Heart failure In A Heartbeat
Epidemiology | Prevalence and incidence increase with age |
Aetiology | Commonly caused by other cardiac diseases |
Clinical features | Symptoms: dyspnoea, orthopnoea, PND, nocturnal cough, chest discomfort, fatigue |
Investigations | In all patients: blood tests (i.e. FBC, U&Es, LFTs, albumin, TSH if new patient, Mg/Ca if arrhythmias, BNP, cardiomyopathy screen if indicated (see Chapter 14)), CXR, ECG, echocardiography |
Management |
|
10.2 Definition
Heart failure refers to the inability of the heart to produce a cardiac output sufficient to meet the metabolic demands of the body.
10.3 Epidemiology
- More common in developed countries
- Affects approximately 900 000 people in the UK
- Prevalence and incidence increase with age
- 7% of people aged 75–84 have some degree of heart failure, with the figures rising to 20% in those above 85 years of age
- Risk factors include old age, male sex, smoking, obesity, coronary heart disease, hypertension, family history and diabetes.
10.4 Aetiology
EXAM | The three most common causes of heart failure are ischaemic heart disease, valvular heart disease, dilated cardiomyopathy and hypertension. Coronary artery disease is the most common cause in the Western world. |
The aetiology of heart failure can be approached in the following way:
- Myocardial dysfunction
- ischaemic heart disease
- hypertension
- dilated cardiomyopathy
- myocarditis
- ischaemic heart disease
- Outflow obstruction
- aortic stenosis
- hypertension
- aortic stenosis
- Ventricular overload
- aortic regurgitation
- mitral regurgitation
- congenital anomalies – ventricular septal defect
- aortic regurgitation
- Impaired ventricular filling
- pericardial tamponade
- restrictive cardiomyopathy
- constrictive pericarditis
- pericardial tamponade
- Rarer causes (<1%): diseases that result in a higher cardiac output
- severe anaemia
- hyperthyroidism
- beriberi (thiamine deficiency)
- pregnancy
- severe anaemia
10.5 Pathophysiology
The pathophysiological process that takes place in heart failure involves a complex interplay of many factors. As cardiac output begins to decline, compensatory mechanisms (both mechanical and neurohumoral in nature) are activated in an attempt to sustain adequate tissue perfusion. However, while these mechanisms may initially be beneficial, they eventually lead to worsening of heart failure over time as they decline in their ability to compensate.
10.5.1 Mechanical adaptations
Frank–Starling Law
- As myocardial contractility declines, stroke volume reduces as a consequence
- This results in an increased end diastolic volume (EDV) due to incomplete emptying of the ventricles during systole
- The myocardial fibres are subsequently stretched, increasing the stroke volume in the following contraction in order to generate sufficient cardiac output
// Why? //
Myocyte sarcomere length increases as the fibres stretch, producing a greater force of contraction as blood is expelled from the ventricle.
- Eventually, this process results in ventricular remodelling, increased wall stress and reduced cardiac output as this mechanism fails.
10.5.2 Neurohumoral adaptations
Activation of sympathetic nervous system (SNS)
- As cardiac output declines, there is early activation of the SNS
- Sympathetic activation causes tachycardia, increased sodium and fluid reabsorption by the kidney and increased peripheral vascular resistance.
Activation of renin-angiotensin-aldosterone system (RAAS) (refer to Chapter 1)
- In heart failure, activation of the RAAS is a late compensatory mechanism
- This is mediated primarily by angiotensin II
- The actions of angiotensin II aim to achieve adequate tissue perfusion by attempting to increase cardiac output
- Over time, the actions of angiotensin II increase the preload and afterload
- As the heart tries to cope with the increased workload in order to achieve adequate tissue perfusion, further activation of the RAAS leads to a vicious cycle of fluid overload and worsening wall stress
// Why? //
RAAS activation results in a series of changes that initially aim to maintain adequate tissue perfusion. This eventually places further strain on the heart.
Effects of angiotensin II:
Increased sympathetic activity – increases heart rate and contractility
Arteriolar vasoconstriction – increases systemic vascular resistance and afterload
Aldosterone activation – causes sodium reabsorption and subsequent increase in preload
ADH activation – causes water retention and subsequent increase in preload.
- Persistently high angiotensin II eventually causes fibrosis of the heart and kidneys, promoting remodelling of the heart and further activation of the SNS.
10.6 Types of heart failure
For ease of reference, heart failure can be classified according to anatomical, functional and temporal features. These are further detailed in Tables 10.1–10.3.
Table 10.1 – Anatomical features of heart failure
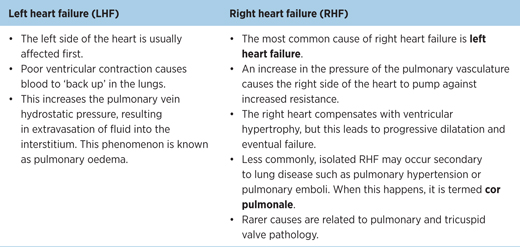
Table 10.2 – Functional features of heart failure
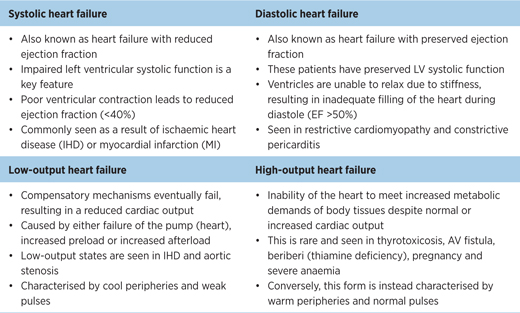
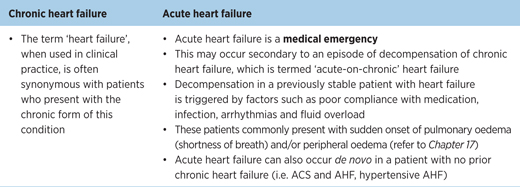
Table 10.3 – Temporal features of heart failure
The combination of left and right heart failure is known as congestive heart failure. Congestive heart failure is the most common presentation in clinical practice.
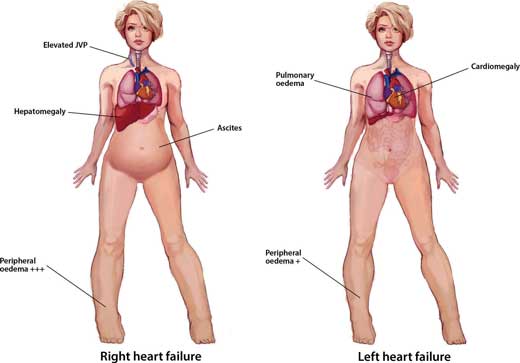
Figure 10.1 – Signs of right heart failure and left heart failure.
// PRO-TIP //
Neither low- nor high-output heart failure meets the metabolic demands of body tissues. In this case, ‘high-output’ is somewhat of a misnomer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


