Chapter 19 Heart Failure
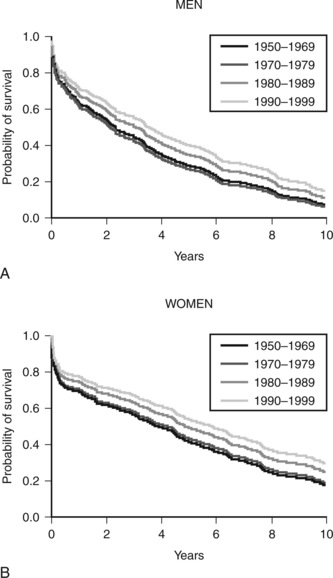
Heart failure is a clinical syndrome that occurs as the end result of any structural or functional cardiac disorder that impairs the ability of the ventricles to fill with or eject blood. In Western countries coronary artery disease and hypertension are its most common causes. In the United States heart failure affects more than 5 million people and results in significant impairment of quality of life, frequent hospitalizations, and poor long-term survival rates (Fig. 19-1).1 The number of deaths from heart failure is increasing despite advances in diagnosis and treatment. This increase is due in part to an aging population and to improved survival after acute myocardial infarction.2
ACUTE HEART FAILURE
Pathophysiology
Impaired left ventricular function leads to increased left ventricular end-diastolic pressure (LVEDP) and reduced stroke volume. Increased LVEDP causes increased pulmonary capillary hydrostatic pressure, which results in the increased filtration of protein-poor fluid into the pulmonary interstitium (Equation 1-12). Moderately increased left atrial pressure (18 to 25 mmHg) results in interstitial edema, which is defined as fluid accumulation in the peribronchovascular spaces; severely increased left atrial pressure (>25 mmHg) results in alveolar edema, which is defined as fluid accumulation in the alveoli.3 Interstitial edema reduces lung compliance and leads to increased work of breathing. Alveolar edema causes increased work of breathing and intrapulmonary shunting, leading to hypoxemia. Acute pulmonary edema can occur in the absence of increased circulating volume or pathologic fluid retention.
Systemic hypoperfusion leads to lactic acidosis and oliguric renal failure. Severe acidemia aggravates myocardial dysfunction, whereas renal dysfunction exacerbates fluid retention. Over a period of days fluid retention leads to elevated systemic venous pressure and dependent edema, even in the absence of right ventricular dysfunction. Catecholamines and other substances that evolve during cardiogenic shock have important effects on intermediary metabolism (see Chapter 2) that result in hyperglycemia, lipolysis, and increased protein catabolism.
Systemic inflammation also occurs with heart failure, cardiogenic shock, and cardiac arrest. Patients with severe heart failure have increased levels of inducible nitric oxide synthetase and various inflammatory cytokines, such as tumor necrosis factor-α and interleukins 1 and 6.4 The inducible form of nitric oxide synthetase is involved in the regulation of vascular tone in various disease states and, along with tumor necrosis factor-α, it mediates myocardial depression. In patients resuscitated from cardiac arrest, systemic inflammation may produce a hemodynamic state that resembles septic shock, with pathologic vasodilation and capillary leak.5 In addition, there is commonly fever, leukocytosis, and elevations in acute-phase reactants.
Based on a simple pump-failure model of cardiogenic shock, patients would be expected to have profoundly depressed ventricular function (i.e., ejection fraction <20%) and elevated systemic vascular resistance. However, many of the patients with cardiogenic shock in the SHOCK trial registry (see later discussion) did not have elevated systemic vascular resistance, and their average ejection fraction was 30%—that is, only moderate to severely depressed.6 These findings may be explained as being a severe systemic inflammatory response to myocardial infarction, shock, and cardiac arrest.
Classification and Clinical Presentation
Acute heart failure may be classified on the basis of the presenting clinical syndrome, the hemodynamic profile, and the severity of symptoms. The European Society of Cardiology system recognizes clinical syndromes7: (1) mild acute decompensated heart failure characterized by fluid overload with or without hypoperfusion; (2) hypertensive acute heart failure in which there is hypertension, preserved left ventricular systolic function, and acute pulmonary edema; (3) acute heart failure with pulmonary edema; (4) cardiogenic shock; (5) high output failure; (6) right heart failure. Acute heart failure may also be classified on the basis of hemodynamic profile. Patients are categorized as “warm” or “cold” on the basis of their systemic perfusion and as “wet” or “dry” on the basis of the presence of congestion (either systemic or pulmonary). Class I is warm and dry, Class II is warm and wet, Class III is cold and dry, and Class IV is cold and wet. After myocardial infarction, the Killip classification is widely used for grading heart failure (Table 19-1).8
Table 19-1 Killip Classification of Heart Failure Following Myocardial Infarction
| Class I | No signs of heart failure |
|---|---|
| Class II | Crackles, S3 gallop, elevated jugular venous pressure |
| Class III | Pulmonary edema |
| Class IV | Cardiogenic shock |
From Killip T 3rd, Kimball JT: Treatment of myocardial infarction in a coronary care unit: a two-year experience with 250 patients. Am J Cardiol 20:457-464, 1967.
Pulmonary Edema
Pulmonary edema may be cardiogenic or noncardiogenic. A pulmonary artery wedge pressure (PAWP) greater than 18 mmHg defines cardiogenic pulmonary edema. Pulmonary edema that occurs following a myocardial infarction is typically due to left ventricular systolic dysfunction. It may or may not be associated with systemic hypoperfusion. In contrast, “flash” pulmonary edema is commonly associated with preserved systolic function,9,10 and the trigger for decompensation is often diastolic dysfunction secondary to a hypertensive crisis.9 Other causes of cardiogenic pulmonary edema include acute aortic and mitral valve disease, arrhythmias, atrial myxoma, and high-output states, such as anemia and thyrotoxicosis.
Cardiogenic Shock
Cardiogenic shock is hypotension (systolic blood pressure below 90 mmHg for more than 30 minutes or systolic blood pressure above 90 mmHg with vasoactive support) in association with tissue hypoperfusion or, if a pulmonary artery catheter (PAC) is in situ, a cardiac output of less than 2.2 l/min/m2.11
The main cause of cardiogenic shock is left ventricular systolic dysfunction secondary to acute STEMI. Cardiogenic shock occurs in about 4% of patients following STEMI.12 Risk factors for cardiogenic shock include extensive infarction, anterior infarction, previous myocardial infarction, low ejection fraction, and multivessel coronary artery disease. Shock is more common in myocardial infarctions that occur in the elderly, in diabetics, and in patients who have histories of cerebral or peripheral vascular disease. Only very rarely does cardiogenic shock develop following non-ST-segment elevation myocardial infarction. Most patients who develop cardiogenic shock do so within 24 hours of the myocardial infarction. In the trial known as should we emergently revascularize Occluded Coronaries in cardiogenic shock (the SHOCK trial; see subsequent discussion), 11% of patients had shock at the time of hospital admission and 75% had developed shock by 24 hours.11
Shock that occurs beyond 24 hours should raise the possibility of a mechanical complication of myocardial infarction, such as papillary muscle rupture, ventricular septal rupture, or ventricular free wall rupture. Another cause of shock following myocardial infarction is right ventricular failure. Approximately 25% of patients with inferior myocardial infarction have right ventricular infarction,13 and a proportion of these patients develop right ventricular failure. Cardiogenic shock can also occur for reasons unrelated to myocardial infarction, such as pericardial tamponade, fulminant myocarditis, or acute valvular dysfunction.
Clinical signs of tissue hypoperfusion include cool clammy skin, peripheral cyanosis, oliguria, tachycardia, confusion, and drowsiness. Patients with right ventricular failure may have distended neck veins with visible pulsations (V waves; see Figure 8-11) that are indicative of tricuspid regurgitation. Biochemical abnormalities include hyperglycemia, lactic acidosis, increased blood urea nitrogen and creatinine, and elevations in hepatic transaminases.
Cardiac arrest, typically ventricular fibrillation, occurs in about 3% of patients with STEMI12 and may be the presenting feature. At least 25% of patients who subsequently develop cardiogenic shock will have had a cardiac arrest, usually at presentation.11 Following cardiac arrest, patients may suffer hypoxic ischemic encephalopathy (HIE; see Chapter 37). Cardiogenic shock is the leading cause of death after acute myocardial infarction and is an important cause of multiple organ dysfunction syndrome (MODS).
Diagnosis
The diagnosis of acute heart failure rests on clinical assessment, electrocardiography, chest radiography, echocardiography, and laboratory tests. Diagnostic assessment should be directed at confirming the diagnosis of heart failure and identifying the cause. The differential diagnoses of pulmonary edema and cardiogenic shock are listed in Table 19-2.
Table 19-2 Differential Diagnosis of Noncardiogenic Pulmonary Edema and Cardiogenic Shock
| Pulmonary Edema Without Shock |
| ARDS |
| Transfusion-related acute lung injury |
| Neurogenic pulmonary edema |
| Cardiogenic Shock |
| Massive pulmonary embolism |
| Occult hypovolemic shock |
| Septic-shock-induced severe myocardial depression |
| Anaphylaxis |
| Aortic dissection with tamponade and/or acute aortic regurgitation |
| Pericardial tamponade (e.g., due to malignant effusion) |
| Mechanical complication of myocardial infarction: |
| Acute mitral regurgitation |
| Ventricular septal rupture |
| Ventricular free wall rupture |
ARDS, acute respiratory distress syndrome.
Clinical Assessment
Symptoms are generally nondiscriminatory. An exception is a history of paroxysmal nocturnal dyspnea, which implies a cardiac cause for shortness of breath. Risk factors for and a previous history of coronary artery disease should be sought. Chest pain may be suggestive of myocardial infarction or point to another diagnosis (see Table 18-4). Systemic conditions that are associated with heart failure, such as collagen vascular diseases, pregnancy, and thyrotoxicosis, may be identified. Features suggestive of acute cardiomyopathy are outlined subsequently.
On physical examination, the finding of an S3 gallop is a specific, but insensitive, sign of heart failure.14 Both S3 gallop and an elevated jugular venous pressure are independently associated with adverse outcome.15 Crackles and wheezes are common but nondiscriminatory. A murmur may indicate valvular dysfunction or a mechanical complication of myocardial infarction.
Electrocardiogram and Chest Radiograph
On the chest radiograph, useful information is obtained from the cardiac silhouette and the pulmonary vasculature. With de novo heart failure, cardiac size is not enlarged. Thus, an enlarged cardiac silhouette indicates a chronic process or a pericardial collection. The shape of the cardiac contour may be useful in differentiating a pericardial fluid collection from left or right ventricular dilatation. Features suggestive of a specific valve abnormality, such as mitral stenosis, may be apparent. The chest radiograph may demonstrate interstitial or alveolar edema (see Chapter 6). Features suggestive of a cardiogenic cause may also be apparent (see Table 27-5). Radiographic signs of pulmonary edema may develop very rapidly but their resolution lags behind clinical recovery, often by several days.
Echocardiography
Echocardiography is the single most useful test in the evaluation of patients with heart failure.2 Two-dimensional and Doppler imaging allows for the evaluation of global and regional left ventricular systolic function, left ventricular diastolic function, right ventricular function, and valvular function. Uncommon conditions such as constrictive pericarditis, pericardial tamponade, congenital heart disease, and restrictive or obstructive cardiomyopathy may be identified. In most circumstances, transthoracic echocardiography (TTE) is adequate, although transesophageal echocardiography may be required in patients who are mechanically ventilated because image quality is often poor with TTE.16
Laboratory Tests
The plasma level of BNP is elevated in patients with raised LVEDP and may be used to help determine the cause of acute dyspnea. Heart failure is “very improbable” when the plasma BNP concentration is below 100 pg/ml and “very probable” when it is above 500 pg/ml; when accompanied by a history of heart failure or strong clinical suspicion, heart failure is “very probable” when the BNP concentration is between 100 and 500 pg/ml.17 However, BNP levels must be interpreted with caution because they also are elevated in a range of other conditions encountered in the ICU, such as aortic stenosis,18 pulmonary embolus,19 cardiac surgery sequelae,20 septic shock,21–23 and acute respiratory distress syndrome.24 BNP levels are commonly elevated above 500 pg/ml in patients who are critically unwell, independent of any cardiac dysfunction.23 BNP levels are also increased in renal failure, and a cutoff value of 200 pg/ml to exclude heart failure is recommended when the glomerular filtration rate is less than 60 ml/min.17 Conversely, BNP levels may be normal at the time of admission in patients with flash pulmonary edema.
As an alternative to BNP, the plasma concentration of N-BNP, the N-terminus of pro-BNP, may be used, in which case the recommended lower cutoff value to exclude heart failure is 125 pg/ml in patients younger than 75 years of age and 450 pg/ml in patients older than 75 years.17 An elevated troponin level supports a diagnosis of myocardial infarction but, as with BNP, elevated troponin levels can occur in a range of conditions (see Table 18-7) other than acute coronary syndromes.
Features Suggestive of Acute Cardiomyopathy
Severe acute heart failure is occasionally caused by cardiomyopathy. The diagnosis is suggested by the abrupt onset of severe biventricular failure in a young patient in association with ventricular arrhythmias and widespread repolarization (ST segment) abnormalities on the ECG. A history of recent viral illness or drug ingestion (e.g., alcohol, cocaine, antiretroviral drugs, doxorubicin) suggests the diagnosis. The main differential diagnosis is myocardial ischemia and infarction. Biventricular involvement and a normal coronary angiogram are strongly suggestive of acute cardiomyopathy. The diagnosis may be confirmed by right ventricular endomyocardial biopsy.
Management of Acute Heart Failure
The management of acute severe heart failure involves:
Treatment of Acute Pulmonary Edema
Pharmacotherapy
Pharmacotherapy25 for acute pulmonary edema consists of diuretics, morphine, and vasodilators. Intravenous furosemide is the most commonly used initial therapy for acute heart failure,26 and it provides relief from pulmonary congestion. Furosemide must be used with caution because it can cause hypokalemia, hypomagnesemia, hypovolemia, and renal dysfunction. Morphine reduces the sensation of dyspnea and acts as a weak vasodilator, thereby reducing preload and afterload. Morphine must be used cautiously in patients with low cardiac output or reduced level of consciousness. Small intravenous boluses (1 to 3 mg) should be titrated to effect.
Venodilatation decreases systemic venous return and therefore reduces left ventricular preload, whereas arteriolar dilatation reduces left ventricular afterload. Both effects reduce left atrial pressure. Intravenous nitroglycerin dilates both veins and arterioles and is useful for treating cardiogenic pulmonary edema. Higher doses (>1 μg/kg/min) than are required to treat angina may be needed. Nitroprusside, a potent arteriolar dilator, is also effective in reducing left atrial pressure but can cause marked hypotension, even at low doses. It is particularly useful in patients with acute pulmonary edema secondary to hypertensive crisis. It should be administered only to patients with invasive blood pressure monitoring. Nesiritide, an analogue of BNP, is a mixed vein and arteriole vasodilator that has a mild diuretic effect.27 In patients with acute heart failure, nesiritide is more effective than nitroglycerin in improving symptoms and reducing left atrial pressure.28,29 Vasodilators should be avoided in patients with cardiogenic shock.
Ventilatory Support
Patients with persistent hypoxemia (SaO2 <90%) or marked respiratory distress despite high-flow face-mask oxygen should be given continuous positive airways pressure (CPAP), which is administered by using a tight-fitting face mask. CPAP increases functional residual capacity, reduces work of breathing, improves oxygenation, and reduces left ventricular afterload. Initial CPAP settings of 10 cm H2O with 100% oxygen are appropriate. The inspired oxygen concentration should be titrated to achieve an SaO2 above 90% with a stable arterial carbon dioxide tension and pH. Patients should be closely monitored for deteriorating hemodynamics, worsening gas exchange, and exhaustion. Criteria for endotracheal intubation are outlined in Table 27-3.
If endotracheal intubation is required, it may be fraught with problems for two reasons. First, copious quantities of frothy edema fluid may fill the pharynx, making laryngoscopy extremely difficult. If this occurs, an assistant can place the tip of a suction catheter directly into the laryngeal inlet during laryngoscopy to allow visualization of the vocal cords. Second, the loss of sympathetic tone associated with general anesthesia may precipitate severe hypotension. Vasopressors should be drawn up in preparation for this state. Invasive ventilation for patients with acute pulmonary edema is described in Chapter 29.
Treatment of Hypoperfusion and Shock
Monitoring and Investigations
In addition to the monitors listed earlier, a central venous catheter should be placed in patients with cardiogenic shock to measure central venous pressure and superior vena caval oxygen saturation (SSVCO2; see Chapter 20) and to administer vasoactive drugs. Note, however, that central venous pressure may be a very misleading measure of preload in patients with acute heart failure (see Chapter 8). A PAC is not indicated routinely but should be considered in patients who do not respond in predictable ways to standard treatment.7 In the absence of a central venous catheter, inodilator therapy (e.g., dobutamine, milrinone) may be administered via a peripheral intravenous cannula.