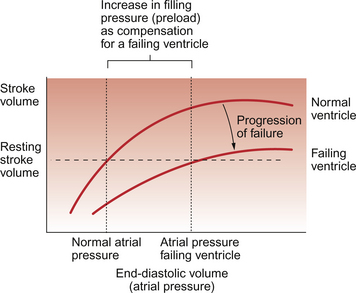
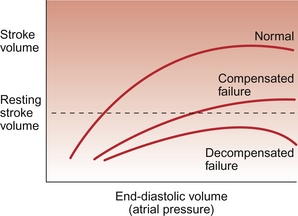
6 The typical ‘textbook person’ at rest has a cardiac output of about 5 L/min (see Chapter 4). The key physiological variables determining cardiac output are grouped as follows: • preload events (filling pressure of the ventricle) • contractility events (events inside the myocyte particularly associated with [Ca++] and [H+]) • afterload events (the resistance to blood leaving the heart) The first three items on this list determine the stroke volume of each ventricle and the heart rate is primarily regulated by the baroreceptor reflex which keeps arterial blood pressure quite constant (see Chapter 9). In Case 6.1:1 the history is outlined of a 37-year-old man who finds that his exercise capacity is becoming limited. In general the causes of heart failure can be attributed to one or more of the following: • decreased myocyte contractility • inappropriate workload due to pressure overload (e.g. hypertension causing increased afterload) or volume overload (increased preload) Heart failure may result from functional changes affecting either systole or diastole or both. Table 6.1 summarizes some of the key differences between systolic and diastolic heart failure. Examples of these different forms of cardiac failure are: Table 6.1 Some characteristic differences between systolic and diastolic heart failure It is widely thought that cardiac myocytes cannot proliferate, only change size and shape. Some recent reports however suggest limited myocyte division is possible after myocardial infarction. In eccentric hypertrophy extra sarcomeres (see Fig. 2.1) are added in series and so myocyte length increases leading to a dilated heart. In concentric hypertrophy extra sarcomeres are added in parallel and so myocyte diameter increases. • Mainly systolic dysfunction: • Mainly diastolic dysfunction: • Mixed systolic/diastolic dysfunction: If the degree of functional impairment of the heart is relatively small then at rest the ventricle may be able to maintain a normal stroke volume and hence a normal cardiac output. This is achieved by an increase in filling pressure of the ventricle and hence an increase in end-diastolic volume. This increase in ‘preload’ causes the impaired ventricular function to move up a Starling curve (see Chapter 4) to reach a normal stroke volume (Fig. 6.1). There is however a limitation on the ability to increase stroke volume above the resting levels. This manifests itself as part of the exercise limitation experienced by heart failure patients. The increase in preload to restore resting stroke volume for a damaged heart to normal levels is referred to as ‘compensation’. The extent to which compensation can occur is limited by the shape of the cardiac function curve. If end-diastolic volume increases too much then a plateau is reached when further increases in end-diastolic volume do not produce a corresponding increase in the force of contraction of the ventricle. If the cardiac output is still inadequate when this plateau region is reached then end-diastolic volume may continue to increase and this will eventually cause the force of contraction to decrease. This is the region of ‘decompensation’ on the Starling curve and may rapidly lead to death (Fig. 6.2). Fig. 6.2 Decompensated cardiac failure. In compensated cardiac failure the resting stroke volume and therefore resting cardiac output can reach normal levels by virtue of an increase in filling pressure (preload) for the ventricle (see Fig. 6.1). In decompensated failure increases in preload fail to achieve a satisfactory cardiac output and further increases may lead to a decline in stroke volume. The commonest form of heart failure is left ventricle systolic failure. It has an annual mortality rate of 15–30% depending on disease severity. In pure left heart failure, the healthy right ventricle will continue to pump blood into the lungs until left ventricular preload is increased enough to restore ventricular balance, i.e. the same output from the two sides of the heart. This ventricular balance will be achieved at the price of raised left atrial, pulmonary capillary and pulmonary artery pressures. The raised pulmonary capillary pressure may result in pulmonary oedema (see Chapter 11) and this will cause the lungs to become ‘stiff’. There will be an increased resistance to inflation of the lungs (a decreased compliance) and this will produce a sensation of breathlessness (dyspnoea). The pulmonary oedema may also upset the balance between the distribution of lung ventilation and pulmonary blood flow causing a ‘ventilation-perfusion mismatch’ which will result in arterial hypoxaemia. This in turn will further reduce the delivery of oxygen to the heart and potentially exacerbate heart failure, producing a vicious circle of events.
HEART FAILURE
Systolic vs diastolic failure
Systolic heart failure
Diastolic heart failure
Systolic BP
Low normal; hypertension
Low normal; hypertension
End-diastolic volume
↑↑
Normal or ↓
End-systolic volume
↑↑
↓
Stroke volume
Normal or ↓
Normal or ↓
Ejection fraction
↓↓
Normal
Myocardial hypertrophy
Eccentric
Concentric
LV wall thickness
↓
↑↑
Extracellular matrix
↓
↑↑
Haemodynamic events
Haemodynamic events in systolic heart failure
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


HEART FAILURE