We explored the directions of the repolarization sequence (RS) and excitation sequence (ES) as determinants of QRS|T angle widening in 126 patients with acute coronary syndrome (ACS) with and 658 patients without diagnostic ST-segment elevation myocardial infarction and in a reference group of 5,376 normal subjects. The initial and terminal RS and ES directions were derived from the initial and terminal T and QRS vectors from quintiles 1 to 3 and 5 of time-normalized QRS and T. In addition to the QRS|T angle, we evaluated the RS and ES deviation angles from the normal RS and ES directions. The normal zones for the ES and RS directions in the reference group were used to classify the ES and RS in the group with and without ST-segment myocardial infarction as normal or deviant. The initial and terminal QRS|T angles were rate invariant in the normal group but correlated with the heart rate (r = 0.33) in the ACS group. Adjusted for a heart rate of 70 beats/min, the initial QRS|T angle increased progressively in the ACS group from 41° among those with normal RS and ES directions to 121° when both were deviant. This apparently ischemia-induced initial QRS|T angle increase was associated with an initial RS direction from the anterior-right to the posterior-left producing a progressively greater peak TV1 amplitude. The terminal ES orientation in the ACS group was toward the right ventricular outflow tract with a QRS|T angle of 124° in 48% and leftward and posterior, with the QRS|T angle decreasing to 59°, in the remaining 52%. In conclusion, the initial and terminal RS and ES orientations differ drastically and their deviant orientation accounts for the widened QRS|T angle in patients with ACS, differences not revealed by evaluation of the mean QRS|T angle.
The QRS|T angle has been associated with increased risk of coronary heart disease and all-cause mortality and of nonfatal coronary heart disease events. A widened QRS|T angle is generally considered a marker of “deviant” repolarization. Information is lacking about the mechanism of widening of the QRS|T angle in various abnormal conditions. Most of the previous reports on the QRS|T angle have used the angle between the mean QRS and T vectors, at times computed as the mean angle or its cosine between the first principal components of QRS and T. It became clear early on in the present investigation that the QRS|T angle differs widely between the initial and terminal phases of repolarization and that the mean QRS angle does not reveal these differences. The purpose of the present investigation was to evaluate the ischemia-induced changes in the QRS|T angle in patients with acute myocardial infarction with and without ST-segment elevation (STEMI and NSTEMI, respectively), with a special objective of elucidating the mechanisms that would account for the widening of the QRS|T angle observed in patients with acute coronary syndrome (ACS).
Methods
The source data for the reference normal group were selected from community-based populations, mainly from the Third National Health and Nutrition Examination Survey (NHANES III) conducted from 1988 to 1994. The normal subgroup (aged 40 to 90 years, 47% men) has been described in previous studies. Excluded were subjects with a history of heart attack, coronary artery bypass surgery, or coronary angioplasty. Electrocardiographic-based exclusions included complete bundle branch block (QRS duration >120 ms), electronic pacemakers, and other major electrocardiographic abnormalities using the Novacode electrocardiographic classification system (old myocardial infarctions and isolated major ST- and T-wave abnormalities). The source data of the ACS group consisted of admission electrocardiograms from a research data file of one of us (R.S.). A combination of visual and automated quality control procedures using tolerance windows for critical global electrocardiographic wave onset and offset reference points were applied to detect “outliers.” After these quality control measures, the electrocardiograms of 5,376 normal subjects (2,552 men and 2,824 women) and 784 patients with acute myocardial infarction qualified for the present study. Most of the patients in this special collection of acute myocardial infarction recordings of patients with ACS were classified as having NSTEMI (84%). The remaining 16% met the diagnostic criteria for acute STEMI (ST-segment elevation in 2 congruent leads ≥200 μV in V 1 to V 3 or ≥100 μV in other leads). Nine patients in the STEMI group (7%) and 102 (16%) in the NSTEMI group had a history of a previous myocardial infarction. The mean age of the ACS group was 59 ± 15 years.
The electrocardiograms for the normal subjects were recorded with the subject at rest in a supine position using a comparable and strictly standardized procedure for electrocardiographic acquisition. All electrocardiograms were analyzed at a central electrocardiographic laboratory and were inspected visually to detect technical errors, missing leads, and inadequate quality. Such records were rejected from the electrocardiographic data files. The electrocardiograms of the myocardial infarction group were the admission electrocardiograms recorded in the emergency department of the Long Beach Memorial Hospital (Long Beach, California). The electrocardiographic measurements for the present study were obtained using the Philips DXL electrocardiographic program (Philips Healthcare, Andover, Massachusetts).
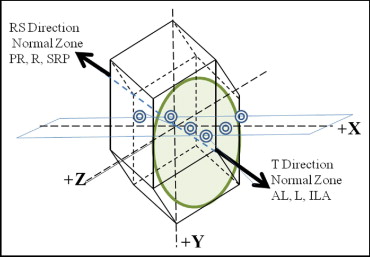
Repolarization measurements were made from the “global” T wave, the spatial T vector magnitude curve obtained from an inverse transformation matrix used to derive the XYZ leads from the 8 independent components of the 12-lead electrocardiograms. The T wave and QRS durations vary from subject to subject with the heart rate and other factors influencing the duration of repolarization. The T wave and QRS durations were time normalized and divided into 5 quintiles. Quintiles 1 to 3 were considered to represent the initial repolarization, quintile 5 the terminal, and quintile 4 the transition period of repolarization. The spatial direction of the repolarization sequence (RS) vector is diametrically opposite to the mean T vector, and the spatial direction of the excitation sequence (ES) vector is equal to that of the QRS vector. Thus, the spatial angle between ES and RS vectors, Θ(ES|RS) = 180° − Θ(QRS|T), where Θ(QRS|T) is the spatial angle between the QRS and T vectors during the corresponding periods of excitation and repolarization. Detailed steps for computation of the directional distributions of the ES and RS vectors in the 12 reference directions of a rhombic dodecahedron lattice ( Figure 1 ) have been described by Rautaharju et al in the Appendix, which also includes a procedure for simplified computation of the initial QRS|T angle from the maximum QRS and T vectors or from the visually measured peak QRS and T amplitudes, instead of the more elaborate computation using the initial 3 quintiles of QRS and T. The RS direction is labeled congruent with the normal RS direction in the reference group (RSref) if the cosine of the spatial angles between the RS and RSref vectors [Θ(RS|RSref)] is >0 and incongruent otherwise. Similarly, the ES direction is labeled congruent with respect to the ES direction in the normal reference group (ESref) if the cosine Θ(ES|ESref) is >0 and incongruent otherwise.
Microsoft Excel, version 2007 for Windows (Microsoft, Redmond, WA), was used to calculate the parameters for the repolarization variables and determine their statistical distributions. Student’s 2-way t test was used to determine the significance of the group differences for the parameters of interest and z -test for proportions was used to compare proportions of narrow and wide QRS|T angles separately for STEMI and NSTEMI.
Results
The heart rates in the ACS group were considerably greater than those in the reference group, 81 beats/min in the STEMI group and 86 beats/min in the NSTEMI group ( Table 1 ). The mean and maximum QRS|T angles were wider in men than in women and wider in the NSTEMI group than in the STEMI group.
| Variable | Normal Group | Acute MI group | ||
|---|---|---|---|---|
| Men (n = 2,554) | Women (2,824) | STEMI (n = 126) | NSTEMI (n = 662) | |
| Heart rate (beats/min) | 70 ± 11.5 | 69 ± 11.1 ⁎ | 81 ± 21.9 | 86 ± 23.3 † |
| QRS duration (ms) | 94 ± 9.2 | 90 ± 8.8 ‡ | 94 ± 11.8 | 95 ± 10.5 ⁎ |
| Interval from QRS onset to peak of R wave in V 6 (ms) | 45 ± 5.6 | 44 ± 5.2 ‡ | 44 ± 10.2 | 44 ± 9.4 ⁎ |
| Rate-adjusted QT interval § (ms) | 420 ± 19.0 | 428 ± 19.8 ‡ | 429 ± 28.4 | 433 ± 30.1 ⁎ |
| Mean spatial angle between mean QRS and T vectors (°) | 73 ± 28.8 | 56 ± 27.7 ‡ | 73 ± 36.9 | 95 ± 45.0 ‡ |
| Maximum spatial angle between mean QRS and T vectors (°) | 61 ± 34.2 | 45 ± 30.3 | 76 ± 40.6 | 90 ± 51.7 ‡ |
| Spatial angle between QRS and T vectors computed from initial 3 quintiles of global QRS and T waves (°) | 55 ± 23.6 | 42 ± 26.8 ‡ | 73 ± 35.2 | 89 ± 47.7 ‡ |
| Spatial angle between QRS and T vectors computed from last quintile of global QRS and T waves (°) | 130 ± 28.2 | 128 ± 28.6 ⁎ | 85 ± 36.1 | 117 ± 38.0 ‡ |
‡ p <0.001; for mean difference between genders and between STEMI and NSTEMI groups.
§ QT − k × (RR − 1), where k = 158 for men and k = 167 for women.
Although the initial QRS|T angle in the reference group was rate independent (R 2 = 0.0025), in the combined STEMI and NSTEMI group, its correlation with the RR interval was 0.30 and slightly greater with heart rate (r = 0.33). An evaluation of the separate formulas for QRS|T angle adjustment for heart rate in the STEMI and NSTEMI groups by gender revealed that the differences for a 10-beat/min increase in heart rate were minimal, <1°. Thus, all QRS|T angles in the ACS group were adjusted using a common formula for heart rate of 70 beats/min (the rate in the reference group) for evaluation of the role of the heart rate dependence of the QRS|T angle ( Table 2 ). Comparing the unadjusted and rate-adjusted values (last 2 rows in Table 2 ), the proportion of the QRS|T angle widening or narrowing owing to the heart rate was close to 10% for all these angles in both myocardial infarction groups. Compared to the reference group, the rate-adjusted initial QRS|T angle in the STEMI group was 20° wider and the terminal QRS|T angle 46° narrower (p <0.001 for both). The mean QRS|T angle was not significantly different from the reference group. The initial rate-adjusted QRS|T angle in the NSTEMI group was 33° wider, the terminal angle 18° narrower, and the mean angle 22° wider than in the reference group (p <0.001 for all).
| Group | Mean Θ(QRS|T) | Initial Θ(QRS|T) | Terminal Θ(QRS|T) | |||
|---|---|---|---|---|---|---|
| Unadjusted | Adjusted ⁎ | Unadjusted | Adjusted ⁎ | Unadjusted | Adjusted ⁎ | |
| Reference | 63 (29.1) | — | 46 (26.9) | — | 113 (32.6) | — |
| ST-segment elevation myocardial infarction | 73 (36.9) | 66 (34.7) | 73 (35.2) | 66 (32.6) | 74 (41.2) | 67 (43.2) |
| Non–ST-segment elevation myocardial infarction | 95 (45.0) | 85 (42.6) | 89 (47.7) | 79 (45.3) | 106 (44.3) | 95 (45.5) |
| ST-segment elevation myocardial infarction vs reference | 10 † | 3 † | 27 ‡ | 20 ‡ | −39 ‡ | −46 ‡ |
| Non–ST-segment elevation myocardial infarction vs reference | 32 ‡ | 22 ‡ | 43 ‡ | 33 ‡ | −8 ‡ | −18 ‡ |
| Non–ST-segment elevation myocardial infarction vs ST-segment elevation myocardial infarction | 23 ‡ | 19 ‡ | 16 ‡ | 12 ‡ | 32 ‡ | 28 ‡ |
| Proportion of unadjusted spatial angle between QRS and T vectors due to heart rate (%) | ||||||
| ST-segment elevation myocardial infarction | 10 | — | 10 | — | 9 | — |
| Non–ST-segment elevation myocardial infarction | 11 | — | 11 | — | 10 | — |
⁎ Rate-adjusted Θ(QRS|T) = Θ(QRS|T) − 0.65 × (heart rate − 70).
The evaluation of the QRS|T angles during the initial and terminal repolarization revealed considerable differences among the various subgroups ( Table 3 ). The initial QRS|T angle was relatively narrow, 42° in women and 51° in men (9° wider), and it widened to 110° in women and 117° in men for terminal repolarization (p <0.001 for all). This implies that although the normal initial RS is predominantly incongruent (“reverse”) with respect to ES, it becomes predominantly congruent during terminal repolarization. The most striking of these differences was between the initial and terminal QRS|T angles in the reference group. These differences were not revealed by the mean QRS|T angle.
| Group | Mean Θ(QRS|T) ⁎ | Initial Θ(QRS|T) | Terminal Θ(QRS|T) | |||
|---|---|---|---|---|---|---|
| Mean ± SD | 5% → 95% | Mean ± SD | 5% → 95% | Mean ± SD | 5% → 95% | |
| Normal (reference) | ||||||
| Men | 71 ± 28.8 | 28 → 123 | 51 ± 26.3 | 15 → 99 | 117 ± 32.3 | 57 → 163 |
| Women | 56 ± 27.7 † | 20 → 109 | 42 ± 26.8 † | 9 → 90 | 110 ± 32.6 † | 54 → 160 |
| Myocardial infarction group | % Narrow | % wide | % Narrow | % wide | % Narrow| % wide | |||
| Men | ||||||
| ST-segment elevation myocardial infarction | 65 ± 33.1 | 13 ‡ | 3 | 66 ± 31.0 | 3 | 17 ‡ | 75 (41.4) | 51 † | 0 |
| Non–ST-segment elevation myocardial infarction | 81 ± 41.6 | 10 | 19 † | 72 ± 44.0 | 6 | 28 † | 98 (44.2) | 31 † | 2 |
| ST-segment elevation myocardial infarction vs reference | −6 ‡ | — | 15 † | −42 † | — | |
| Non–ST-segment elevation myocardial infarction vs references | 10 † | — | 22 † | — | −18 † | — |
| Women | ||||||
| ST-segment elevation myocardial infarction | 66 ± 36.3 | 6 | 13 # | 65 ± 34.2 | 2 | 23 ‡ | 54 ± 41.5 | 65 † | 0 |
| Non–ST-segment elevation myocardial infarction | 90 ± 43.8 | 5 | 39 † | 88 ± 46.1 | 3 | 50 † | 90 ± 46.8 | 37 † | 2 |
| ST-segment elevation myocardial infarction vs reference | 10 ‡ | — | 23 † | −56 † | — | |
| Non–ST-segment elevation myocardial infarction vs references | 34 † | 46 † | −20 † | — | ||
⁎ Θ(QRS/T) = QRS|T angle adjusted for heart rate (HR) 70 beats/min using formula: Θ(QRS/T)adjusted = Θ(QRS/T) − 0.65 × (HR − 70).
# p = NS; from Student’s test for mean differences between each myocardial infarction subgroup and corresponding normal gender-specific reference group and for z test comparing proportions of narrow and widened QRS|T angles separately for STEMI and NSTEMI.
Comparing the gender-specific initial QRS|T angle differences between the reference group and the myocardial infarction groups, the largest differences were observed in women, with a 23° wider initial QRS|T angle in the STEMI group and 46° wider angle in the NSTEMI group (p <0.001 for both). In contrast, the terminal QRS|T angle in women was narrower, by 56° in the STEMI group and 20° in the NSTEMI group (p <0.001 for both). Similar significant trends were observed in men, except that the difference from the reference group was not significant for the initial QRS|T angle in the NSTEMI group.
Comparing proportions of narrow and wide QRS|T angles Table 3 , the proportions of abnormally wide initial QRS|T angles were predominant in all subgroups, with prevalence ranging from 17% in STEMI group’s males to 50% in NSTEMI group’s females. In contrast, the proportion of abnormally narrow terminal QRS|T angle was predominant, with prevalence ranging from 31% in NSTEMI group’s males to 65% in STEMI group’s females. These differences between initial and terminal QRS|T angles were not evident from the proportions narrow and wide mean QRS|T angles.
An evaluation of the spatial directions of the initial and terminal T wave vectors in the reference group, with men and women combined, revealed they were contained within the normal reference zone in 95%, in the directions anterior-left, left, and inferior-left-anterior ( Figure 1 ). The distribution of the spatial orientation of the initial T vectors in the combined STEMI and NSTEMI group listed in an opened-up display of the spatial reference frame in Figure 2 shows that most (69%) of the initial T-wave vectors were contained within the normal T-wave orientation zone, depicted by the circle with a solid outline. The orientation of the deviant initial T vectors was shifted in 92% to the right of the normal zone, (circle with a broken outline), predominantly (78%) to the anterior-right, right, and inferior-right-anterior directions. This implies that the spatial direction of the deviant RS in patients with ACS was predominantly in the posterior-left, left, and superior-left-posterior directions.




