Chapter 23
Heart Failure Evaluation and Long-Term Management
Arunima Misra, MD, FACC, Kumudha Ramasubbu, MD, FACC, Shawn T. Ragbir, MD, Glenn N. Levine, MD, FACC, FAHA and Biykem Bozkurt, MD, PhD, FACC, FAHA
This chapter deals specifically with the evaluation and long-term management of patients with heart failure caused by depressed ejection fraction. The management of patients with heart failure with preserved ejection fraction (diastolic dysfunction) is discussed in Chapter 24. The management of patients with acute decompensated heart failure is discussed in Chapter 22. Specific discussions of the evaluation and management of myocarditis, dilated cardiomyopathy, hypertrophic cardiomyopathy, and restrictive/infiltrative cardiomyopathy, as well as consideration with cardiac transplantation, are discussed in other dedicated chapters in this section of the book. The roles of pacemakers and implantable cardioverter-defibrillators in patients with heart failure are discussed in this chapter, as well as in the chapters on pacemakers (Chapter 37) and implantable cardioverter-defibrillators (Chapter 38).
1. What are the most common causes of heart failure?
2. What elements should the initial assessment of the patient with heart failure include?
Initial assessment of the patient with heart failure should include:
 Evaluation of heart failure symptoms and functional capacity (dyspnea on exertion, orthopnea, paroxysmal nocturnal dyspnea [PND], fatigue, and lower extremity edema)
Evaluation of heart failure symptoms and functional capacity (dyspnea on exertion, orthopnea, paroxysmal nocturnal dyspnea [PND], fatigue, and lower extremity edema)
 Evaluation for the presence of diabetes; hypertension; smoking; prior cardiac disease; family history of cardiac disease; history of heart murmur, congenital heart disease, or rheumatic fever; sleep disturbances (obstructive sleep apnea [OSA]); thyroid disease history; exposure to infectious agents; exposure to cardiotoxins; mediastinal irradiation; and past or current use of alcohol and illicit drugs
Evaluation for the presence of diabetes; hypertension; smoking; prior cardiac disease; family history of cardiac disease; history of heart murmur, congenital heart disease, or rheumatic fever; sleep disturbances (obstructive sleep apnea [OSA]); thyroid disease history; exposure to infectious agents; exposure to cardiotoxins; mediastinal irradiation; and past or current use of alcohol and illicit drugs
 Physical examination, including heart rate and rhythm; blood pressure and orthostatic blood pressure changes; measurements of weight, height, and body mass index; overall volume status; jugular venous distension; carotid upstroke and presence or absence of bruits; lung examination for rales or effusions; cardiac examination for systolic or diastolic murmurs; displaced point of maximal impulse (PMI); presence of left ventricular heave; intensity of S2; presence of S3 or S4; liver size; presence of ascites; presence of renal bruits; presence of abdominal aortic aneurysm; peripheral edema; peripheral pulses; and checking whether the extremities are cold and clammy
Physical examination, including heart rate and rhythm; blood pressure and orthostatic blood pressure changes; measurements of weight, height, and body mass index; overall volume status; jugular venous distension; carotid upstroke and presence or absence of bruits; lung examination for rales or effusions; cardiac examination for systolic or diastolic murmurs; displaced point of maximal impulse (PMI); presence of left ventricular heave; intensity of S2; presence of S3 or S4; liver size; presence of ascites; presence of renal bruits; presence of abdominal aortic aneurysm; peripheral edema; peripheral pulses; and checking whether the extremities are cold and clammy
 Laboratory tests, including complete blood cell count (CBC), creatinine and blood urea nitrogen (BUN), serum electrolytes, natriuretic peptide (BNP or NT-proBNP), fasting blood glucose, lipid profile, liver function tests, thyroid-stimulating hormone (TSH), and urine analysis; and screening for hemochromatosis and human immunodeficiency virus (HIV), pheochromocytoma, amyloidosis, or rheumatologic diseases reasonable in selected patients, particularly if there is clinical suspicion for testing
Laboratory tests, including complete blood cell count (CBC), creatinine and blood urea nitrogen (BUN), serum electrolytes, natriuretic peptide (BNP or NT-proBNP), fasting blood glucose, lipid profile, liver function tests, thyroid-stimulating hormone (TSH), and urine analysis; and screening for hemochromatosis and human immunodeficiency virus (HIV), pheochromocytoma, amyloidosis, or rheumatologic diseases reasonable in selected patients, particularly if there is clinical suspicion for testing
 Twelve-lead electrocardiogram (ECG), assessing for rhythm, conduction abnormalities, QRS voltage and duration, QT duration, chamber enlargement, presence of ST/T changes, and Q waves
Twelve-lead electrocardiogram (ECG), assessing for rhythm, conduction abnormalities, QRS voltage and duration, QT duration, chamber enlargement, presence of ST/T changes, and Q waves
 Transthoracic echocardiogram to asses for left ventricular (LV) and right ventricular (RV) function: wall motion; chamber sizes; filling pressures; morphology of the valves; presence of ventricular hypertrophy; and diastolic parameters
Transthoracic echocardiogram to asses for left ventricular (LV) and right ventricular (RV) function: wall motion; chamber sizes; filling pressures; morphology of the valves; presence of ventricular hypertrophy; and diastolic parameters
 Consideration of ischemia workup; depending on patient’s age, history, symptoms, and ECG, this may be no workup, stress testing, or cardiac catheterization.
Consideration of ischemia workup; depending on patient’s age, history, symptoms, and ECG, this may be no workup, stress testing, or cardiac catheterization.
 Endomyocardial biopsy is not part of routine workup but can be considered in highly specific circumstances (see later).
Endomyocardial biopsy is not part of routine workup but can be considered in highly specific circumstances (see later).
 Consider cardiac MRI if infiltrative causes, such as cardiac sarcoidosis or amyloidosis, are suspected.
Consider cardiac MRI if infiltrative causes, such as cardiac sarcoidosis or amyloidosis, are suspected.
3. How are heart failure symptoms classified?
 Class I: No limitation; ordinary physical activity does not cause excess fatigue, shortness of breath, or palpitations.
Class I: No limitation; ordinary physical activity does not cause excess fatigue, shortness of breath, or palpitations.
 Class II: Slight limitation of physical activity; ordinary physical activity results in fatigue, shortness of breath, palpitations, or angina.
Class II: Slight limitation of physical activity; ordinary physical activity results in fatigue, shortness of breath, palpitations, or angina.
 Class III: Marked limitation of physical activity; ordinary activity will lead to symptoms.
Class III: Marked limitation of physical activity; ordinary activity will lead to symptoms.
 Class IV: Inability to carry on any physical activity without discomfort; symptoms of congestive heart failure (CHF) are present even at rest; increased discomfort is experienced with any physical activity.
Class IV: Inability to carry on any physical activity without discomfort; symptoms of congestive heart failure (CHF) are present even at rest; increased discomfort is experienced with any physical activity.
4. What is the stage system for classifying heart failure?
In 2001, the American College of Cardiology/American Heart Association (ACC/AHA) introduced a system to categorize the stages of heart failure. This system is somewhat different in focus than the previous NYHA classification system and was intended, in part, to emphasize the prevention of the development of symptomatic heart failure. In addition, the 2009 update on the 2005 Heart Failure Guidelines suggest appropriate therapy for each stage (Figure 23-1).
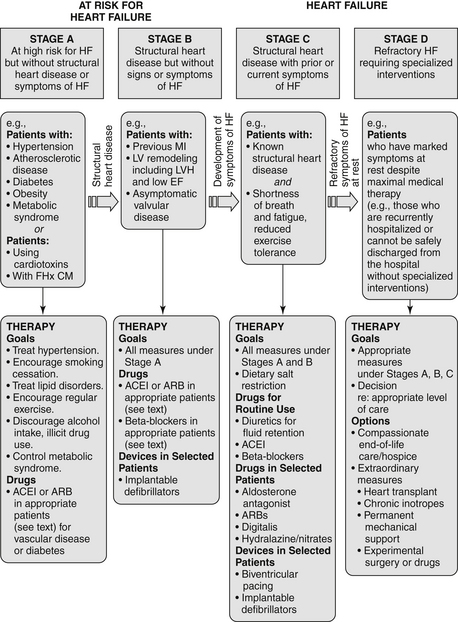
Figure 23-1 American College of Cardiology/American Heart Association Stages in the Development of Heart Failure/Recommended Therapy by Stage. (From Jessup M, Abraham WT, Casey DE, et al: ACC/AHA 2009 focused update: ACCF/AHA guidelines for the diagnosis and management of heart failure in adults : a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: Developed in collaboration with the International Society for Heart and Lung Transplantation, Circulation 119:1977-2016, 2009; originally published online March 26, 2009.) ACEI, Angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; EF, ejection fraction; FHx CM, family history of cardiomyopathy; HF, heart failure; LV, left ventricle; LVH, left ventricular hypertrophy; MI, myocardial infarction.
 Stage A: Patient is at high risk for developing heart failure but is without structural heart disease or symptoms of heart failure. Includes patients with hypertension, coronary artery disease (CAD), obesity, diabetes, history of drug or alcohol abuse, history of rheumatic fever, family history of cardiomyopathy, or treatment with cardiotoxins
Stage A: Patient is at high risk for developing heart failure but is without structural heart disease or symptoms of heart failure. Includes patients with hypertension, coronary artery disease (CAD), obesity, diabetes, history of drug or alcohol abuse, history of rheumatic fever, family history of cardiomyopathy, or treatment with cardiotoxins
 Stage B: Patient with structural heart disease but is without signs or symptoms of heart failure. Includes patients with previous myocardial infarction (MI), LV remodeling (including left ventricular hypertrophy [LVH] or low ejection fraction), or asymptomatic valvular disease
Stage B: Patient with structural heart disease but is without signs or symptoms of heart failure. Includes patients with previous myocardial infarction (MI), LV remodeling (including left ventricular hypertrophy [LVH] or low ejection fraction), or asymptomatic valvular disease
 Stage C: Patient with structural heart disease and with prior or current symptoms of heart failure
Stage C: Patient with structural heart disease and with prior or current symptoms of heart failure
 Stage D: Patient with refractory heart failure requiring specialized interventions
Stage D: Patient with refractory heart failure requiring specialized interventions
5. Which patients with heart failure should be considered for endomyocardial biopsy (EMB)?
In 2007, the ACC/AHA/European College of Cardiology (ACC/AHA/ECC) issued a scientific statement on the role of EMB. Most patients who are seen for heart failure should not be referred for EMB. Biopsy results are often nonspecific or unrevealing, and in most cases there is no specific therapy based on biopsy results that have been shown to improve prognosis. However, in certain clinical scenarios, EMB should be performed (class I recommendation) or can be considered and is considered reasonable (class IIa recommendation). As given in that document, these scenarios include the following:
 New-onset heart failure of less than 2 weeks duration associated with a normal-sized or dilated left ventricle and hemodynamic compromise (class I; level of evidence B)
New-onset heart failure of less than 2 weeks duration associated with a normal-sized or dilated left ventricle and hemodynamic compromise (class I; level of evidence B)
 New-onset heart failure of 2 weeks to 3 months duration associated with a dilated left ventricle and new ventricular arrhythmias, second- or third-degree heart block, or failure to respond to usual care within 1 to 2 weeks (class I; level of evidence B)
New-onset heart failure of 2 weeks to 3 months duration associated with a dilated left ventricle and new ventricular arrhythmias, second- or third-degree heart block, or failure to respond to usual care within 1 to 2 weeks (class I; level of evidence B)
 Heart failure of more than 3 months duration associated with a dilated left ventricle and new ventricular arrhythmias, second- or third-degree heart block, or failure to respond to usual care within 1 to 2 weeks (class IIa; level of evidence C)
Heart failure of more than 3 months duration associated with a dilated left ventricle and new ventricular arrhythmias, second- or third-degree heart block, or failure to respond to usual care within 1 to 2 weeks (class IIa; level of evidence C)
 Heart failure associated with a dilated cardiomyopathy of any duration associated with suspected allergic reaction or eosinophilia (class IIa; level of evidence C)
Heart failure associated with a dilated cardiomyopathy of any duration associated with suspected allergic reaction or eosinophilia (class IIa; level of evidence C)
 Heart failure associated with suspected anthracycline cardiomyopathy (class Ia; level of evidence C)
Heart failure associated with suspected anthracycline cardiomyopathy (class Ia; level of evidence C)
 Heart failure with unexplained restrictive cardiomyopathy (class IIa; level of evidence C)
Heart failure with unexplained restrictive cardiomyopathy (class IIa; level of evidence C)
6. What are the general treatments for patients with heart failure?
 Diuretics are indicated for volume overload. Starting doses of furosemide are often 20 to 40 mg once or twice a day, but higher doses will be required in patients with significant renal dysfunction. The dose should be uptitrated to a maximum of up to 600 mg daily in divided doses. Failure of therapy is often the result of inadequate diuretic dosing. Torsemide is more expensive than furosemide but has superior absorption and longer duration of action. Bumetanide is approximately 40 times more potent milligram-for-milligram than furosemide and can also be used in patients who are unresponsive or poorly responsive to furosemide. Synergistic diuretics that act on the distal portion of the tubule (thiazides such as metolazone, or potassium-sparing agents) are often added in those who fail to respond to high-dose loop diuretics alone. In addition, a new recommendation from 2009 Focused Update states that for hospitalized heart failure patients, if diuresis is inadequate to relieve congestion, higher doses of loop diuretics should be used, addition of second diuretic should be made or continuous infusion of a loop diuretic should be considered.
Diuretics are indicated for volume overload. Starting doses of furosemide are often 20 to 40 mg once or twice a day, but higher doses will be required in patients with significant renal dysfunction. The dose should be uptitrated to a maximum of up to 600 mg daily in divided doses. Failure of therapy is often the result of inadequate diuretic dosing. Torsemide is more expensive than furosemide but has superior absorption and longer duration of action. Bumetanide is approximately 40 times more potent milligram-for-milligram than furosemide and can also be used in patients who are unresponsive or poorly responsive to furosemide. Synergistic diuretics that act on the distal portion of the tubule (thiazides such as metolazone, or potassium-sparing agents) are often added in those who fail to respond to high-dose loop diuretics alone. In addition, a new recommendation from 2009 Focused Update states that for hospitalized heart failure patients, if diuresis is inadequate to relieve congestion, higher doses of loop diuretics should be used, addition of second diuretic should be made or continuous infusion of a loop diuretic should be considered.
 Inhibition of the renin-angiotensin-aldosterone system should be initiated. Angiotensin-converting enzyme (ACE) inhibitors are first-line agents in those with depressed ejection fraction because they have been convincingly shown to improve symptoms, decrease hospitalizations, and reduce mortality. Angiotensin II receptor blockers (ARBs) are used in those who are ACE-inhibitor intolerant because of persistent cough. ARBs may also be considered in addition to ACE inhibitors in select patients (this latter decision is best left to a heart failure specialist). The aldosterone antagonists spironolactone or eplerenone can be considered as additional therapy in carefully selected patients with preserved renal function already on standard heart failure therapies.
Inhibition of the renin-angiotensin-aldosterone system should be initiated. Angiotensin-converting enzyme (ACE) inhibitors are first-line agents in those with depressed ejection fraction because they have been convincingly shown to improve symptoms, decrease hospitalizations, and reduce mortality. Angiotensin II receptor blockers (ARBs) are used in those who are ACE-inhibitor intolerant because of persistent cough. ARBs may also be considered in addition to ACE inhibitors in select patients (this latter decision is best left to a heart failure specialist). The aldosterone antagonists spironolactone or eplerenone can be considered as additional therapy in carefully selected patients with preserved renal function already on standard heart failure therapies.
 Hydralazine and isosorbide are used in patients who are unable to tolerate both ACE inhibitors and ARBs because of renal failure. Hydralazine and isosorbide should be considered in addition to an ACE inhibitor or ARB in African Americans, and can be considered as an add-on therapy in others. They may be considered in patients who are ACE inhibitor and ARB intolerant.
Hydralazine and isosorbide are used in patients who are unable to tolerate both ACE inhibitors and ARBs because of renal failure. Hydralazine and isosorbide should be considered in addition to an ACE inhibitor or ARB in African Americans, and can be considered as an add-on therapy in others. They may be considered in patients who are ACE inhibitor and ARB intolerant.
 The beta-adrenergic blocking agents (β-blockers) metoprolol succinate (Toprol XL), carvedilol (Coreg), and bisoprolol have been shown to decrease mortality in appropriately selected patients. These agents should be initiated in euvolemic patients on stable background heart failure therapy, including ACE inhibitors or ARBs.
The beta-adrenergic blocking agents (β-blockers) metoprolol succinate (Toprol XL), carvedilol (Coreg), and bisoprolol have been shown to decrease mortality in appropriately selected patients. These agents should be initiated in euvolemic patients on stable background heart failure therapy, including ACE inhibitors or ARBs.
 Implantable cardioverter-defibrillators (ICDs) are considered for primary prevention in patients whose ejection fractions remain less than 30% to 35% despite optimal medical therapy, and who have a good-quality life expectancy of at least 1 year.
Implantable cardioverter-defibrillators (ICDs) are considered for primary prevention in patients whose ejection fractions remain less than 30% to 35% despite optimal medical therapy, and who have a good-quality life expectancy of at least 1 year.
 Biventricular pacing for resynchronization therapy should be considered. According to the 2009 American College of Cardiology Foundation/AHA (ACCF/AHA) guidelines, biventricular pacing for cardiac resynchronization therapy (CRT) should be considered for patients in sinus rhythm with NYHA class III-IV symptoms, left ventricular ejection fraction (LVEF) less than 35%, and QRS greater than 120 ms. Consultation with an electrophysiologist is recommended.
Biventricular pacing for resynchronization therapy should be considered. According to the 2009 American College of Cardiology Foundation/AHA (ACCF/AHA) guidelines, biventricular pacing for cardiac resynchronization therapy (CRT) should be considered for patients in sinus rhythm with NYHA class III-IV symptoms, left ventricular ejection fraction (LVEF) less than 35%, and QRS greater than 120 ms. Consultation with an electrophysiologist is recommended.
The elements of long-term management of patients with CHF resulting from depressed LV systolic function are summarized in Table 23-1.
TABLE 23-1
ELEMENTS OF THE LONG-TERM MANAGEMENT OF PATIENTS WITH CONGESTIVE HEART FAILURE DUE TO LEFT VENTRICULAR SYSTOLIC DYSFUNCTION
| Treatment/Intervention | Recommendation (Level of Evidence) |
| Diuretics for fluid retention | Class I (LOE: C) |
| Salt restriction | Class I (LOE: C) |
| ACE inhibitors (ACEIs) | Class I (LOE: A) |
| Angiotensin II receptor blockers (ARB) in ACEI-intolerant patients | Class I (LOE: A) |
| ARB in persistently symptomatic patients with reduced LVEF already being treated with conventional therapy | Class IIb (LOE: C) |
| Hydralazine + Isosorbide in patients ACEI and ARB intolerant | Class IIb (LOE: C) |
| Hydralazine + Isosorbide in patients already on ACEI and β-blocker with persistent symptoms | Class IIa (LOE: A) |




