectively, based on experience. However, when abnormalities are present, intensity can be determined electronically by recording a phonocardiogram (PCG) and by measuring the amplitude of the sound’s vibrations. A PCG is a graphic representation of heart sounds that can be compared with the sounds heard during auscultation and with the heart’s electrical activity recorded on the patient’s ECG.
Keep in mind that heart sound intensity is related to the pressures generated and the blood flow velocity within the heart. It’s also related to the patient’s size, body build, and chest configuration. For example, a slender patient has a thinner chest wall; therefore, sounds are transmitted more easily through a slender patient’s chest wall than through an obese patient’s chest wall. Sounds can also be diminished by certain media, such as pericardial fluid or emphysematous lung tissue.
Duration
Sound duration refers to the length of time the sound is heard; it can be described as either short or long. Remember, heart sounds are brief vibrations that mark the beginning and end of systole. A sound’s duration affects whether you hear it as a click, a snap, or a murmur. For example, murmurs are longer vibrations usually associated with blood flow during systole or diastole.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree